23 October 2021: Articles 
Successful Elbow Flexion Reconstruction Using Latissimus Dorsi Muscle Transfer Following a Road Traffic Accident and Upper Limb Trauma
Unusual setting of medical care, Rare disease
Salem Mohammad Alshammari1BEF*, Abdulrahman Abdulaziz AlghamdiDOI: 10.12659/AJCR.933374
Am J Case Rep 2021; 22:e933374
Abstract
BACKGROUND: Several surgical procedures to restore elbow flexion have been reported in the literature. Multiple factors direct the selection of appropriate procedures for each patient, including hand dominance, neurovascular injury, and comorbidities. Traumatic damage to the anterior compartment of the arm is an indication for latissimus dorsi transfer, which can restore elbow flexion. Bipolar pedicled latissimus dorsi (LD) flap is a design used very rarely to simultaneously reconstruct biceps brachii soft-tissue defects and regain complete flexion function. We report the case of a 30-year-old man who underwent successful elbow flexion reconstruction using latissimus dorsi muscle transfer following a road traffic accident and upper limb trauma.
CASE REPORT: A 30-year-old man presented with acute compartment syndrome caused by a road traffic accident and impact trauma to the left arm. The surgical evaluation revealed proximal biceps tendons rapture; therefore, immediate repair and therapeutic fasciotomy were done. Subsequently, unsuccessful repair resulted in total necrosis of the biceps muscle, which necessitated debridement of the biceps muscle. Delayed reconstruction with an LD flap was successfully done after stabilization of the patient’s condition. The flap was harvested as free-pedicled, then modified into a tube-like shape to resemble the biceps muscle.
CONCLUSIONS: This report has shown that the surgical procedure of latissimus dorsi muscle transfer can successfully restore elbow function following upper limb trauma; however, preoperative planning and postoperative follow-up are crucial for functional reconstruction of the upper extremity. In addition, carefully selecting reconstructive surgery considering patient factors, degree of injury, and the institution’s capacity are essential factors in achieving optimal function restoration with minimal complications.
Keywords: Activities of Daily Living, Compartment Syndromes, Elbow Joint, Surgical Flaps, Superficial Back Muscles, case reports, Elbow, Upper Extremity, Accidents, Traffic, Humans, Male, Mammaplasty, Reconstructive Surgical Procedures
Background
The anatomy of the upper limb makes it one of the most challenging and complex structures in the human body [1]. Elbow flexion is an action directed by many muscles; the biceps brachii is responsible mainly for elbow flexion and supination of the forearm. The musculocutaneous nerve enervates the biceps brachii [1].
Elbow flexion loss can be debilitating and limit activities of daily living (ADL). Generally, many factors affect the performance of ADL, such as age, gender, hand dominance, and functional angle of a joint. Elbow flexion requires a higher flexion angle (≥135°) to perform half of the ADLs [2]. One of the main factors influencing a surgeon’s choice of surgical procedure is the degree of tissue injury. Several options for reconstruction and restoration of elbow flexions have been reported, such as pectoralis major transfer, Steindler flexorplasty, unipolar or bipolar transfer of latissimus dorsi, triceps to biceps transfer, pectoralis minor transfer, and sternocleidomastoid transfer [3].
Elbow flexion impairment can be due to brachial plexus injury, injury to the musculocutaneous nerve, and trauma or infection of the anterior compartment of the arm. Latissimus dorsi muscle transfer allows a surgeon to fabricate and design it for multiple applications. Zancolli has discussed the use of bipolar latissimus dorsi transfer and the advantage of achieving active flexion up to 120 degrees and better muscle power compared to other procedures [4].
Several authors emphasized the need for a multidisciplinary approach and case-by-case selection of the surgical procedure [5–7]. Preoperative assessment of the latissimus dorsi flap is not a routine practice. However, evaluating the muscle flap beforehand is crucial, as this muscle will replace soft-tissue defects and restore function [8]. A free gracilis flap has been used to restore the elbow flexion, receiving nerve innervation from either the intercostal or spinal accessory nerves [9].
There are no specific guidelines on how to restore the function of elbow flexion; it depends mainly on the etiology of the trauma and the diagnosis. However, similar surgical techniques were previously reported to manage varying presentations and degrees of tissue loss [8].
