11 December 2020: Articles 
Novel Pathogenic Germline Variant of the Adenomatous Polyposis Coli (APC) Gene, p.S2627Gfs*12 Identified in a Mild Phenotype of APC-Associated Polyposis: A Case Report
Unusual clinical course
Diane R. Koeller1ABEF, Alison Schwartz1ABEF, Danielle K. Manning2BDE, Fei Dong23BD, Neal I. Lindeman23DE, Judy E. Garber134DE, Arezou A. Ghazani235ABDEF*DOI: 10.12659/AJCR.927293
Am J Case Rep 2020; 21:e927293
Abstract
BACKGROUND: The diagnoses of adenomatous polyposis coli (APC)-associated polyposis conditions are typically based on suggestive personal features and/or family history, and the identification of a pathogenic variant in the APC gene. However, with large-scale genome sequencing, it is now possible to identify pathogenic variants before or even without the presentation of the expected clinical features. This case describes a novel pathogenic APC variant.
CASE REPORT: We report the unexpected identification of a rare, pathogenic germline APC variant, p.S2627Gfs*12 in an 80-year-old man with a diagnosis of renal cell carcinoma, without any family history of APC-associated polyposis or personal history of colorectal cancer. After the identification of the APC variant, a review of the patient’s medical records showed a personal history of 15 adenomatous polyps over a decade ago, with no follow-up genetic testing at the time.
CONCLUSIONS: This novel APC variant has not been characterized to date. The presence of the APC-p.S2627Gfs*12 variant in this patient led to the recommendation of additional cascade genetic testing and surveillance measures for any family members who tested positive for this variant. This report highlights the broad spectrum of the APC-associated polyposis features, and a mild phenotype associated with the pathogenic APC p.S2627Gfs*12 variant.
Keywords: Adenomatous Polyposis Coli, Carcinoma, Renal Cell, Genes, APC, Adenomatous Polyposis Coli Protein, Aged, 80 and over, Germ Cells, Germ-Line Mutation, Phenotype
Background
The pathogenic germline variants in the adenomatous polyposis coli (APC) gene are associated with several APC-associated polyposis conditions. These conditions include familial adenomatous polyposis (FAP), attenuated FAP (AFAP), gastric adeno-carcinoma or proximal polyposis of the stomach (GAPPS) with polyps restricted to the proximal stomach [1,2], and more recently, gastric polyposis and desmoid FAP (GD-FAP) [3]. Genetic testing for the APC gene is performed for individuals with suggestive clinical features or a family history of APC-associated polyposis. However, the large-scale genome sequencing or multi-panel genetic platforms have changed this paradigm of genetic testing. Many studies have reported the presence of pathogenic alterations in cancer genes unrelated to the clinical indication in cancer patients [4]; and in some reports, these incidental findings have guided early intervention and clinical management [5]. The large-scale sequencing data have presented an opportunity for a re-evaluation of the observed penetrance of the specific genomic alterations for related disease in unbiased ascertainment cohorts [6]. The reporting of these cases is invaluable as it can provide valuable phenotypic and clinical information about these rare variants. Sharing this clinical and genotype information with the medical community will aid the clinical interpretation of these rare variants.
We report the incidental identification of a rare pathogenic germline variant, APC p.S2627Gfs*12 (ClinVar entry: SCV001211471) in an 80-year-old man undergoing broad multigene panel testing because of his personal history of renal cell carcinoma (RCC). There was no personal history of colorectal cancer or a diagnosis of APC-associated polyposis. After the discovery of the APC variant in the proband, it was revealed that he had a history of adenomatous polyps over a decade ago, with no follow-up genetic testing at the time. To our knowledge, this pathogenic APC variant is first reported by our group and has not been characterized in the literature. This report describes the mild phenotype associated with the APC p.S2627Gfs variant in this patient. This incidental finding was followed by a recommendation for cascade testing and appropriate surveillance measures for other family members with this variant.
