01 June 2021: Articles 
Blunt Abdominal Trauma Leading to an Incidental Finding of Duplicate Inferior Vena Cava (DIVC): A Case Report and Literature Review
Congenital defects / diseases
Mamoun Nabri1AEF*, Norah J. Alromaih1BEF, Sharifah A. Othman1BEF, Elham S. Alghusnah1BEF, Hossain Abu Al Ola2EF, Adel Elbagir1EF, Ayman O. Nasr1EFDOI: 10.12659/AJCR.929198
Am J Case Rep 2021; 22:e929198
Abstract
BACKGROUND: With a prevalence of about 2% to 3%, duplication is the most common anomaly associated with the inferior vena cava (IVC). In general, systemic venous anomalies are being more frequently diagnosed in asymptomatic patients. We report the case of a young man with an incidental finding of an asymptomatic duplicated IVC, along with a literature review.
CASE REPORT: A 36-year-old man was brought to our Emergency Department (ED) following a high-speed motor vehicle collision (MVC), reporting right flank and hip pain. Upon examination, the “seatbelt sign” was noticed, along with abrasions over his right side. He sustained a small-bowel mesenteric injury, for which he was admitted and was treated conservatively. A CT scan incidentally revealed a duplicate IVC (DIVC). He later underwent a laparotomy with limited right hemi-colectomy and was discharged home in good condition.
CONCLUSIONS: Undiscovered and asymptomatic DIVCs pose a potential risk to patients during clinical interventions. Advancements in diagnostic imaging contribute greatly to the incidental discoveries of inferior vena cava duplication.
Keywords: Congenital Abnormalities, Incidental Findings, Vena Cava, Inferior, Tomography, X-Ray Computed
Background
Between the 4th and 8th weeks of gestation, the IVC develops from primitive veins, including the post-cardinal, sub-cardinal, and supra-cardinal veins. During this timeframe, any developmental abnormalities, regressions, or anastomosis typically lead to anomalies in the IVC.
The most common anomaly of the IVC is its duplication, with a prevalence between 2% and 3%, [1] and the first report of a duplicate inferior vena cava was made by Lucas in 1916. Currently, systemic venous anomalies are more frequently found in asymptomatic patients due to the extensive use of cross-sectional imaging. Accurate recognition of systemic venous anomalies plays a significant role in the optimal functioning of surgical and other interventional procedures [2].
Here, we report the case of a young man with an incidental finding of asymptomatic DIVC.
Case Report
As the driver in a frontal impact motor vehicle collision, a 36-year-old man was brought to the ED by ambulance. The ATLS protocol was followed on arrival and the patient was found to be stable, with a GCS of 15. He reported right flank and hip pain, and upon examination, the ‘seatbelt sign’ was noticed, along with abrasions over his right side. Focused assessment with sonography for trauma (FAST) was negative, and a subsequent CT revealed bilateral pre-nephritic fat stranding in the abdomen along with mesenteric fat stranding (Figure 1A, 1B) and a small amount of free fluid in the right iliac fossa, increasing the possibility of a mesenteric injury. At this time, a duplicate inferior vena cava was also noted, which was not related to the patient’s presentation (Figure 2).
The patient was admitted for observation with conservative management and serial abdominal examinations. Despite reporting intermittent right lower-quadrant pain, he remained hemodynamically stable and was started on a liquid diet. On the 5th day after admission, his abdominal pain increased in severity and the CT was repeated (Figure 3), revealing interval thickening of ileal loops wall. A distal segment of the ileum lacked wall enhancement, in keeping with sub-segmental ischemia, and a distal ileal branch corresponding with the same segment was poorly opacified and irregular. There was a slight interval increase in the amount of free fluid, without a loculated collection and with no evidence of free air.
The patient underwent an urgent laparotomy that same day. Intra-operatively, we discovered a large amount of blood with an ischemic terminal ileum about 5 cm from the ileocecal valve. Hence, a limited right hemi-colectomy with primary anastomosis was performed (Figure 4A, 4B). Postoperatively, the course was uneventful, aside from a prolonged ileus that was managed conservatively. The patient was discharged home in good condition on the 13th postoperative day, and was followed up in the outpatient clinic.