Traumatic damage to the anterior compartment of the arm is an indication for latissimus dorsi transfer, which can restore elbow flexion. Here, we present a case of a 30-year-old man who underwent successful elbow flexion reconstruction using latissimus dorsi muscle transfer following a road traffic accident and upper limb trauma.
Case Report
SURGICAL TECHNIQUE:
First, the muscle was located as part of preoperative planning. Then, the incision border was marked with an incorporated skin paddle to monitor the flap postoperatively. It was placed 10 cm distal to the axillary fold and was 4 cm wide. We began the procedure by positioning the patient in lateral decubitus position, making incisions as planned. During initial dissection, the flap was fixed to the underlining fascia to prevent shearing forces, and resting muscle tension was measured. Next, the muscle flap was mobilized, and the thoracodorsal pedicle was dissected and freely mobilized. Then, the flap was designed in a tubular shape and passed to the anterior arm. The proximal part of the flap was attached to the coracoid process, and the distal part was fixed to the bicipital tendon.
Discussion
We successfully used a latissimus dorsi flap to replace the volumetric loss of biceps muscle and to restore elbow flexion. There are multiple surgical techniques used to restore active elbow flexion. Functional transfer of the pectoralis muscle was used in war injuries, as described by Ghahremani et al [10]. Multiple modifications were implemented to reach the goal of restoring elbow flexion. The pectoralis major flap was combined with tensor fascia lata as an interposition graft [11]. Steindler flexorplasty, transferring the pronator-flexor muscles group, has also been assessed and revised with several modifications [12]. Triceps muscle transfer can be done without sacrificing elbow extension independence, which is achieved by transferring the long head of the triceps as a pedicled flap [13,14]. Free muscle transfer has been commonly used to reconstruct elbow flexion with brachial plexus injuries [15,16]. Since our patient had an intact brachial plexus and was a suitable candidate for LD flap, to avoid the complications of the free flap, free muscle transfer was not performed.
Upper arm injury and the loss of elbow flexion can be challenging to reconstruct back to the usual upper limb’s physiological function and for the patient to resume ADL. Latissimus dorsi flap was one of the first functional musculocutaneous tissue transfers used to restore upper extremity function, including elbow extension [17] and flexion [4]. In our patient, there was a substantial volumetric defect that needed coverage; therefore, the pedicled LD flap was a suitable choice to fill the defect site and a reliable muscle to handle elbow flexion movement. Furthermore, since this surgery was not designed as a free flap, it had a short recovery time with minimal possible complications compared to a free flap.
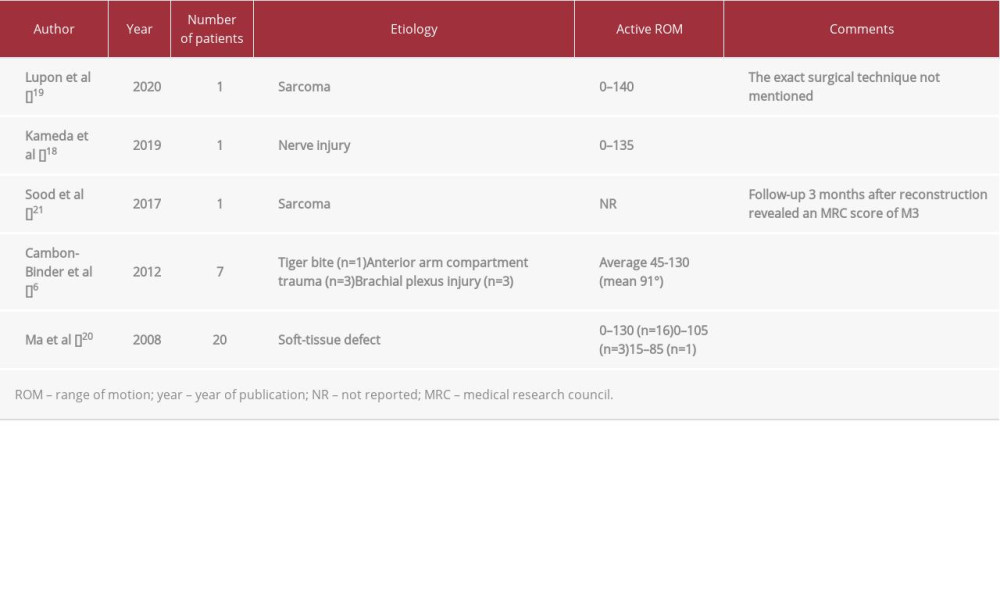
We reviewed recent cases in the literature with a similar surgical procedure. Etiologies and outcomes are summarized in Table 1 [6,18–21].
