27 February 2021: Articles 
Leg Compartment Syndrome Complicating Posterior Spinal Fusion for Adolescent Idiopathic Scoliosis: A Case Report
Unusual clinical course
Achraf Jardaly12ABDEF, Michael J. Conklin23CDEG, Shawn R. Gilbert23ADEFG*DOI: 10.12659/AJCR.927082
Am J Case Rep 2021; 22:e927082
Abstract
BACKGROUND: Lower-extremity compartment syndrome (CS) is a rare yet devastating complication of posterior spinal fusion. We present our case to discuss this occurrence and possible risk factors.
CASE REPORT: An obese 15-year-old boy with adolescent idiopathic scoliosis underwent posterior spinal instrumentation and fusion, which was complicated by loss of 5000 mL of blood. He received 11 946 mL of intraoperative infusions to maintain adequate perfusion. Throughout the procedure, his sensory and motor evoked potentials (EPs) were normal. On postoperative Day 1, the patient complained of mild anterior and lateral left leg pain, which became severe by Day 2. Physical examination revealed tense anterior and lateral compartments. He immediately underwent a fasciotomy with irrigation and debridement. On follow-up, the patient has regained full ankle range of motion and has 5/5 dorsiflexion and plantar flexion. He has a weak extensor hallucis longus (1/5) but has been able to fully participate in sports.
CONCLUSIONS: CS should be suspected when a patient has significant postoperative pain in areas remote from the spine. Risk factors such as excessive blood loss, large volumes of infusion, obesity, prolonged operative time, and EPs can be contributory.
Keywords: Blood Loss, Surgical, Compartment Syndromes, Obesity, Scoliosis, Spinal Fusion, Adolescent, Kyphosis, Leg
Background
Adolescent idiopathic scoliosis is a common deformity, affecting 2% to 3% of the general population [1]. Large spine deformities are often corrected with surgery, which most commonly involves spinal fusion and instrumentation. Recognized complications of this procedure include blood loss, infection, and neurological injury [2]. A rare yet devastating complication is compartment syndrome (CS) [3]. It is poorly understood in this context and a delay in diagnosis can lead to a permanent deficit.
Most commonly, CS arises in the setting of fractures, crush injuries, or severe muscle bruising [3]. A less common cause is reperfusion of blood vessels following blocked circulation, such as during surgery or sleep, when an individual is unable to move his or her limbs. During spine surgery in particular, positioning, blood loss, and high volumes of intravenous resuscitation all can contribute to extravasation of blood into the limb compartments, leading to CS [4,5]. CS, in turn, can lead to motor power deficits, nerve damage, infection, and even amputation. Therefore, prompt recognition and emergent treatment of it are key. The aim of the present case report is to raise awareness about this clinically significant complication, which can arise after posterior fusion for adolescent idiopathic scoliosis, and to discuss possible etiologies of it.
Case Report
An obese 15-year-old boy presented for evaluation of scoliosis. His height was 180 cm, he weighed 94.3 kg, and his body mass index was 29, at the 97th percentile. He had a 59-degree left thoracic scoliosis. Adolescent idiopathic scoliosis was diagnosed and magnetic resonance imaging showed no spinal cord abnormalities. Because of the magnitude of the patient’s curve and the Risser stage 2 classification of ossification, surgery was planned.
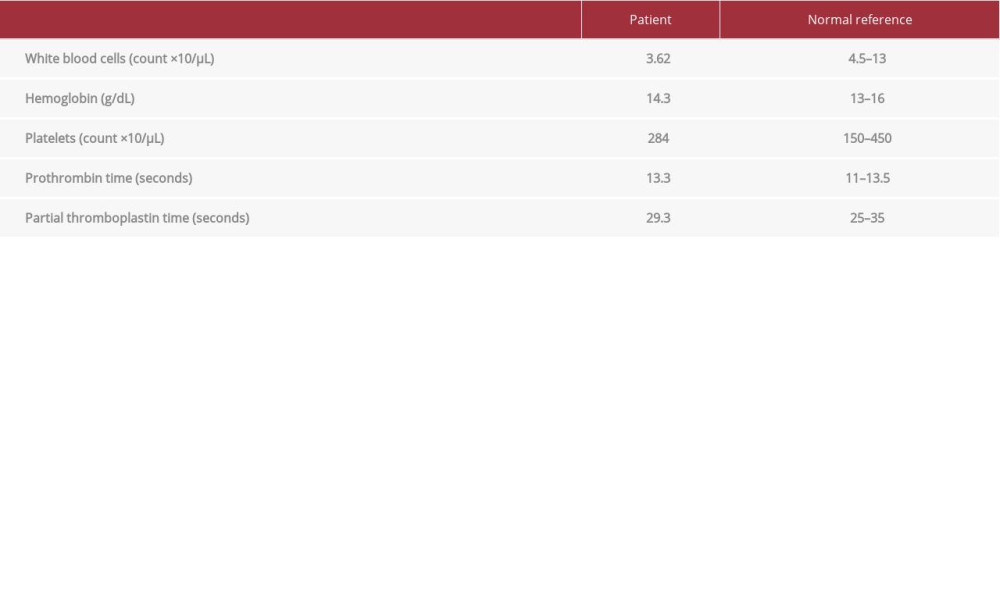
The patient underwent posterior spinal instrumentation and fusion. On admission, his vital signs were as follows: blood pressure 155/72 mmHg, heart rate 75 bpm, respiratory rate 14, oxygen saturation 98% on room air, and temperature 36.6°C. The patient was placed prone on a Jackson table frame. All pressure points were padded and pillows were placed under both of his legs. The surgery was complicated by a 5000-mL blood loss, 70.7% of the patient’s estimated blood volume, for which no cause could be identified. There was no personal or family history of bleeding. Preoperative prothrombin time (PT), partial thromboplastin time, and platelet levels all were normal (Table 1) and no known iatrogenic injury occurred. Intraoperatively, the patient received 2000 mL of lactated Ringer’s solution, 6600 mL of Plasma-Lyte, 1250 mL of cell saver, 1528 mL of packed red blood cells (pRBCs), and 568 mL of fresh frozen plasma (FFP), for a 11 946-mL total infusion. This volume was needed to maintain his blood pressure at 93/44 mmHg. The surgery lasted 6 h and the patient’s sensory and motor evoked potentials (EPs) were normal throughout the procedure.