Case Report
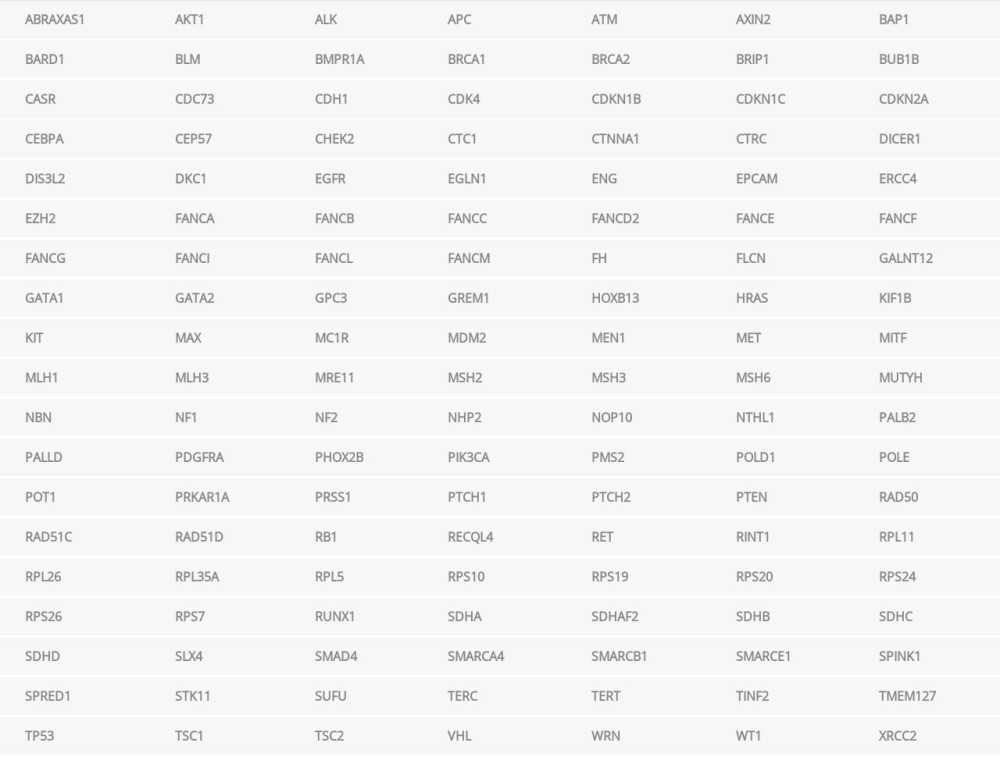
An 80-year-old man with a personal history of RCC consented to participate in the PROACTIVE study at the Dana-Farber Cancer Institute (DFCI) (Boston, Massachusetts, USA) in 2019. PROACTIVE is an institute-wide study that provides the option of germline testing for a hereditary cancer-gene panel of 133 genes (Table 1) (Invitae, San Francisco, CA, USA) as well as whole genome and whole transcriptome analyses for participants meeting the disease-specific eligibility criteria. The Genitourinary Division at the DFCI recruited kidney cancer patients of all subtypes. Before undergoing testing, the proband had a known 50% priori risk of carrying an ATM variant that had been identified in his son diagnosed with chronic myeloid leukemia at the age of 58 years. Germline testing in the pro-band was performed in a commercial laboratory (Invitae, San Francisco, CA, USA) according to published protocols [7,8]. The samples were enriched for targeted regions using a hybridization-based protocol, and sequenced using the Illumina NovaSeq 6000 platform (Illumina, San Diego, CA, USA). The enrichment and analysis were performed on the targeted coding sequences, 10 bp of flanking the intronic sequence (20 bp for BRCA 1/2), and other known causative genomic regions. The exon-level deletions and duplications were analyzed by comparing the read depth for each target sequence with both, mean read depth and read-depth distribution obtained from a set of clinical samples.
The germline report showed 3 pathogenic variants: APC p.S2627Gfs*12 (NM_000038.5: c.7879_7894del) (this variant from the present case was submitted to ClinVar by Invitae [San Francisco, CA, USA]; SCV001211471), ATM p.R1150Sfs*14 (NM_000051.3: c.3450_3454del), and MITF p.E318K (NM_000248.3: c.952G>A). The proband’s son was positive for the ATM variant, although he was negative for the APC and MITF variants. The proband’s late father reportedly had colorectal polyps of unknown origin; however, he had not been genetically evaluated. No family members have been diagnosed with FAP or AFAP. The patient’s maternal ancestry is Irish/Italian, and his maternal ancestry is German/English/Irish, with no known Ashkenazi Jewish ancestry or consanguinity (including the ancestry is routine practice in genetics) (Figure 1).