Since the development of this surgical technique, the outcomes have been variable, and it has been noted that preoperative assessment of the LD muscle plays a significant role in prognosis [22]. Many surgeons used this technique to restore elbow flexion, considering evaluating the LD muscle before surgery, and most of them reported a good result in active ROM [23,24]. Harvesting the flap with a skin paddle will allow for flap monitoring postoperatively [8].
One of the disadvantages of the LD flap is the risk of donor-site morbidity, including the possibility of developing functional impairment at the shoulder level [25]. However, it has been shown by prospective cohort studies that there is no significant difference between patients who underwent reconstruction with LD flap after mastectomy in comparison with mastectomy alone [26,27]. In addition, Ali et al reported that a combination technique of quilting and fibrin glue reduced the time for drains at the donor site and reduced the risk of seroma, hematoma, and infections [28]. After harvesting the LD flap, risk factors for seroma formation have been demonstrated by Gruber et al, including comorbidities, BMI, selective serotonin reuptake inhibitors (SSRIs), and surgical technique [29].
A bipolar pedicelled LD flap is useful when radiation or chemo-therapy was used in the recipient area [19] or if severe trauma with extensive soft-tissue defect was the main issue [8]. Furthermore, the LD flap is a reliable flap to reconstruct the upper extremity, including restoration of elbow flexion, if combined with good preoperative assessment, organized postoperative rehabilitation care, and regular follow-up [30].
Conclusions
Several surgical techniques are used to restore elbow flexion. This report shows that latissimus dorsi muscle transfer is a reliable option for restoring elbow flexion following upper limb trauma. For a better outcome, a complete preoperative assessment and a comprehensive postoperative rehabilitation program are fundamental. A multiprofessional approach and consideration of patient characteristics, including the degree of injury, are important in selecting an appropriate surgical procedure.
References:
1.. Forro SD, Munjal A, Lowe JB, Anatomy, shoulder and upper limb, arm structure and function: StatPearls, Treasure Island (FL), StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC.; 2021. https://www.ncbi.nlm.nih.gov/books/NBK507841/
2.. Oosterwijk AM, Nieuwenhuis MK, Schouten HJ, Rating scales for shoulder and elbow range of motion impairment: Call for a functional approach: PLoS One, 2018; 13(8); e0200710
3.. Loeffler BJ, Lewis DR, Restoration of elbow flexion: Hand Clinics, 2016; 32(3); 311-21
4.. Zancolli E, Mitre H, Latissimus dorsi transfer to restore elbow flexion. An appraisal of eight cases: J Bone Joint Surg Am, 1973; 55(6); 1265-75
5.. Al-Qattan MM, Elbow flexion reconstruction by Steindler flexorplasty in obstetric brachial plexus palsy: J Hand Surg Br, 2005; 30(4); 424-27
6.. Cambon-Binder A, Belkheyar Z, Elbow flexion restoration using pedicled latissimus dorsi transfer in seven cases: Chir Main, 2012; 31(6); 324-30
7.. Potter SM, Ferris SI, Reliability of functioning free muscle transfer and vascularized ulnar nerve grafting for elbow flexion in complete brachial plexus palsy: J Hand Surg Eur Vol, 2017; 42(7); 693-99
8.. Stevanovic MV, Cuéllar VG, Ghiassi A, Sharpe F, Single-stage reconstruction of elbow flexion associated with massive soft-tissue defect using the latissimus dorsi muscle bipolar rotational transfer: Plast Reconstr Surg Glob Open, 2016; 4(9); e1066
9.. Maldonado AA, Romero-Brufau S, Kircher RNM, Free functioning gracilis muscle transfer for elbow flexion reconstruction after traumatic adult brachial pan-plexus injury: Where is the optimal distal tendon attachment for elbow flexion?: Plast Reconstr Surg, 2017; 139(1); 128-36