Discussion
Complex processes occur in embryological development of the IVC during the 6th and 8th weeks of gestational age. This process has been described as a journey of development, regression, and anastomosis of 3 primitive pairs of veins: the posterior cardinal, sub-cardinal, and supra-cardinal veins [3].
Venous drainage from the body wall caudal to the heart is received by the posterior cardinal veins, while the vitelline vein joins right sub-cardinal vein, forming the hepatic segment of the IVC. This process accounts for the pre-renal IVC, during which the left sub-cardinal vein regresses completely.
Ultimately, 4 segments constitute the normal IVC: the hepatic segment arises from the right hepatic vein, the supra-renal segment arises from the right sub-cardinal vein, the renal segment arises from the right supra-sub-cardinal and post-sub-cardinal anastomoses, and the infra-renal segments arise from the right supra-cardinal anastomosis [2,4,5]. Persisting right and left supra-cardinal vein have been reported to result in the double IVC anomaly [1].
Morita et al classified DIVC according to the patterns of the interiliac communicating vein. Variations fall under 8 sub-types: type 1 has a normal iliac connection, type 2a is DIVC with no interiliac communication, type 2b is DIVC with an interiliac communication from left common iliac vein, type 2c is DIVC with an interiliac communication from right common iliac vein, type 2d is DIVC with an interiliac communication from left internal iliac vein, type 2e is DIVC with an interiliac communication from right internal iliac vein, type 3 is left IVC with symmetrical to normal iliac connection, and type 4 has no iliac connection in the case of absence of an infra-renal IVC [6]. The various types of IVC are illustrated in Figure 5.
Ang et al [7] and Chaijaroonkhanarak et al [8] reviewed 41 and 13 published articles respectively, of double IVC between 2000 and 2015. Ang et al’s review revealed 53 cases with a male predominance of 31 males to 21 females and 1 case of unknown sex according to the authors [7]. Chaijaroonkhanarak et al reported a total of 18 cases, with a 10: 8 male-to-female ratio [8].
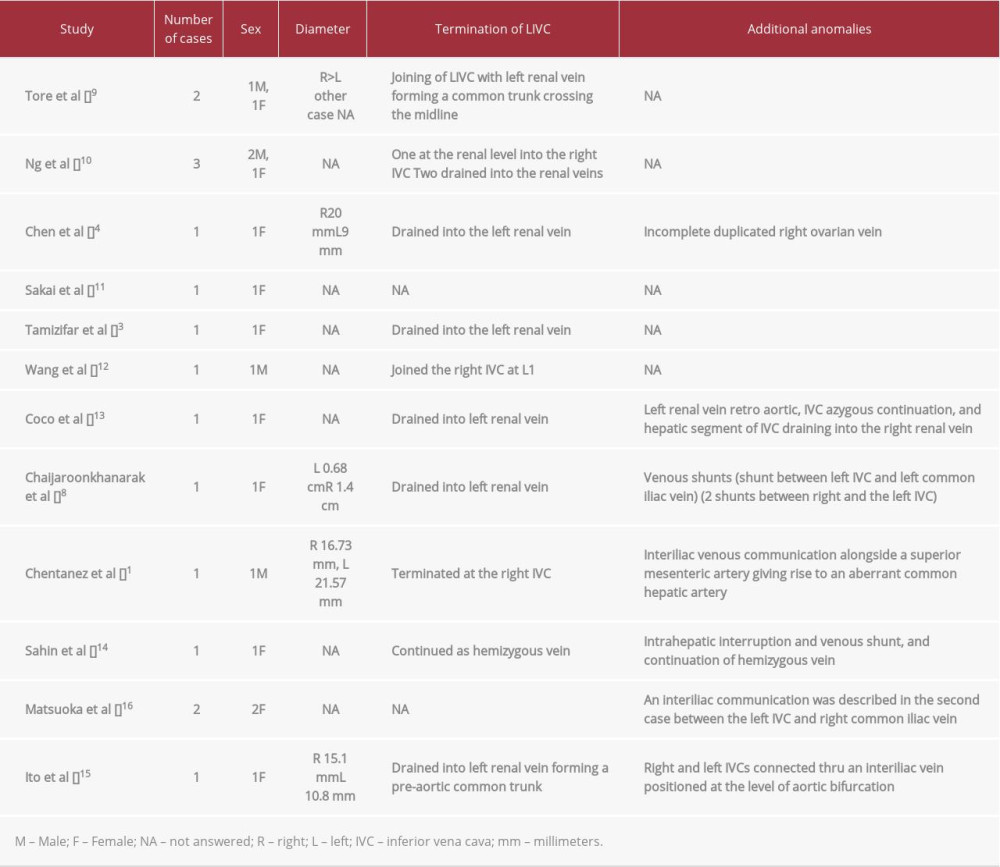
We discovered 13 published articles reporting 17 DIVC anomalies between 2004 and 2020, with a total of 6 male cases and 11 female cases (Table 1).