In 1994, at age 55, the proband had undergone a right radical nephrectomy. The histopathologic evaluation had revealed a clear-cell-type RCC of 3.3 cm (Fuhrman nuclear grade II of IV). The tumor was reportedly confined within the renal parenchyma. No vascular invasion by the tumor was identified, and the resection margins were tumor free (AJCC [American Joint Committee on Cancer] stage T2 N0 Mx).
The patient’s reports state that he had a confirmed history of 3 routine colonoscopies starting from 2004 at the age of 65 years. It is possible he had prior colonoscopies; however, the reports from these procedures were not available. The initial documented colonoscopy procedure with polypectomies revealed: 4 polyps in the transverse colon (3 at the level of the hepatic flexure), 1 sessile polyp (3 cm) and 2 additional polyps (each 8 mm) in the descending colon, 1 polyp (5 cm) at the junction of the sigmoid and descending colon, and 2 additional polyps in the descending colon that were treated with Endoclip. The cecum and rectum were reportedly within normal limits. A histological evaluation reported all the polyps to be tubular adenomas, except the one in the descending colon, which was a tubulovillous adenoma. A careful assessment of the family history and a risk evaluation for colorectal neoplasia were recommended. However, the patient was not genetically evaluated at that time.
Later in 2006, at age 67, he had a repeat colonoscopy. The histopathologic exam showed 2 tubular adenomas (5 mm each) in the transverse colon. The cecum, ascending, descending, and sigmoid colon were within normal limits. In 2013, at age 74, a colonoscopy identified 3 sessile polyps of varying sizes in the cecum (7 mm), transverse colon (7 mm) and the descending colon (8 mm). All these polyps were tubular adenomas. A repeat colonoscopy was recommended in 5 years. There are no reports of subsequent colonoscopy procedures. No genetic testing was performed at that time.
In 2013, at age 74, he presented with hematuria. The follow-up ultrasound was unremarkable; however, computed tomography and magnetic resonance imaging (MRI) showed suspicious abdominal masses. An upper endoscopic ultrasound with a fine-needle aspiration showed 3 round masses in the pancreatic head and body. The cytology report was positive for malignant cells consistent with his known RCC. The immunostaining showed that the tumor cells were positive for RCC, PAX8, AE1/AE3 and EMA (focal); and negative for CK7, synaptophysin, PDX1, and chromogranin. The microarchitecture in the tumor was similar to that seen in the known primary RCC. After this upper endoscopic ultrasound, he was followed up with an abdominal MRI in 2015, and an abdominal ultrasound in 2018. No gastric polyps or desmoid tumors were reported.
In 2015, a retroperitoneal lymph node biopsy showed a metastatic clear-cell-type RCC. In 2016, an OncoPanel (BWH Pathology, Boston, MA, USA) clinical test was performed on the deoxyribonucleic acid (DNA) extracted from the formalin-fixed, paraffin-embedded tissue obtained from a retroperitoneal lymph node biopsy of the metastatic RCC (estimated neo-plastic cells were 90%), according to the established protocol and methods [9–13]. OncoPanel (BWH Pathology, Boston, MA, USA) is a next-generation sequencing (NGS) test designed for the detection of single-nucleotide variants (SNVs), insertions and deletions (indels), copy number variants, and structural variants in tumor DNA containing at least 20% of tumor nuclei. The sample library was analyzed by massively parallel sequencing using a solution-phase Agilent-SureSelect hybrid capture kit (Agilent, Santa Clara, CA, USA) and an Illumina HiSeq 2500 9(Illumina, San Diego, CA, USA) sequencer. This assay interrogated the exonic sequences of 447 cancer-related genes, and 191 regions across 60 genes for rearrangements. Mutect1 and GATK (Broad Institute, Cambridge, MA, USA) tools were used to identify the SNVs and small indels; internally developed RobustCNV and BreaKmer (DFCI, Boston, MA, USA) tools were validated to detect copy number alterations and structural variants, respectively. The copy number detection was based on localized changes in the mapping depth of the sequenced reads in the baited regions. The copy number was calculated based on a robust linear regression against the panel of non-cancer samples with the same capture bait set. The copy number gains or losses were assigned using an adaptive calling method that adjusts the calling thresholds based on the post-normalization variability in each sample. The observed values were normalized against the predicted values and expressed as log2 ratios. A secondary normalization step removed the GC bias using a loess fit. The log2 ratios were centered on the diploid segments based on the allele fraction of the heterozygous single-nucleotide variants in the targeted panel. The assignment of gain, loss, or normal-copy calls for segments was performed using a sample-specific cut-off derived from the within-segment standard deviation of the post-normalized mapping depths, and the parameters in validation experiments.
