16 April 2021: Articles 
Septic Shock Caused by Bacteremia in an Immunocompetent Adult
Rare disease
Heidi A. Roeder1ABDEF, Benjamin Fuller2ABDEF, Sarah Scoular1ABDEF*DOI: 10.12659/AJCR.930888
Am J Case Rep 2021; 22:e930888
Abstract
BACKGROUND: Rahnella aquatilis is a facultatively anaerobic, gram-negative rod bacterium commonly found in freshwater. There are few cases of bacteremia caused by Rahnella aquatilis in the literature and even fewer cases reported of it causing sepsis in immunocompetent individuals. In this case report, we present a rare case of an immunocompetent individual who developed sepsis secondary to bacteremia caused by Rahnella aquatilis.
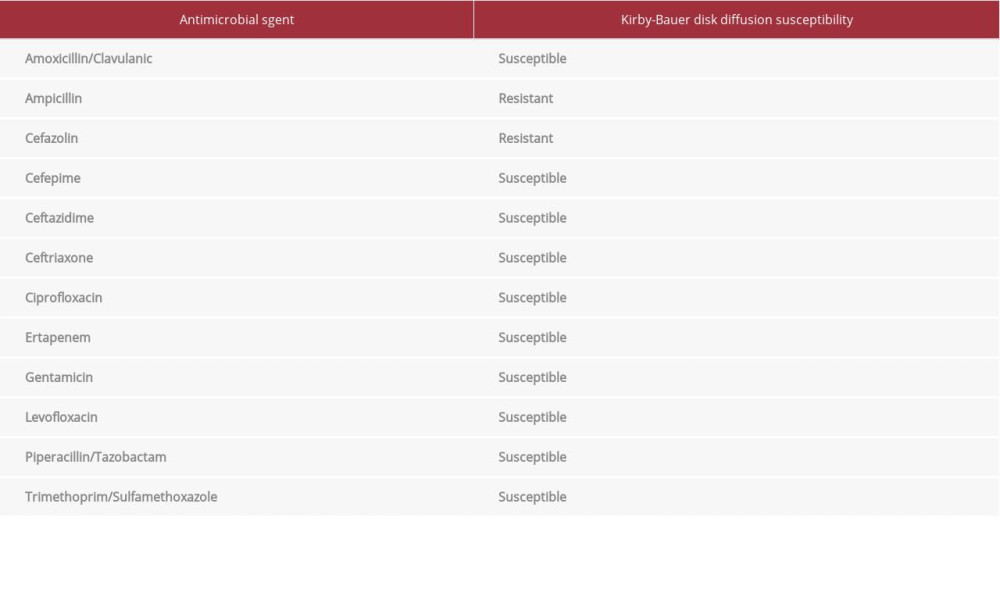
CASE REPORT: A 37-year-old immunocompetent man with cerebral palsy and chronic enterocutaneous fistulas, with an indwelling peripherally inserted central catheter (PICC) line for total parenteral nutrition (TPN), presented to the emergency department with complaints of increased enteric drainage from his fistula, rigors, and subjective fevers following a mechanical fall, which occurred approximately 1 week before. The day following admission, the patient developed septic shock and was transferred to the intensive care unit for vasopressor support. He was given intravenous cefepime and metronidazole for empiric therapy. Blood cultures grew Rahnella aquatilis, and antibiotic therapy was de-escalated to monotherapy with intravenous ceftriaxone. The patient’s condition stabilized, his PICC line was replaced, and he was successfully discharged, and continued on outpatient antibiotic therapy with ceftriaxone.
CONCLUSIONS: This case report represents a novel presentation of septic shock secondary to bacteremia caused by a gram-negative rod bacterium, Rahnella aquatilis, in an immunocompetent host dependent on TPN via a PICC line. This case also demonstrates that Rahnella aquatilis can be susceptible to and treated successfully with intravenous ceftriaxone. Bacteremia caused by Rahnella aquatilis can cause a swift, aggressive decompensation and should be treated with antibiotics immediately.
Keywords: Bacteremia, Gram-Negative Anaerobic Bacteria, Gram-Negative Bacterial Infections, Rahnella, Sepsis, Shock, Anti-Bacterial Agents, Cerebral Palsy, Immunocompetence, Shock, Septic
Background
Case Report
A 37-year-old immunocompetent man with cerebral palsy, multiple enterocutaneous fistulas secondary to a perforated appendix, which occurred 20 years prior, and a previous right atrial thrombus treated by anticoagulation therapy presented to the emergency department with his caregiver with complaints of increased enteric drainage from his enterocutaneous fistula, occasional rigors, and waxing and waning subjective fevers following a mechanical fall, which occurred approximately 1 week prior. It is important to note that the patient had a long-term, indwelling, peripherally inserted central catheter (PICC) line for total parenteral nutrition (TPN). Prior to admission, the patient’s enterocutaneous fistula was healing well until he fell, causing it to open up, which produced increased output requiring ostomy appliance changes approximately 2 times per day. It was noted that his caregiver provided excellent wound care and there were no signs of infection involving the enterocutaneous fistula. Upon presentation to the emergency department, the patient was afebrile with a blood pressure of 98/60 mmHg, had a heart rate and respiratory rate within normal limits, and a serum creatinine of 1.88 mg/dL, from a baseline of 0.9 mg/dL. At this time, he met no criteria for systemic inflammatory response syndrome. He was admitted to the general medicine unit for further management of his increased enterocutaneous fistula drainage and acute kidney injury.
