23 February 2021: Articles 
A Low-Grade Appendiceal Mucinous Neoplasia and Neuroendocrine Appendiceal Collision Tumor: A Case Report and Review of the Literature
Rare coexistence of disease or pathology
Massimo Villa1AG, Daniele Sforza1ABCDEFG*, Leandro Siragusa2ABCDEFG, Andrea Martina Guida2BEFG, Matteo Ciancio Manuelli1AG, Brunella Maria Pirozzi2AG, Marco Pocci3CEG, Giampiero Palmieri3CDEF, Michele Grande1AFGDOI: 10.12659/AJCR.927876
Am J Case Rep 2021; 22:e927876
Abstract
BACKGROUND: Incidental appendiceal neoplasms account for 1–2% of appendectomies. Mucinous neoplasms and carcinoids are the most frequent lesions, with an incidence of 0.6% and 0.3–0.9%, respectively. Appendiceal collision tumors are extremely rare and result from the proliferation of 2 different cellular lines. This report describes a young woman with a collision tumor composed of a low-grade appendiceal mucinous neoplasia (LAMN) and an appendiceal neuroendocrine tumor (ANET).
CASE REPORT: A 31-year-old woman was admitted to our institution presenting with abdominal pain and dysuria. After ultrasound assessment of a dilated appendix with wall thickening and distension by anechogenic material, a diagnosis of acute appendicitis was made. The patient, after a period of antibiotic therapy and observation, underwent an urgent laparoscopic appendectomy due to worsening condition. Surprisingly, the histological exam revealed a Tis LAMN extending from the base of the appendix to the resection margins, and a T3 grade-1 ANET, chromogranin-A and synaptophysin-positive, with a Ki67 less than 1%. On the basis of histological examination and European Neuroendocrine Tumor Network guidelines, in light of the positive LAMN resection margin and ANET mesoappendiceal invasion, after multidisciplinary team discussion, an elective laparoscopic hemicolectomy was indicated. The patient is now in good condition following a regular 5-year follow-up.
CONCLUSIONS: A collision LAMN and ANET is an exceedingly rare condition. The heterogeneity of clinical presentation and lack of solid evidence seem to recommend a tailored management. Laparoscopy is a safe and useful tool in localized mass excision.
Keywords: Adenocarcinoma, Mucinous, Appendiceal Neoplasms, Carcinoma, Neuroendocrine, Appendectomy, appendicitis, Appendix, neuroendocrine tumors
Background
Primary appendiceal neoplasms are infrequent tumors, found in around 1–2% of all appendectomy specimens [1,2]. Most benign and malignant appendiceal neoplasms are discovered incidentally during appendectomy with preoperative diagnosis of appendicitis. Malignant appendiceal neoplasms can present with distant spread, peritoneal involvement, or direct invasion, although this is an uncommon presentation [1].
The most common clinical onset is acute appendicitis caused by appendicular luminal obstruction by the neoplastic mass. A carcinoid syndrome is rarer and is caused by vasoactive peptides produced by appendiceal neuroendocrine tumors (ANETs), while mucocele and pseudomyxoma peritonei are a typical finding of mucinous neoplasms [1].
Mucinous neoplasms and carcinoids are the most frequent benign and malignant appendiceal lesions, respectively found in 0.6% and 0.3–0.9% of appendectomy specimens [3].
Rarely, collision or combined neoplasms can occur. The former are the result of 2 distinct but adjacent neoplasms, without any transition zone, resulting from the proliferation of 2 different cellular lines (biclonal malignant transformation), while the latter are the result of a multidirectional differentiation of cells from a single tumor [4,5]. Since combined and collision tumors are exceptional cases, a consensus on their treatment has not yet been reached.
Here, we present the case of a 31-year-old woman undergoing laparoscopic appendectomy for assumed appendicitis and afterward, a laparoscopic right hemicolectomy for a collision low-grade appendiceal mucinous neoplasm (LAMN) and an ANET. In addition, a review of similar cases reported in the literature was performed.