The somatic OncoPanel (BWH Pathology, Boston, MA, USA) showed several alterations, notably a missense substitution VHL p.C162Y (NM_000551.3: c.485G>A) and other alterations in the 3p region including PBRM1 c.139-1G>C (NM_181042.4), and SETD2 c.7531_7533+5delAAGGTACT (NM_014159.6). The loss-of-function variants in these genes have been reported in RCC [14,15]. In addition, the somatic OncoPanel (BWH Pathology, Boston, MA, USA) showed multiple copy number changes, including a single-copy loss in 3p (Figure 2), a signature profile of clear-cell RCC, and a likely driver event in tumorigenesis [16]. The somatic profile was positive for a gain in 5q (Figure 2), often reported concurrently with the 3p loss in clear-cell RCC tumors [16]. The pathogenic ATM p.R1150Sfs*14 variant was present in 35% of the 243 reads. This ATM variant was later found to be a germline alteration after his son was found to be a carrier of this variant. The somatic Oncopanel (BWH Pathology, Boston, MA, USA) also showed a single-copy gain in the 16p region. The clinical significance of this alteration in this patient is not clear.
The patient died in 2019 at the age of 80 years. While he did not undergo AFAP-, ATM-, or MITF-related surveillance due to his then-recent genetic findings, any positive variants can have implications for the rest of his family. Therefore, cascade testing and appropriate surveillance measures were recommended for family members who tested positive for the APC and ATM variants. The patient and his family gave informed consent for the publication of this case report. All genetic testing was performed after approval from the institutional review board.
Discussion
The APC gene is located on chromosome 5 at 5q22.2 and encodes a tumor-suppressor protein involved in the negative regulation of Wnt signaling by degrading β-catenin. A loss of function of the APC results in the accumulation of β-catenin that in turn, leads to the constitutive activation of several proto-oncogenes including cyclinD1, c-myc, and CRD-BP [17], and ultimately, uncontrolled cell division [18]. The canonical transcript of the APC gene includes 8 known functional domains [17].
The pathogenic germline variants in the APC gene are implicated in the APC-associated polyposis conditions. The majority of the pathogenic germline APC variants are base-pair changes that lead to the production of truncated proteins [19]. The variants associated with severe phenotypes abolish the β-catenin-binding site on the protein (1256-2031aa) [17]. The β-catenin accumulation, in turn, predisposes the tissue to the development of colon tumors [20]. Generally, the bi-allelic loss of the APC function is a mechanism of tumorigenesis in colorectal cancer [17,21]. Depending on the location of the germline variant in APC, the second allele is sporadically mutated or exhibits allelic loss. In FAP, the likelihood that the tumor exhibits a loss of heterozygosity (LOH) is dependent on the location of the germline variant in the APC gene. Similar to the sporadic variants in colorectal cancer, the germline variants between codons 1194 and 1392 are associated with a higher frequency of LOH [22]. In contrast, the germline variants distal to codon 1392 of the APC protein show a significantly lower frequency of LOH [22].