Tore et al [9], reported 2 cases (1 male and 1 female) that were incidentally found to have DIVC during CT imaging for chronic lumbar pain and abdominal pain, respectively. Ng et al [10] reported 3 cases in which a DIVC was found inadvertently through an MRI performed on 1 female and CTs on 2 males. Chen et al [4] reported a DIVC in a female cadaver. Sakai et al [11] documented a male case known to have polycystic kidney disease of the autosomal dominant type, who had a living donor kidney graft, which was discovered to have a DIVC during CT imaging. Tamizifar et al [3] reported the case of an 18-year-old female patient diagnosed with a deep vein thrombosis (DVT), who was discovered to have a DIVC through CT of the abdomen and CT angiography with i.v. contrast injection. Wang et al [12] recorded the case of 32-year-old male patient, also diagnosed with DVT, with a DIVC found on venography. Coco et al [13] reported 1 female case in which the DIVC was discovered through multi-detector CT.
In addition to the literature review, Chaijaroonkhanarak et al [8] reported 1 case of a DIVC in a female cadaver. Chentanez et al [1] reported a DIVC in a male cadaver. Sahin et al [14] reported a female case of DIVC incidentally discovered by CT. Ito et al [15] reported the DIVC in a female cadaver. Matsuoka et al [16] reported 2 cases of females with DIVCs discovered while undergoing retroperitoneal lymphadenectomy for advanced ovarian cancer. Most recently, Wasniewska et al [17] reported a female case of DIVC and nutcracker syndrome.
IN numerous reports over the past 2 decades, double IVC has consistently been recorded as an incidental finding. Nevertheless, pelvic vein anomalies such as DIVC have significant clinical consequences in both surgical and interventional procedures, and thus require correct interpretation of radiological imaging [15].
This accuracy is important, as historically, radiological imaging through axial CT has led to the misinterpretation of DIVC as either lymphadenopathy or ureteric dilation. Currently, the widespread use of multi-detector CT systems has rendered this issue of less importance [14].
As noted previously, early recognition of pelvic venous variations has serious clinical importance in retroperitoneal surgeries [10]. According to Matsuoka et al [16], patients known to have DIVC and interiliac veins should be managed with care during retroperitoneal lymphadenectomies in order to prevent major bleeding. Similarly, harvesting a kidney from a living donor with DIVC may create a challenge due to the renal vein length available for reconstruction techniques [11]. Kumar et al [18] reported the accidental finding of DIVC during a pacemaker implantation and described the difficulty created by the angles of the left and right IVCs, along with the decreasing caliber of the IVC. Furthermore, there have been suggestions that DIVCs require the implantation of more than 1 IVC filter for thrombi interruption [19]. Interestingly, the association between DIVC and venous thromboembolism has been reported in several case reports, highlighting a possible increased incidence of thrombosis formation [18].
Conclusions
With duplicate IVCs being almost always discovered incidentally during pre- or intra-procedural investigation or a postmortem examination, patients are potentially at risk due to this anomaly. Advancements in diagnostic imaging mitigate this risk by assisting in early identification.
