09 April 2021: Articles 
False-Positive Nonstructural Protein 1 Antigen in a Patient with Philadelphia Chromosome-Positive Acute Lymphoblastic Leukemia: A Case Report with Literature Review
Mistake in diagnosis
Supat Chamnanchanunt12ABCDEFG*, Pravinwan Thungthong2ABDE, Asrinda Abdulkanan3BCE, Chajchawan Nakhakes2ACDFDOI: 10.12659/AJCR.928865
Am J Case Rep 2021; 22:e928865
Abstract
BACKGROUND: A rapid investigation of dengue viral infection is needed for physicians who manage patients with suspected dengue infection. The nonstructural protein 1 (NS1) test kit is commonly used to diagnose patients with acute febrile illness in dengue-endemic countries, although this test kit can yield false-positive results. The Dengue NS1 test kit mostly relies on cross-reaction among febrile illness patients with other viral infections rather than malignancies.
CASE REPORT: A 52-year-old male patient presented with 3 days of fever, intermittent gum bleeding, weight loss, and mucocutaneous bleeding. He was transferred to a second hospital with acute febrile illness. Both dengue NS1 antigen test kits were positive from the 2 hospitals where he was previously treated. Fever and cytopenia persisted, and then the dengue RT-PCR test was performed to establish the cause of illness. A peripheral blood smear was reviewed and showed blast cells. A bone marrow examination was done to test for the compatibility of lymphoblastic leukemia. The flow cytometry test showed B cells ALL with Philadelphia-positive chromosome. Finally, the result of the dengue RT-PCR test was negative.
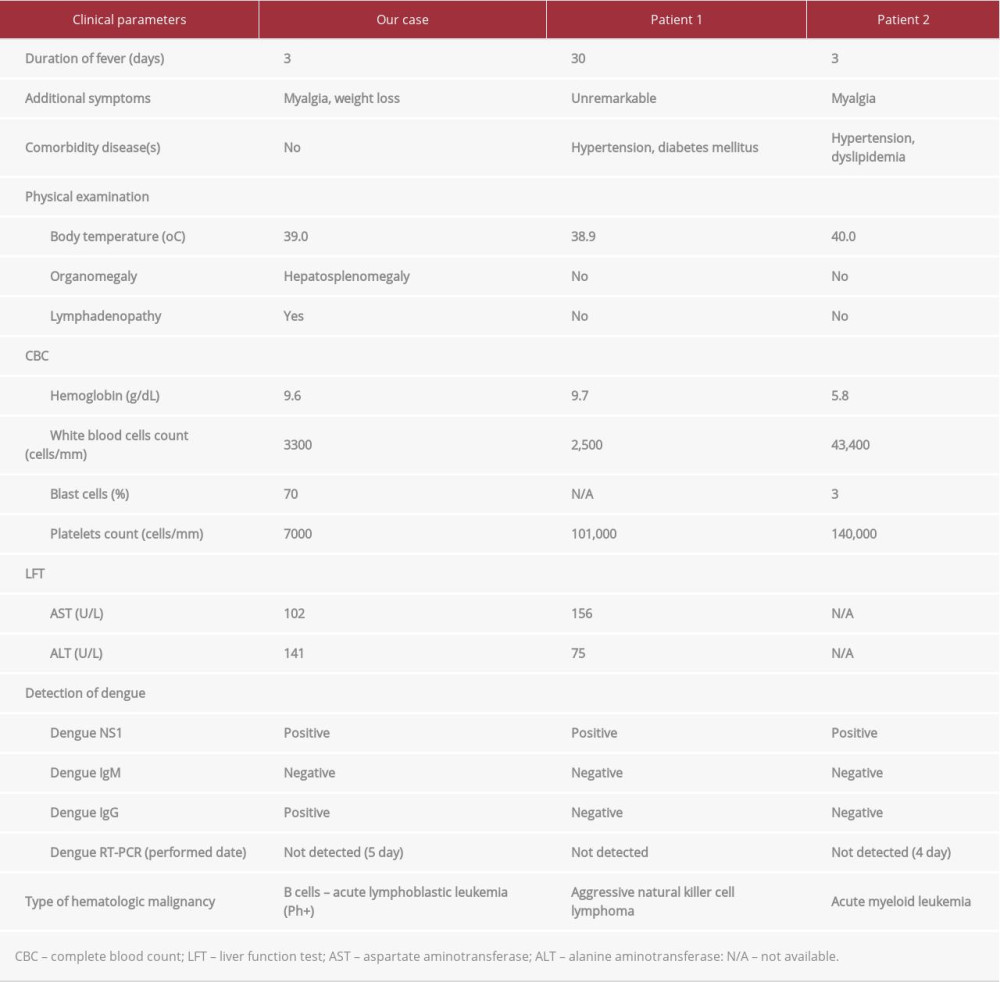
CONCLUSIONS: Our patient presented with fever and viral-like illness, but he was finally diagnosed with Ph+ ALL. We demonstrated the first case of false-positive dengue NS1 antigen in a Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL) patient. Moreover, we reviewed the literature to gather information on false-positive results using the dengue NS1 test kit. The dengue NS1 test kit is useful and produces reliable clinical findings, especially in patients with hematological malignancies.