Case Report
A 31-year-old woman presented at the emergency room of our institution with abdominal pain associated with dysuria. She had had 2 pregnancies, no comorbidities, and no previous history of surgery. Physical examination revealed a painful and tender abdomen, particularly in the right iliac fossa with local peritonism, a positive Blumberg’s sign, and no signs of bowel occlusion. The patient was afebrile and vitals were normal, as were blood sample tests that showed a slight neutrophilia with a normal white blood cell count. A pelvic ultrasound scan revealed a 5.5-cm-long appendix with wall thickening, without any surrounding free fluid, that was distended by an anechogenic material (Figure 1).
Our first-line treatment was conservative management with antibiotics (ceftriaxone and metronidazole) and analgesic therapy. Two days after admission, the patient’s condition worsened, with increasing C reactive protein and leukocytosis prompting an urgent laparoscopic appendectomy. Intraoperatively, the appendix was covered with fibrin, adherent to the right salpinx with concomitant cecal, uterine, and anterior rectal inflammation and reactive pelvic inflammation. Intraoperatively, there were no signs of appendiceal perforation or extracellular mucin. The postoperative course was regular and the patient was discharged in good condition on the fourth postoperative day.
Macroscopic specimen examination showed a 4-centimeter-long appendix, filled with a dense acellular mucoid fluid, with a 1.5-centimeter yellowish bulk on its tip. This was found to be a well-differentiated ANET that was chromogranin-A- and synaptophysin-positive, with a Ki67 of less than 1% (ANET-1, WHO 2010 guidelines), no perineural or lymphovascular infiltration, and full-thickness invasion extended to the periappendiceal fat tissue (pT3Nx). Surprisingly, the histopathological examination also revealed a synchronous Tis LAMN (Armed Forces Institute of Pathology (AFIP) 2017 and WHO 2010 guidelines) at the appendiceal base with total mucosal substitution and involved surgical margins (Figure 2).
Three months later, a complete colonoscopy showed no pathological findings and a staging abdominal contrast computed tomography (CT) scan revealed no pathological enhancements but some subcentimetric paraortic and interaortocaval nodes. After multidisciplinary team discussion of the case, a laparoscopic right hemicolectomy was planned as suggested by American Joint Committee on Cancer (AJCC) guidelines [6], since the resection margins were involved by the LAMN and the ANET was extended to the periappendiceal fat tissue. Intraoperatively, no further macroscopic lesions were seen, and a right hemicolectomy with a latero-lateral isoperistaltic ileocolic anastomosis was performed. At the histopathological examination, margins were negative as were the 6 lymph nodes retrieved. Extracellular mucinous fluid was found in the colic submucosal layer, surrounded by a fibrotic nodular area in the site of the previous resection.
After the surgical procedure and multidisciplinary team discussion, no further treatment was considered necessary, so the patient was referred to an oncologic specialist who scheduled a 5-year follow-up period. There was no sign of recurrence after 1 year.
Discussion
Since collision tumors are such rare entities, one hypothesis is that the blind-ended tubular structure of the appendix favors prolonged exposure to carcinogens, although a common agent able to promote both LAMN and ANET is still unknown [7].
There are other situations in which 2 concomitant appendiceal pathologies can occur, such as ANET and endometriosis. As with collision tumors, the incidence of this condition is extremely rare [8].
LAMNs are found in 0.6% of all appendectomies and account for around 20% of appendiceal neoplasms. Women are more often affected and the peak incidence is in the sixth decade of life. The usual clinical presentation is as a palpable mass or tenderness in the right iliac fossa [1]. LAMNs represent up to 73% of mucinous epithelial neoplasms. They are usually noninvasive and have a good prognosis, although up to 18% of cases present with peritoneal mucinous deposits or pseudo-mixoma peritonei. Their treatment depends on different neo-plastic features such as the grade of their cellular atypia, nodal involvement, and peritoneal spread, and LAMNs confined to the appendix mainly require only appendectomy. However, if nodes are involved or R0 resection is not achieved, a right hemicolectomy is required. In the case of peritoneal involvement, without extraperitoneal masses, patients should undergo cytoreductive surgery and hyperthermic intraperitoneal chemotherapy, while extraperitoneal metastatic disease is treated with the same regimens used for metastatic colorectal chemotherapy [3,9,10].