10.. Ghahremani S, Nejad AA, Restoring elbow flexion by pectoralis major transplantation in war-injured patients: Microsurgery, 1996; 17(2); 97-101
11.. Beaton DE, Dumont A, Mackay MB, Richards RR, Steindler and pectoralis major flexorplasty: a comparative analysis: J Hand Surg Am, 1995; 20(5); 747-56
12.. Chen WS, Restoration of elbow flexion by modified Steindler flexorplasty: Int Orthop, 2000; 24(1); 43-46
13.. Gogola GR, Ezaki M, Oishi SN, Long head of the triceps muscle transfer for active elbow flexion in arthrogryposis: Tech Hand Up Extrem Surg, 2010; 14(2); 121-24
14.. Naidu S, Lim A, Poh LK, Kumar VP, Long head of the triceps transfer for elbow flexion: Plast Reconstr Surg, 2007; 119(3); 45e-47e
15.. Elzinga K, Zuo KJ, Olson JL, Double free gracilis muscle transfer after complete brachial plexus injury: First Canadian experience: Plast Surg (Oakv), 2014; 22(1); 26-29
16.. Yang Y, Yang JT, Fu G, Functioning free gracilis transfer to reconstruct elbow flexion and quality of life in global brachial plexus injured patients: Sci Rep, 2016; 6; 22479
17.. Harmon PH, Muscle transplantation for triceps palsy; The technique of utilizing the latissimus dorsi: J Bone Joint Surg Am, 1949; 31A(2); 409-12
18.. Kameda T, Soichi E, Yokota T, Konno SI, Restoration of elbow flexion with a pedicled latissimus dorsi myocutaneous flap to a brachial plexus injury at the terminal nerve level: Plast Reconstr Surg Glob Open, 2019; 7(10); e2472
19.. Lupon E, Chevreau C, Lellouch AG, Elbow flexion reconstruction after arm-sparing excision for high-grade triton sarcoma: A case report: J Med Case Rep, 2020; 14(1); 103
20.. Ma CH, Tu YK, Wu CH, Reconstruction of upper extremity large soft-tissue defects using pedicled latissimus dorsi muscle flaps – technique illustration and clinical outcomes: Injury, 2008; 39(Suppl. 4); 67-74
21.. Sood A, Therattil PJ, Russo G, Lee ES, Functional latissimus dorsi transfer for upper-extremity reconstruction: A case report and review of the literature: Eplasty, 2017; 17; e5
22.. Moneim MS, Omer GE, Latissimus dorsi muscle transfer for restoration of elbow flexion after brachial plexus disruption: J Hand Surg Am, 1986; 11(1); 135-39
23.. Azab AA, Alsabbahi MS, Bipolar transfer of latissimus dorsi myocutaneous flap for restoration of elbow flexion in late traumatic brachial plexus injury: Evaluation of 13 cases: Ann Plast Surg, 2017; 78(2); 198-201
24.. Kawamura K, Yajima H, Tomita Y, Restoration of elbow function with pedicled latissimus dorsi myocutaneous flap transfer: J Shoulder Elbow Surg, 2007; 16(1); 84-90
25.. Lee KT, Mun GH, A systematic review of functional donor-site morbidity after latissimus dorsi muscle transfer: Plast Reconstr Surg, 2014; 134(2); 303-14
26.. de Oliveira RR, do Nascimento SL, Derchain SF, Sarian LO, Immediate breast reconstruction with a Latissimus dorsi flap has no detrimental effects on shoulder motion or postsurgical complications up to 1 year after surgery: Plast Reconstr Surg, 2013; 131(5); 673e-80e
27.. de Oliveira RR, Pinto e Silva MP, Gurgel MS, Immediate breast reconstruction with transverse latissimus dorsi flap does not affect the short-term recovery of shoulder range of motion after mastectomy: Ann Plast Surg, 2010; 64(4); 402-8
28.. Ali SN, Gill P, Oikonomou D, Sterne GD, The combination of fibrin glue and quilting reduces drainage in the extended latissimus dorsi flap donor site: Plast Reconstr Surg, 2010; 125(6); 1615-19
29.. Gruber S, Whitworth AB, Kemmler G, Papp C, New risk factors for donor site seroma formation after latissimus dorsi flap breast reconstruction: 10-year period outcome analysis: J Plast Reconstr Aesthet Surg, 2011; 64(1); 69-74
30.. Pierce TD, Tomaino MM, Use of the pedicled latissimus muscle flap for upper-extremity reconstruction: J Am Acad Orthop Surg, 2000; 8(5); 324-31
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250