Keywords: Dengue, False Positive Reactions, Philadelphia Chromosome, Precursor Cell Lymphoblastic Leukemia-Lymphoma, Viral Nonstructural Proteins, Dengue Virus, Enzyme-Linked Immunosorbent Assay, Sensitivity and Specificity
Background
Dengue is one of the tropical infectious diseases transmitted by mosquitoes. Its clinical presentation is an acute febrile illness with nonspecific organ involvement. Symptoms include fever, rash, arthralgia, and myalgia. Apart from the nonspecific symptoms, laboratory parameters (eg, leucopenia, increased atypical lymphocyte cells, and thrombocytopenia) can be used to assess the viral etiology [1]. The combination of clinical presentations and laboratory parameters may help physicians to distinguish between dengue infection and other conditions (eg, human immunodeficiency virus, septicemia, an autoimmune disorder, and hematological malignancies) [2,3]. The nonstructural protein 1 (NS1) antigen is a reliable diagnostic test kit for dengue infection, which showed sensitivity and specificity of 48.5–58.6% and 92.5–99.4%, respectively, and the positive predictive value was 88.5–99.3% [4–6]. The NS1 antigen structure is composed of a 46–55 kDa enigmatic protein. The NS1 antigen test for the diagnosis of dengue infection is more promising and widely accepted than the immunoglobulin M (IgM) test [7]. If the test result is positive, the patient is most likely diagnosed with dengue infection. The limitation of the NS1 antigen test is that it can produce either a false-negative result (the result depends on the day of testing) or a false-positive result (including cross-reactivity with other
Case Report
A 52-year-old male patient presented with a 3-day history of fever, rigor, myalgia, and intermittent gum bleeding. He lost 1 kg of weight during the illness. He had no known sick contacts and had no significant travel history before hospitalization. He denied comorbidities and previous dengue infection. During hospitalization in Malaysia, he had a high-grade fever (temperature, 39°C), and was normotensive with a blood pressure of 132/60 mmHg. Apart from pallor, the results of the physical examination were normal. His basic laboratory tests showed leucopenia (white blood count with 3600 cells/mm3), thrombocytopenia (platelets count=13 000 cells/mm3), and hemoglobin 12.4 g/dL. Evaluation of his liver enzymes revealed transaminitis (aspartate aminotransferase, 42 U/L; alanine transaminase, 274 U/L). The result of the dengue NS1 antigen test was positive through the use of the rapid dengue diagnosis kit SD BIOLINE Dengue Duo Combo test (Standard Diagnostics, Inc., South Korea), and the combined dengue IgM and immunoglobulin (IgG) antibodies tests were negative in the same specimen. A rapid HIV test and blood cultures for bacteria were performed, which showed negative results. The history of acute febrile illness and positive dengue NS1 antigen test positively led him to be diagnosed with dengue infection. The patient continued to have high-grade fever, continuous gum bleeding, and ecchymosis in both arms on the fifth day. One unit of platelet concentrate was transfused to improve his bleeding condition and raise his platelet level. He was classified as dengue hemorrhagic fever grade III with progressive disseminated intravascular coagulation (prothrombin time, 13.4 s; activated partial thromboplastin time, 12.4 s). He was referred to the Hospital for Tropical Diseases, Bangkok, Thailand and was tested using a commercially available rapid dengue diagnostic kit (Panbio, Standard Diagnostics, Inc., South Korea) in the second week. The dengue NS1 antigen and dengue IgG antibody results were positive, but the dengue IgM antibody test