The novel pathogenic germline APC c.7879_7894del, p.S2627Gfs*12 variant described herein, (ClinVar entry: SCV001211471) is a 16 base-pair deletion in the last exon of the APC gene, causing a frameshift at codon Ser2627. It is expected to disrupt the last 217 amino acids of the APC protein. The C-terminus of the protein contains EB1- and HDLG-binding sites involved in the negative regulation of microtubular migration [23]. To date, this variant is absent from the gnomAD dataset and has not been characterized in the published literature. There are no
The location of pathogenic variants in the APC gene is reportedly associated with the different clinical manifestations of APC-associated polyposis [3,25–27]. The pathogenic variants in the alternatively spliced regions of exon 9, most 5’-end (codons 1–177), most 3’-end, and distal to codon 1580 are associated with an attenuated polyposis phenotype [28]. Recently, distal variants in APC have been associated with the gastric polyposis and desmoid FAP (GD-FAP) phenotype [3]. The APC variant discussed in the present case is in the 3’region of the gene, at the 2627 residue that corresponds to the C-terminus region of the APC protein. Given its location and the patient’s phenotype, this variant is likely to be associated with AFAP not FAP. The AFAP is characterized by a milder course of the disease, and a later age of onset with fewer colorectal adenomatous polyps than observed in FAP. The AFAP patients typically present with 10– 100 polyps, with an average of 30 polyps [28,29]. In AFAP, the incidence of colorectal cancer sharply rises after the age of 40 years [29]. The cumulative colorectal cancer risk by 80 years of age is reportedly around 70% [29,30], with the mean age of cancer diagnosis at 50-55 years [31,32] and the mean age of polyp diagnosis at 44 years [32]. The colonic polyps are often proximal, with infrequent rectal involvement [33]. According to the National Comprehensive Cancer Network (NCCN) guidelines for Genetic/Familial High-Risk Assessment of Colorectal Cancer [29], AFAP is considered when >10 to <100 adenomas are present and an APC pathogenic variant is identified. Between 65 years to 74 years of age, the patient in the current case report collectively had 15 documented adenomatous polyps, which were all discovered during routine colonoscopies. Ten of the 15 polyps were reported in 2004, with no significant polyp burden in 9 years until the last documented colonoscopy. Furthermore, the polyps were in the hepatic flexure, transverse colon, descending colon, and 1 in the cecum. No polyp was reported in the ascending colon as typically reported in AFAP. There is no reported family member with a diagnosis of AFAP or a reported history of more than 10 colonic polyps. It is noteworthy that up to 30% of APC variants in FAP or AFAP are reportedly
In addition to the APC variant, this patient’s germline profile showed a heterozygous pathogenic variant in the MITF. The MITF is a member of the MYC supergene of transcription factors. The pathogenic MITF p.E318K variant in this patient is located in the conserved small-ubiquitin-like modifier consensus site. This variant reportedly increases the MITF transcriptional activity [35] that in turn, upregulates the hypoxia inducible factor in renal tumor-igenesis [36]. This variant has been observed in individuals with RCC and reported to be associated with an autosomal dominant predisposition to RCC [36,37]. While the presence of this variant increases the patient’s lifetime risk of developing RCC, the exact role of this germline MITF p.E318K variant in the tumorigenicity of this patient’s RCC requires further research.
The patient was also positive for a heterozygous pathogenic germline ATM variant, ATM p.R1150Sfs*14. The ATM variants are mainly associated with an increased risk for female breast cancer and pancreatic cancer. The current pancreatic cancer screening guidelines are heavily dependent on information from the family history. The identification of this ATM variant in the setting of the proband’s family history of pancreatic cancer indicates that any ATM-positive family members can benefit from the pancreatic screening. Due to his advanced disease, the germline finding did not alter the medical management for the proband. However, these findings have implications for the rest of the family. Cascade genetic testing and appropriate surveillance measures were recommended for family members who were positive for this variant. If the pro-band had only been offered single-site testing for the familial ATM variant, the APC and MITF gene variants would not have been identified, and his other children could have only been offered single-site or single-gene testing.
The somatic profile of the patient was obtained from a retroperitoneal lymph node biopsy of the clear-cell-type meta-static RCC. It showed a single-copy loss in 3p, and the somatic missense variants of VHL p.C162Y, PBRM1 c.139-1G>C, and SETD2 c.7531_7533+5delAAGGTACT. The loss-of-function variants in all these genes have been reported in RCC [14,15]. The pathogenic ATM-p.R1150Sfs*14 variant was present in 35% of the 243 reads. There was also a single-copy gain along chromosome 5 including the regions in 5q; a signature profile frequently observed concurrently with a 3p loss in the clear-cell RCC tumors [16]. A somatic copy number plot also showed a single-copy gain in the 16p region. The clinical significance of this alteration with respect to this patient’s RCC is not clear. An investigation of the somatic NGS data after the germline results were reported, identified the germline variants of MITF p.E318K and APC p.R1150Sfs. The APC variant was detected in 6 of the 373 reads below the calling threshold of the OncoPanel (BWH Pathology, Boston, MA, USA) testing.