The patient had an uneventful initial postoperative recovery. Of note is that his PT increased from 13.3 s preoperatively to 16.7 s postoperatively (normal range, 11–13.5 s). On postoperative Day 1, he complained of mild non-traumatic left leg pain, which became severe by Day 2. Physical examination revealed tense anterior and lateral compartments. The patient’s muscle strength and range of motion were normal. The pressures in his anterior and lateral compartments measured 58 and 41 mmHg, respectively. A 4-compartment fasciotomy of the leg was immediately performed. Intraoperatively, the compartments were found to be bulging and a hematoma was noted. A wound vac was placed for drainage. The patient underwent irrigation and debridement of nonviable tissue (portions of the anterior tibialis, extensor hallucis longus [EHL], and extensor digitorum longus) with delayed primary wound closure. He was discharged 9 days after fusion.
On follow-up, the patient demonstrated no spine problems. He has regained full ankle range of motion and has 5/5 dorsiflexion and plantar flexion. He has a weak EHL (1/5) but has been able to fully participate in sports.
Discussion
CS is a rare complication of procedures on the spine. It can arise in various locations, including the orbit, abdomen, and upper extremities, but the lower extremities are commonly involved [3,6–8]. Stotts et al reported on a case of medial foot CS following posterior spinal fusion for adolescent idiopathic scoliosis [8]. The few other case reports about CS following spine surgery all have involved adults. To the best of our knowledge, ours is the second reported case of CS following spinal fusion in an adolescent.
CS is one of the few true orthopedic emergencies. It occurs when compartmental pressure becomes elevated, decreasing tissue perfusion and leading to ischemia. It requires prompt treatment by fasciotomy to achieve tissue reperfusion and to prevent severe sequelae. There are several possible etiologies for CS in the setting of surgery on the spine. Positioning is regarded as a causative factor, particularly knee-chest position [7]. Because case reports exist of CS after supine positioning, however, other factors may be contributory [3,9,10]. Obesity is another potential cause, because excessive weight increases limb compression, and thus facilitates the development of CS [11]. Some authors attribute CS to intraoperative EP [3,11]. Muscle contraction due to stimulation in the face of pneumatic compression can lead to lower-extremity CS. While our patient underwent intraoperative monitoring, whether EPs are sufficient to cause CS is controversial. In addition, thigh and gluteal CS has been reported after surgery on the spine, and it is unlikely to be affected by monitoring of EP [5,11]. Therefore, an exploration of other potential causes is necessary.
Excessive blood loss can occur during surgery on the spine and it is likely that it was contributory in the present case. Male sex and increased surgical times are associated with high-volume blood loss [12]. Coupled with large infusion volumes, the result can be further bleeding and fluid shifts, both of which can cause CS [13]. Previous studies have shown that bleeding can lead to fluid overload in patients when a posterior approach is used for surgery on the spine [14]. Furthermore, with massive blood loss, clotting factors and calcium become depleted. Blood can extravasate and build up within compartments. A resulting hematoma ensues, leading to elevated compartment pressures. Therefore, it is prudent to assess bleeding intraoperatively and to try to reduce it and transfusion volumes. Using a cell saver can reduce the amount of transfused RBCs, but, like fluids, it also depletes coagulation factors. One unit of FFP is recommended for every 1000 mL of returned blood [15]. Fibrinogen is often the first factor depleted and FFP alone may not achieve target fibrinogen concentrations, so fibrinogen concentrates also can be considered [16]. In addition, antifibrinolytics can be used to reduce blood loss and need for transfusions. Loss of less blood alone should decrease fluid expansion within tissue compartments. This also helps control transfusion volumes, which maintains a patient’s hemostatic regulatory mechanisms and minimizes coagulopathy and bleeding within the compartments.