result was negative. Peripheral blood smears were reviewed and lymphoblastic leukemia cells (70% of blast cells) with low red blood cells and platelet count (Figure 1A–1C) were found. An urgent bone marrow study was performed to confirm the diagnosis of ALL (Figure 1D, 1E). Flow cytometry analysis of bone marrow showed 62.7% blasts and revealed an increased abnormal population in CD19, PAX5, CD10, CD34, HLA-DR, and PAX5; and negative for CD7, CD3, Cytoplasmic CD3, and MPO. Aberrant expression of CD33 was noted. These immunophenotype results were compatible with B cell ALL and the bone marrow showed a Philadelphia-positive chromosome. Finally, his test for dengue using a reverse transcriptase polymerase chain reaction (RT-PCR) showed a negative result. Chemotherapy was administered with a specific chemotherapy protocol for B cell ALL.
Discussion
This patient presented with viral-like fever and thrombocytopenia. The most common symptoms of dengue are fever and cytopenia, especially thrombocytopenia. In addition to assessing the clinical presentation and physical signs, we used the commercial screening laboratory test SD BIOLINE Dengue Duo test due to its high sensitivity and specificity [8]. The reliability of the dengue NS1 antigen test is ~90% [2,5,6]. This patient was previously repeatedly tested with the dengue NS1 test kit at 2 different hospitals. Two dengue NS1 test kit results were positive, but a peripheral blood smear showed a young lymphoid series. Thus, we questioned the result of the dengue NS1 test kit in this patient with febrile illness. The limitations of the test have been continuously reported in situations such as immune dysfunction, but some patients with hematological malignancies have cross-reactivity with the dengue NS1 antigen. Diagnosis must be carefully performed when there is a false-positive dengue NS1 antigen test result in a lymphoblastic leukemia patient. Cross-reactivity of the dengue NS1 antigen test was reported with other viral infections (
A false-positive dengue NS1 antigen test result can occur with other viral infections, but there are few reports on hematologic malignancy patients. Only 2 patients showed myeloid leukemia and lymphoma [9]. However, a false-positive dengue NS1 antigen test result has not been reported in a lymphoid leukemia patient. The false-positive dengue NS1 antigen test result may be due to a cross-activity with dengue-specific protein.
The dengue NS1 antigen is a specific enigmatic protein with a small molecular weight ranging from 46 to 55 kDa [12]. Cells in patients with hematologic malignancies rapidly proliferate and can produce a small-molecular-weight protein [13], and this protein may bind in a way similar to that in the dengue NS1 antigen test [9]. Hematologic malignancies can produce a large number of nonspecific proteins which can coat the NS1 antigen [3,14]. It is hypothesized that this is similar to false-positive results with the dengue test kit in patients with positive rheumatoid factor. Moreover, the Philadelphia chromosome may affect the enigmatic protein [15,16]. Nevertheless, physicians may be unable to distinguish between atypical lymphocyte and leukemic cells [17]. Our case showed only leukemic cells in the peripheral blood smear, which can also be rapidly diagnosed as a hematologic malignancy rather than a dengue infection. Clinical parameters and correct blood smear interpretation should be used to differentiate between dengue infection and conditions of hematologic malignancies. Thus, a peripheral blood smear was suitably used to fulfill the World Health Organization’s criteria for bedside testing and proper diagnosis in endemic areas for hematologic patients.