Lastly, the somatic OncoPanel (BWH Pathology, Boston, MA, USA) profile did not show a bi-allelic loss of the APC function. In fact, the 5q22.2 region encompassing the normal APC allele showed a single-copy gain. It is possible that the extra copy of the normal APC mitigated the aberrant function of the truncated APC allele. This could explain the absence of the expected AFAP phenotype. The penetrance and expressivity of this rare APC variant are unknown. Further studies are needed to elucidate the exact functional consequence and degree of phenotype variability associated with this APC variant.
Conclusions
In summary, we present an unexpected incidental finding of a novel and rare APC variant, p.S2627Gfs*12, in a patient with clear-cell RCC without a diagnosis of APC-associated AFAP. Through advances in large-scale genetic testing, it is now possible to identify potential clinically actionable alterations before or without manifestation of the clinical phenotypes or syndromes. The publication of these cases is valuable, as contextualizing the phenotype-genotype correlation can aid the clinical interpretation of these rare variants. They also emphasize the need for larger studies in unbiased clinical cohorts to establish the penetrance of such novel variants. This case report highlights a mild phenotype associated with the pathogenic APC p.S2627Gfs*12 variant. It also underscores a broader spectrum of the phenotypes of a traditionally well-known APC-associated polyposis revealed through pan-cancer genetic panel testing.
Figures
References:
1.. Jasperson KW, Patel SG, Ahnen DJ: APC-Associated Polyposis Conditions; 1993-2020, GeneReviews® Seattle (WA), University of Washington Seattle
2.. Worthley DL, Phillips KD, Wayte N, Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS): A new autosomal dominant syndrome: Gut, 2012; 61(5); 774-79
3.. Disciglio V, Fasano C, Cariola F, Gastric polyposis and desmoid tumours as a new familial adenomatous polyposis clinical variant associated with APC mutation at the extreme 3’-end: J Med Genet, 2020; 57(5); 356-60
4.. Ghazani AA, Oliver NM, St Pierre JP, Assigning clinical meaning to somatic and germ-line whole-exome sequencing data in a prospective cancer precision medicine study: Genet Med, 2017; 19(7); 787-95
5.. Jamuar SS, Kuan JL, Brett M, Incidentalome from genomic sequencing: A barrier to personalized medicine?: EBioMedicine, 2016; 5; 211-16
6.. Loveday C, Josephs K, Chubb D, p.Val804Met, the most frequent pathogenic mutation in RET, confers a very low lifetime risk of medullary thyroid cancer: J Clin Endocrinol Metab, 2018; 103(11); 4275-82
7.. Desmond A, Kurian AW, Gabree M, Clinical actionability of multigene panel testing for hereditary breast and ovarian cancer risk assessment: JAMA Oncol, 2015; 1(7); 943-51
8.. Kurian AW, Hare EE, Mills MA, Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment: J Clin Oncol, 2014; 32(19); 2001-9
9.. Wagle N, Berger MF, Davis MJ, High-throughput detection of actionable genomic alterations in clinical tumor samples by targeted, massively parallel sequencing: Cancer Discov, 2012; 2(1); 82-93
10.. Abo RP, Ducar M, Garcia EP, BreaKmer: Detection of structural variation in targeted massively parallel sequencing data using kmers: Nucleic Acids Res, 2015; 43(3); e19
11.. Olshen AB, Venkatraman ES, Lucito R, Wigler M, Circular binary segmentation for the analysis of array-based DNA copy number data: Biostatistics, 2004; 5(4); 557-72
12.. Garcia EP, Minkovsky A, Jia Y, Validation of OncoPanel: A targeted next-generation sequencing assay for the detection of somatic variants in cancer: Arch Pathol Lab Med, 2017; 141(6); 751-58
13.. Sholl LM, Do K, Shivdasani P, Institutional implementation of clinical tumor profiling on an unselected cancer population: JCI Insight, 2016; 1(19); e87062