In the absence of trauma to our patient’s leg and in light of his aforementioned risk factors, multiple factors together appear to have caused CS in the present case. The patient was obese and experienced excessive blood loss and subsequent dilution of clotting from resuscitation. No cause for his severe bleeding was identified and he received the infusion volume necessary to replace the fluid lost (eg, lactated Ringer’s solution, Plasma-Lyte, a cell saver, pRBCs, and FFP). Blood loss was monitored intraoperatively by observing the suction volumes and the patient’s systolic blood pressure was monitored and kept above 90 mmHg to maintain adequate tissue perfusion. The use of intraoperative EP, which is routine during our surgeries on the spine, also could have contributed to this occurrence. Among all the risk factors, severe blood loss and large infusion volumes are potentially modifiable. As discussed earlier, antifibrinolytics can decrease bleeding during surgery on the spine and supplementing infusions with adequate FFP and fibrinogen can help prevent coagulopathy from infusions.
We are reporting our experience to encourage other surgeons to exercise heightened vigilance in similar cases. Our patient had initial pain on postoperative Day 1 but no investigations were undertaken and or interventions employed until the next day. Increased awareness of the possibility of CS and earlier discovery could have averted the need for debridement and prevented weakening of the patient’s EHL. Prompt recognition of CS minimized the clinical sequelae in the present case. A further delay in diagnosis or treatment would have resulted in muscle damage, and ultimately, significant loss of function or amputation. Patients with CS after surgery on the spine have been reported to develop adverse outcomes, such as weakness and foot drop [3]. Therefore, it is important to maintain a high index of suspicion for CS, particularly because initial pain can be masked by procedural and postprocedural analgesia.
Conclusions
Because CS is a rare complication after surgery on the spine, it can be missed. To achieve early diagnosis and prevent severe sequelae, it should be suspected when a patient has significant postoperative pain in areas remote from the spine. Risk factors such as excessive blood loss, large volumes of infusion, obesity, prolonged operative time, and EPs can be contributory.
References:
1.. Weinstein SL, The natural history of adolescent idiopathic scoliosis: J Pediatr Orthop, 2019; 39(6, Suppl 1); S44-46
2.. Sethi R, Buchlak QD, Yanamadala V, A systematic multidisciplinary initiative for reducing the risk of complications in adult scoliosis surgery: J Neurosurg Spine, 2017; 26; 744-50
3.. Divani KG, O’Brien A, Molloy S, A multicentre retrospective review of muscle necrosis of the leg following spinal surgery with motor evoked potential monitoring: A cause for concern?: Eur Spine J, 2016; 25; 801-6
4.. Aschoff A, Steiner-Milz H, Steiner HH, Lower limb compartment syndrome following lumbar discectomy in the knee-chest position: Neurosurg Rev, 1990; 13; 155-59
5.. Rudolph T, Løkebø JE, Bilateral gluteal compartment syndrome and severe rhabdomyolysis after lumbar spine surgery: Eur Spine J, 2011; 20; S180-82
6.. Boniello A, Verma K, Sees JP, Delayed abdominal compartment syndrome as a complication of spinal surgery: Literature review and case report: Spine Deform, 2016; 1; 464-67
7.. Bronson WH, Forsh D, Qureshi SA, Evolving compartment syndrome detected by loss of somatosensory- and motor-evoked potential signals during cervical spine surgery: Orthopedics, 2012; 35; e1453-56
8.. Stotts AK, Carroll KL, Schafer PG, Medial compartment syndrome of the foot: An unusual complication of spine surgery: Spine, 2003; 28; 118-20
9.. Dahab R, Barrett C, Pillay R, Anterior thigh compartment syndrome after prone positioning for lumbosacral fixation: Eur Spine J, 2012; 21; S554-56
10.. Magaji SA, Debnath UK, Mehdian HS, Compartment syndrome of the leg following total lumbar disc replacement via anterior retroperitoneal approach. A rare complication of anterior spinal surgery: Spine, 2010; 35; E74-76
11.. Mizuno J, Takahashi T, Male sex, height, weight, and body mass index can increase external pressure to calf region using knee-crutch-type leg holder system in lithotomy position: Ther Clin Risk Manag, 2016; 12; 305-12
12.. Alamanda VK, Massengill DL, Rozario N, Blood loss trends and financial implications in adolescent idiopathic scoliosis: Clin Spine Surg, 2018; 31(8); E418-21
13.. Norberg A, Brauer KI, Prough DS, Volume turnover kinetics of fluid shifts after hemorrhage, fluid infusion, and the combination of hemorrhage and fluid infusion in sheep: Anesthesiology, 2005; 102; 985-94
14.. Mac-Thiong JM, Asghar J, Parent S, Posterior convex release and interbody fusion for thoracic scoliosis: Technical note: J Neurosurg Spine, 2016; 25(3); 357-65
15.. Liumbruno G, Bennardello F, Lattanzio A, Recommendations for the transfusion of plasma and platelets: Blood Transfus, 2009; 7; 132-50
16.. Theusinger OM, Spahn DR, Perioperative blood conservation strategies for major spine surgery: Best Pract Res Clin Anaesthesiol, 2016; 30; 41-52
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250