Conclusions
We report the first case of a false-positive NS1 test result in a Ph+ ALL patient. The dengue NS1 antigen test was repeated and persistently showing a false-positive result using diagnostic test kits from different companies. Use of appropriate clinical parameters is more useful than use of the highly specific NS1 test, especially in patients with hematologic malignancies. In dengue-endemic countries, hematologic patients with febrile illnesses may develop a cytopenia condition which overlaps dengue infection. Further research is needed to elucidate the mechanism involved in false-positive rapid dengue test results in febrile patients with hematologic malignancies.
References:
1.. Simmons CP, Farrar JJ, Nguyen VVC, Dengue: N Engl J Med, 2012; 366; 1423-32
2.. Andries AC, Duong V, Ngan C, Field evaluation and impact on clinical management of a rapid diagnostic kit that detects dengue NS1, IgM and IgG: PLoS Negl Trop Dis, 2012; 6; e1993
3.. Kamolratanakul S, Thungthong P, Nakhakes C, False-positive dengue IgM test result in a patient with systemic lupus erythematosus: a case report: Asian Biomed (Res Rev News), 2020; 14; 209-13
4.. Pok KY, Lai YL, Sng J, Ng LC, Evaluation of nonstructural 1 antigen assays for the diagnosis and surveillance of dengue in Singapore: Vector Borne Zoonotic Dis, 2010; 10; 1009-16
5.. Wang SM, Sekaran SD, Evaluation of a commercial SD dengue virus NS1 antigen capture enzyme-linked immunosorbent assay kit for early diagnosis of dengue virus infection: J Clin Microbiol, 2010; 48; 2793-97
6.. Blacksell SD, Jarman RG, Bailey MS, Evaluation of six commercial point-of-care tests for diagnosis of acute dengue infections: the need for combining NS1 antigen and IgM/IgG antibody detection to achieve acceptable levels of accuracy: Clin Vaccine Immunol, 2011; 18; 2095-101
7.. Fry SR, Meyer M, Semple MG, The diagnostic sensitivity of dengue rapid test assays is significantly enhanced by using a combined antigen and antibody testing approach: PLoS Negl Trop Dis, 2011; 5; e1199
8.. Gan VC, Tan LK, Lye DC, Diagnosing dengue at the point-of-care: utility of a rapid combined diagnostic kit in Singapore: PLoS One, 2014; 9; e90037
9.. Chung SJ, Krishnan PU, Leo YS, Two cases of false-positive dengue non-structural protein 1 (NS1) antigen in patients with hematological malignancies and a review of the literature on the use of NS1 for the detection of Dengue infection: Am J Trop Med Hyg, 2015; 92; 367-69
10.. Felix AC, Romano CM, Centrone C de C, Low sensitivity of NS1 protein tests evidenced during a dengue type 2 virus outbreak in Santos, Brazil, in 2010: Clin Vaccine Immunol, 2012; 19; 1972-76
11.. Colombo TE, Vedovello D, Araki CS, Dengue-4 false negative results by Panbio(R) Dengue Early ELISA assay in Brazil: J Clin Virol, 2013; 58; 710-12
12.. Muller DA, Young PR, The flavivirus NS1 protein: Molecular and structural biology, immunology, role in pathogenesis and application as a diagnostic biomarker: Antiviral Res, 2013; 98; 192-208
13.. Sheikh N, Abid R, Qureshi AW, Expression of low molecular weight proteins in patients with leukemia: West Indian Med J, 2012; 61; 235-39
14.. Jelinek T, Wastlhuber J, Proll S, Influence of rheumatoid factor on the specificity of a rapid immunochromatographic test for diagnosing dengue infection: Eur J Clin Microbiol Infect Dis, 2000; 19; 555-56
15.. Deininger MWN, Goldman JM, Melo JV, The molecular biology of chronic myeloid leukemia: Blood, 2000; 96; 3343-56
16.. Bernt K, Hunger S, Current concepts in pediatric philadelphia chromosome-positive acute lymphoblastic leukemia: Front Oncol, 2014; 4; 54
17.. Chamnanchanunt S, Thungthong P, Nakhakes C, Dengue virus infection in a patient with chronic myeloid leukemia: Southeast Asian J Trop Med Public Health, 2012; 43; 900-3
In Press
04 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.941835
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250