14.. Mitchell TJ, Rossi SH, Klatte T, Stewart GD, Genomics and clinical correlates of renal cell carcinoma: World J Urol, 2018; 36(12); 1899-911
15.. Bihr S, Ohashi R, Moore AL, Expression and mutation patterns of PBRM1, BAP1 and SETD2 mirror specific evolutionary subtypes in clear cell renal cell carcinoma: Neoplasia, 2019; 21(2); 247-56
16.. Mitchell TJ, Turajlic S, Rowan A, Timing the landmark events in the evolution of clear cell renal cell cancer: TRACERx renal: Cell, 2018; 173(3); 611-23 e17
17.. Kwong LN, Dove WF, APC and its modifiers in colon cancer: Adv Exp Med Biol, 2009; 656; 85-106
18.. Talseth-Palmer BA, The genetic basis of colonic adenomatous polyposis syndromes: Hered Cancer Clin Pract, 2017; 15; 5
19.. Cattaneo F, Molatore S, Mihalatos M, Heterogeneous molecular mechanisms underlie attenuated familial adenomatous polyposis: Genet Med, 2007; 9(12); 836-41
20.. Azzopardi D, Dallosso AR, Eliason K, Multiple rare nonsynonymous variants in the adenomatous polyposis coli gene predispose to colorectal adenomas: Cancer Res, 2008; 68(2); 358-63
21.. Sieber OM, Segditsas S, Knudsen AL, Disease severity and genetic pathways in attenuated familial adenomatous polyposis vary greatly but depend on the site of the germline mutation: Gut, 2006; 55(10); 1440-48
22.. Rowan AJ, Lamlum H, Ilyas M, APC mutations in sporadic colorectal tumors: A mutational “hotspot” and interdependence of the “two hits”: Proc Natl Acad Sci USA, 2000; 97(7); 3352-57
23.. Wen Y, Eng CH, Schmoranzer J, EB1 and APC bind to mDia to stabilize microtubules downstream of Rho and promote cell migration: Nat Cell Biol, 2004; 6(9); 820-30
24.. Richards S, Aziz N, Bale S, Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology: Genet Med, 2015; 17(5); 405-24
25.. Nieuwenhuis MH, Vasen HF, Correlations between mutation site in APC and phenotype of familial adenomatous polyposis (FAP): A review of the literature: Crit Rev Oncol Hematol, 2007; 61(2); 153-61
26.. Jarvinen HJ, Peltomaki P, The complex genotype-phenotype relationship in familial adenomatous polyposis: Eur J Gastroenterol Hepatol, 2004; 16(1); 5-8
27.. Brensinger JD, Laken SJ, Luce MC, Variable phenotype of familial adenomatous polyposis in pedigrees with 3’ mutation in the APC gene: Gut, 1998; 43(4); 548-52
28.. Soravia C, Berk T, Madlensky L, Genotype-phenotype correlations in attenuated adenomatous polyposis coli: Am J Hum Genet, 1998; 62(6); 1290-301
29.. Gupta S, Provenzale D, Llor X, NCCN guidelines insights: Genetic/familial high-risk assessment: Colorectal, Version 2.2019: J Natl Compr Canc Netw, 2019; 17(9); 1032-41
30.. Neklason DW, Stevens J, Boucher KM, American founder mutation for attenuated familial adenomatous polyposis: Clin Gastroenterol Hepatol, 2008; 6(1); 46-52
31.. Knudsen AL, Bisgaard ML, Bulow S, Attenuated familial adenomatous polyposis (AFAP): A review of the literature: Fam Cancer, 2003; 2(1); 43-55
32.. Hernegger GS, Moore HG, Guillem JG, Attenuated familial adenomatous polyposis: An evolving and poorly understood entity: Dis Colon Rectum, 2002; 45(1); 127-34 ; discussion 134–36
33.. Half E, Bercovich D, Rozen P, Familial adenomatous polyposis: Orphanet J Rare Dis, 2009; 4(1); 22
34.. Bisgaard ML, Fenger K, Bulow S, Familial adenomatous polyposis (FAP): Frequency, penetrance, and mutation rate: Hum Mutat, 1994; 3(2); 121-25
35.. Xie L, Zhang Y, Wu CL, Microphthalmia family of transcription factors associated renal cell carcinoma: Asian J Urol, 2019; 6(4); 312-20
36.. Bertolotto C, Lesueur F, Giuliano S, A SUMOylation-defective MITF germline mutation predisposes to melanoma and renal carcinoma: Nature, 2011; 480(7375); 94-98
37.. Ghiorzo P, Pastorino L, Queirolo P, Prevalence of the E318K MITF germ-line mutation in Italian melanoma patients: Associations with histological subtypes and family cancer history: Pigment Cell Melanoma Res, 2013; 26(2); 259-62
Figures
Tables
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250