ANETs comprise approximately 30–80% of all appendiceal tumors [11] and are the most frequent among all kinds of NETs. Most of these neoplasms have an excellent prognosis, with a 5-year survival rate close to 100% in the lower tumor stages [12]. Usually detected intraoperatively or during histological examination after appendectomy, ANETs typically do not present with tumor-related symptomatology [11].
For well-differentiated ANETs between 1 and 2 cm, further treatment after appendectomy is still recommended. In our case, the negative prognostic factors of mesoappendiceal invasion and LAMN extension to the resection margin indicated a laparoscopic right hemicolectomy, which was carried out after multidisciplinary team discussion and patient consent.
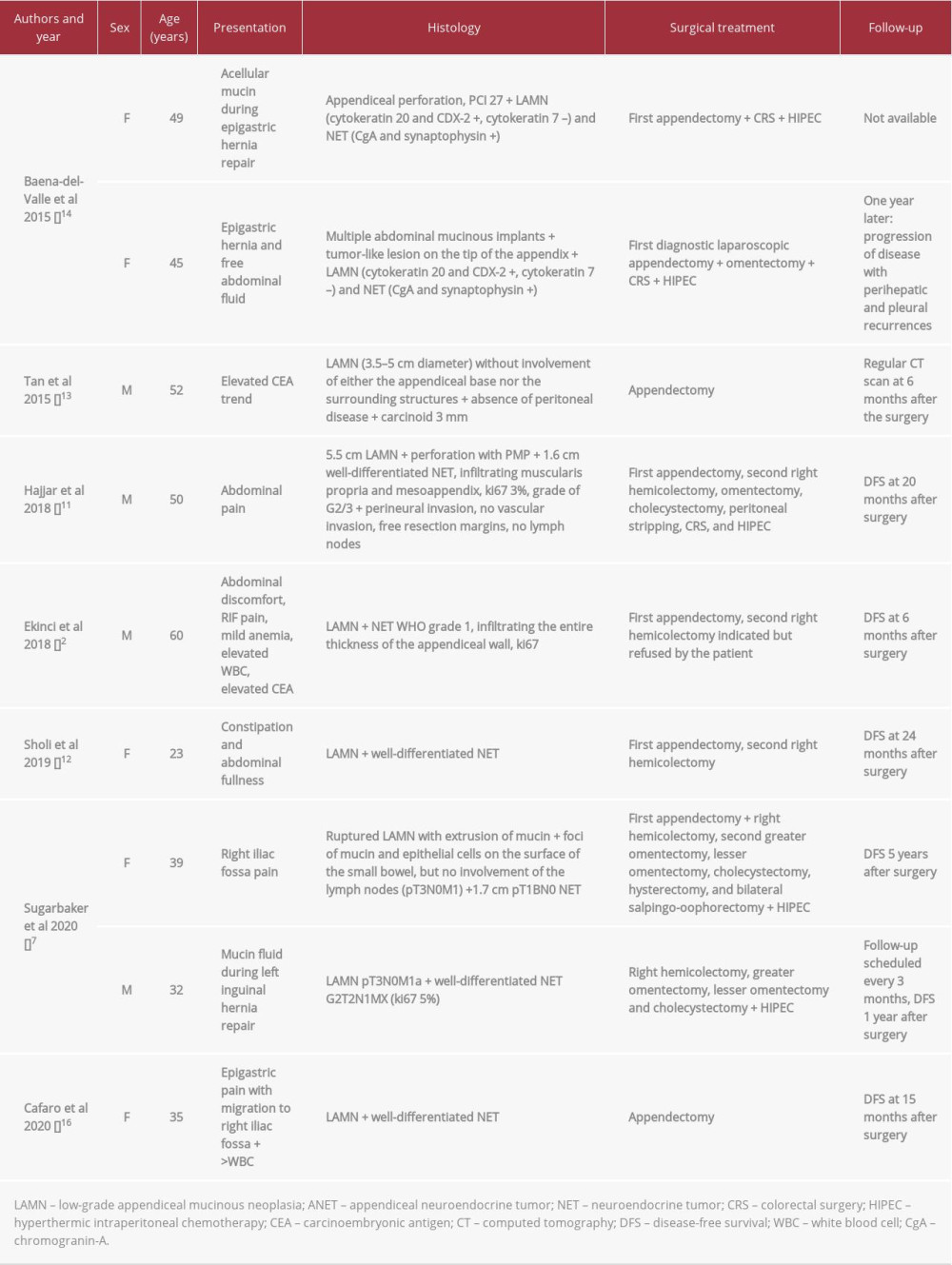
Retrospectively reviewing the literature, to the best of our knowledge, only 9 other cases of collision LAMN and ANET are reported in the literature (see Table 1) [2,7,13–17]. Of the cases reported, the patient age ranged between 23 and 60 years, with a mean age of 38.5 years and no significant differences in sex (6 female and 4 male). In none of these cases was preoperative workup able to diagnose both neoplasms: in 6 cases, the diagnosis was made postoperatively after appendectomy performed in an acute setting; in 3 cases, it was an incidental finding during surgery performed for other reasons; and in 1 case, a high level of carcinoembryonic antigen (CEA) prompted a diagnostic laparoscopy.