Figures
References:
1.. Chentanez V, Nateniyom N, Huanmanop T, Agthong S, Co-existence of the double inferior vena cava with complex interiliac venous communication and aberrant common hepatic artery arising from superior mesenteric artery: A case report: Folia Morphol (Warsz), 2018; 77(1); 151-55
2.. Ghandour A, Partovi S, Karuppasamy K, Rajiah P, Congenital anomalies of the IVC-embryological perspective and clinical relevance: Cardiovasc Diagn Ther, 2016; 6(6); 482-92
3.. Tamizifar B, Seilani P, Zadeh MR, Duplication of the inferior vena cava and thrombosis: A rare case: J Res Med Sci, 2013; 18(10); 911-13
4.. Chen H, Emura S, Nagasaki S, Kubo KY, Double inferior vena cava with interiliac vein: A case report and literature review: Okajimas Folia Anat Jpn, 2012; 88(4); 147-51
5.. Bass JE, Redwine MD, Kramer LA, Spectrum of congenital anomalies of the inferior vena cava: Cross-sectional imaging findings: Radiographics, 2000; 20(3); 639-52
6.. Morita S, Higuchi M, Saito N, Mitsuhashi N, Pelvic venous variations in patients with congenital inferior vena cava anomalies: Classification with computed tomography: Acta Radiol, 2007; 48(9); 974-79
7.. Ang WC, Doyle T, Stringer MD, Left-sided and duplicate inferior vena cava: A case series and review: Clin Anat, 2013; 26(8); 990-1001
8.. Chaijaroonkhanarak W, Pannangrong W, Welbat JU, Double inferior vena cava with three shunts: A rare anomaly with important implications for surgeons: Folia Morphol (Warsz), 2017; 76(2); 307-11
9.. Tore HG, Tatar I, Celik HH, Two cases of inferior vena cava duplication with their CT findings and a review of the literature: Folia Morphol (Warsz), 2005; 64(1); 55-58
10.. Ng WT, Ng SS, Double inferior vena cava: A report of three cases: Singapore Med J, 2009; 50(6); 211-13
11.. Sakai H, Ide K, Ishiyama K, Renal vein extension using an autologous renal vein in a living donor with double inferior vena cava: A case report: Transplant Proc, 2012; 44(5); 1446-49
12.. Wang X, Chen Z, Cai Q, Catheter-directed thrombolysis for double inferior vena cava with deep venous thrombosis: A case report and literature review: Phlebology, 2014; 29(7); 480-83
13.. Coco D, Cecchini S, Leanza S, Inferior vena cava duplication: Incidental case in a young woman: Case Rep Radiol, 2016; 2016; 3071873
14.. Sahin H, Pekcevik Y, Aslaner R, Double inferior vena cava (IVC) with intrahepatic interruption, hemiazygos vein continuation, and intrahepatic venous shunt: Vasc Endovascular Surg, 2017; 51(1); 38-42
15.. Ito T, Ikeda Y, A case of double inferior vena cava with renal, ovarian and iliac vein variation: Anat Sci Int, 2018; 93(1); 139-43
16.. Matsuoka A, Tate S, Nishikimi K, Shozu M, Retroperitoneal lymphadenectomy for ovarian cancer with double inferior vena cava: Gynecol Oncol, 2018; 148(3); 632-33
17.. Waśniewska A, Ruzik K, Olewnik Ł, Unusual coexistence of double inferior vena cava with nutcracker syndrome – a case report and review of the literature: J Int Med Res, 2020; 48(2); 300060520904520
18.. Vasanth Kumar A, Anirudh Kumar A, An uncommon encounter during temporary pacemaker implantation – a double inferior vena cava: Indian Heart J, 2016; 68(Suppl. 2); S216-17
19.. Mano A, Tatsumi T, Sakai H, A case of deep venous thrombosis with a double inferior vena cava effectively treated by suprarenal filter implantation: Jpn Heart J, 2004; 45(6); 1063-69
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250