One day after admission, the patient had an elevated whole blood lactate level of 3.4 mmol/L. At this time, he had blood culture samples drawn from his PICC line and an additional peripheral site. He was given broad-spectrum intravenous (i.v.) antibiotics to empirically treat an infection, given his increasing lactate level. He received cefepime 2000 mg and metronidazole 500 mg i.v. At this time, he was not hypotensive; however, within an hour his lactate level increased to 5.5 mmol/L, and he became hypotensive, with a blood pressure of 91/50 mmHg, had an increased temperature of 39°C, an elevated heart rate of 120 beats per min, and a normal respiratory rate. Due to a new diagnosis of severe sepsis, the patient was started on i.v. fluids with normal saline for blood pressure support and was transferred to the medical intensive care unit (MICU) for a higher level of care. Linezolid 600 mg i.v. was added to his antibiotic regimen to further broaden gram-positive bacteria coverage. While in the MICU, he required vasopressor support with norepinephrine. After being incubated at 35°F (1.6°C) on MacConkey agar for 24 h, both sets of blood cultures grew lactose fermenting gram-negative rods. The linezolid was discontinued because there was no growth of gram-positive bacteria.
Given the possible etiology of the patient’s infection being his PICC line, it was removed, and he received his TPN through a radiologically inserted jejunostomy tube. He continued to receive cefepime and metronidazole, and at 36 h, via matrix-assisted laser desorption/ionization time-of-flight mass spec-trometry, his blood culture speciation identified >100 CFU/mL of
Discussion
Most cases of
The development of sepsis is a common and life-threatening complication that has been reported with enterocutaneous fistulas [14]. Since our patient had chronic enterocutaneous fistulas and sepsis, this was a possible causative route of infection. Our patient had a history of a fistula not healing fully, and when it was almost fully healed, he had a mechanical fall about 1 week prior to presenting to the emergency department. After this fall, his enterocutaneous fistula started to have increased drainage. It was reported that his caretaker was providing excellent wound care to the area of the fistula, and no signs of an infection were present at the fistula site. Despite good wound care, the inherent risk of having an open wound placed him at higher risk for bacterial infection.
The causative route of infection in our patient is ultimately unknown but was likely a central line-associated bloodstream infection due to his prolonged need for TPN via a PICC line. His blood culture drawn from his PICC line grew >100 000 CFU/mL of
Conclusions
This case report represents a novel presentation of septic shock secondary to bacteremia caused by a gram-negative rod bacterium,
References:
1.. Izard D, Gavini F, Trinel PA: Ann Microbiol (Paris), 1979; 130(2); 163-77
2.. Brenner DJ, Müller HE, Steigerwalt AG: Int J Syst Bacteriol, 1998; 48; 141-49 Pt: 1
3.. Park DS, Oh HW, Jeong WJ, A culture-based study of the bacterial communities within the guts of nine longicorn beetle species and their exo-enzyme producing properties for degrading xylan and pectin: J Microbiol, 2007; 45(5); 394-401
4.. Heulin T, Berge O, Mavingui P: Eur J Soil Biol, 1994; 30; 35-42
5.. Harrell LJ, Cameron ML, O’Hara CM: J Clin Microbiol, 1989; 27(7); 1671-72
6.. Tash K: J Clin Microbiol, 2005; 43(5); 2526-28
7.. Matsukura H, Katayama K, Kitano N: Pediatr Cardiol, 1996; 17(2); 108-11
8.. Farmer JJ, Davis BR, Hickman-Brenner FW, Biochemical identification of new species and biogroups of Enterobacteriaceae isolated from clinical specimens: J Clin Microbiol, 1985; 21(1); 46-76
9.. Hoppe JE, Herter M, Aleksic S: J Clin Microbiol, 1993; 31(7); 1911-12
10.. Chang CL, Jeong J, Shin JH: J Clin Microbiol, 1999; 37(12); 4161-62
11.. Caroff N, Chamoux C, Le Gallou F: Eur J Clin Microbiol Infect Dis, 1998; 17(5); 349-52
12.. Dissanaike S, Shelton M, Warner K, The risk for bloodstream infections is associated with increased parenteral caloric intake in patients receiving parenteral nutrition: Crit Care, 2007; 11(5); R114
13.. Yeung CY, Lee HC, Huang FY, Sepsis during total parenteral nutrition: Exploration of risk factors and determination of the effectiveness of peripherally inserted central venous catheters: Pediatr Infect Dis J, 1998; 17(2); 135-42
14.. Williams LJ, Zolfaghari S, Boushey RP, Complications of enterocutaneous fistulas and their management: Clin Colon Rectal Surg, 2010; 23(3); 209-20
15.. Alballaa SR, Hussain Qadri SM, Al-Furayh O: J Clin Microbiol, 1992; 30(11); 2948-50
16.. Cruz AT, Cazacu AC, Allen CH, Pantoea agglomerans, a plant pathogen causing human disease: J Clin Microbiol, 2007; 45(6); 1989-92
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250