A pathognomonic ultrasound-scan sign for mucinous appendiceal neoplasms is the “onion-skin appearance” typical of mucocele. CT scan is furthermore able to detect mucocele as low-attenuated material filling the appendix, and is useful in detecting mucinous distant implants as low-attenuated deposits [18–20]. ANETs in CT scan appear like small submucosal masses or nodular wall thickenings and can eventually show calcifications; usually these lesions are difficult to visualize radiologically because of their small size, and are difficult to discriminate from appendicitis [21].
In 3 of the reported cases, the patients were simply treated with appendectomy; 2 cases further required a right hemicolectomy; and in the remaining 5 cases, peritoneal mucin invasion required extensive surgery and chemotherapy.
In our experience, in the case of localized presentation, the use of laparoscopy to perform second-step surgery is safe, feasible, and results in a faster postoperative recovery. The lack of a linear clinical pattern and the rarity of cases makes it difficult to trace a standard of care and follow-up. At this stage, management should be tailored to each patient, although a landmark seems to be whether the LAMN is disseminated. CEA and chromogranin-A could be useful tools to manage postoperative follow-up and check potential recidivism for LAMN and ANET, respectively [1].
Conclusions
The presence of a collision LAMN and ANET is exceedingly rare. Often diagnosed as an incidental finding after appendectomy, optimal management remains a challenge. We recommend tailoring the postoperative treatment and follow-up on a case-by-case basis, since solid evidence is lacking and clinical patterns differ greatly. In our case, laparoscopy has proven to be an excellent tool in performing appendectomy and right hemicolectomy for localized appendiceal collision neoplasms.
Figures
References:
1.. Leonards LM, Pahwa A, Patel MK, Neoplasms of the appendix: Pictorial review with clinical and pathologic correlation: Radiographics, 2017; 37(4); 1059-83
2.. Ekinci N, Gün E, Avcı A, Er A, Coexistence of low-grade mucinous neoplasm and carcinoid (collision tumor) within multiple appendiceal diverticula: A case report: Turk J Surg, 2018 [Online ahead of print]
3.. Smeenk RM, Van Velthuysen MLF, Verwaal VJ, Zoetmulder FAN, Appendiceal neoplasms and pseudomyxoma peritonei: A population based study: Eur J Surg Oncol, 2008; 34(2); 196-201
4.. Singh NG, Mannan AASR, Kahvic M, Nur AM, Mixed adenocarcinoma-carcinoid (collision tumor) of the appendix: Med Princ Pract, 2011; 20(4); 384-86
5.. Pecorella I, Memeo L, Ciardi A, Rotterdam H, An unusual case of colonic mixed adenoendocrine carcinoma: Collision versus composite tumor. A case report and review of the literature: Ann Diagn Pathol, 2007; 11(4); 285-90
6.. Amin MB, Greene FL, Edge SB, The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging: Cancer J Clin, 2017; 67(2); 93-99
7.. Sugarbaker PH, Ben-Yaacov A, Hazzan D, Nissan A, Synchronous primary neuroendocrine and mucinous epithelial tumors present in the same appendix. Case report of 2 patients: Int J Surg Case Rep, 2020(67); 76-79
8.. Parra RS, Feitosa MR, Biagi GBB, Neuroendocrine appendiceal tumor and endometriosis of the appendix: A case report: J Med Case Rep, 2020; 14(1); 152
9.. Carr NJ, Bibeau F, Bradley RF, The histopathological classification, diagnosis and differential diagnosis of mucinous appendiceal neoplasms, appendiceal adenocarcinomas and pseudomyxoma peritonei: Histopathology, 2017; 71(6); 847-58
10.. Moran B, Baratti D, Yan TD, Consensus statement on the loco-regional treatment of appendiceal mucinous neoplasms with peritoneal dissemination (pseudomyxoma peritonei): J Surg Oncol, 2008; 98(4); 277-82
11.. Pape UF, Niederle B, Costa F, ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (excluding goblet cell carcinomas): Neuroendocrinology, 2016; 103(2); 144-52
12.. Garcia-Carbonero R, Capdevila J, Crespo-Herrero G, Incidence, patterns of care and prognostic factors for outcome of gastroenteropancreatic neuroendocrine tumors (GEP-NETs):Results from the National Cancer Registry of Spain (RGETNE): Ann Oncol, 2010; 21(9); 1794-803
13.. Hajjar R, Dubé P, Mitchell A, Sidéris L, Combined mucinous and neuroendocrine tumours of the appendix managed with surgical cytoreduction and oxaliplatin-based hyperthermic intraperitoneal chemotherapy: Cureus, 2019; 11(1); 3894
14.. Sholi AN, Gray KD, Pomp A, Management and outcome of an appendiceal collision tumour composed of neuroendocrine and mucinous neoplasms: BMJ Case Rep, 2019; 12(7); e229414
15.. Tan HL, Tan GHC, Teo M, Two rare cases of appendiceal collision tumours involving an appendiceal mucinous neoplasm and carcinoid: BMJ Case Rep, 2016; 2016; bcr2015213938
16.. Baena-del-Valle J, Palau-Lázaro M, Mejía-Arango M, Well differentiated neuroendocrine tumor of the appendix and low-grade appendiceal mucinous neoplasm presenting as a collision tumor: Rev Esp Enferm Dig, 2015; 107(6); 396-97
17.. Caspi B, Cassif E, Auslender R, The onion skin sign: J Ultrasound Med, 2004; 23(1); 117-21
18.. Cafaro MA, Yaryura Montero JG, Bianco A, Appendiceal collision tumor. Mucinous epithelial neoplasm and neuroendocrine tumor: Rev Fac Cien Med Univ Nac Cordoba, 2020; 77(2); 113-16
19.. Wang H, Cheng Y, Wei R, Appendiceal mucocele: A diagnostic dilemma in differentiating malignant from benign lesions with CT: Am J Roentgenol, 2013; 201(4); W590-95
20.. Lim HK, Lee WJ, Kim SH, Primary mucinous cystadenocarcinoma of the appendix: CT findings: Am J Roentgenol, 1999; 173(4); 1071-74
21.. Pickhardt PJ, Levy AD, Rohrmann CA, Primary neoplasms of the appendix: Radiologic spectrum of disease with pathologic correlation: Radiographics, 2003; 23(3); 645-62
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250