08 November 2021: Articles 
Gestational Diabetes Mellitus Complicated by Hemolysis, Elevated Liver Enzymes, and Low Platelet Count After Decreased Need for Insulin: 2 Cases
Unusual clinical course, Diagnostic / therapeutic accidents
Yoshimasa Kawarai12ABCDEF*, Shogo Kaneko3B, Masataka Kagimoto2B, Ayaka Kaneko2B, Naoki Ichii2B, Kaoru Kakinuma2B, Koyomi Saito2B, Motomasa Ihara12B, Toshiyuki Kakinuma2B, Michitaka Ohwada2B, Hirokazu Tanaka12BDFDOI: 10.12659/AJCR.933460
Am J Case Rep 2021; 22:e933460
Abstract
BACKGROUND: When a woman becomes pregnant, the placenta produces human placental lactogen (hPL). The anti-insulin effect of hPL raises maternal blood glucose levels, allowing the fetus to use glucose as a nutrient. Because hPL is produced by the placenta until delivery, insulin requirements in patients with gestational diabetes mellitus (GDM) typically increase, but in some cases, they may decrease. We retrospectively examined data from women with GDM who received insulin and delivered at our hospital.
CASE REPORT: From April 2019 to March 2020, we targeted patients who were diagnosed with GDM, received insulin, and delivered at our hospital. GDM was diagnosed based on the guidelines from the Japanese Society of Obstetrics and Gynecology. The rate of change in insulin dosage was calculated as: (insulin dosage at delivery − insulin dosage 14 days before delivery) divided by 14. Two patients whose insulin dosage was significantly reduced developed a syndrome of hemolysis, elevated liver enzymes, and low platelet count or acute fatty liver of pregnancy and underwent emergency cesarean section.
CONCLUSIONS: The present case report suggests that a decrease in insulin requirement in pregnant patients with GDM can predict maternal abnormalities due to placental dysfunction.
Keywords: Acute Fatty Liver Of Pregnancy, HELLP Syndrome, Insulin Resistance, Blood Glucose, Cesarean Section, Diabetes, Gestational, Female, Hemolysis, Humans, Insulin, Liver, Placenta, Platelet Count, Pregnancy
Background
In pregnancy, the placenta produces human placental lactogen (hPL), which increases insulin resistance. Moreover, the amount of insulin produced by the mother’s body also increases, but if it is insufficient, gestational diabetes mellitus (GDM) can occur. Patients in whom that happens are given insulin until their blood glucose levels are sufficiently controlled. As insulin resistance progressively increases before delivery, the insulin dosage is increased accordingly. In a few patients, the insulin dosage is decreased, but no studies to date have reported on perinatal prognosis in the setting of reduced insulin requirements during pregnancy. In the present study, we retrospectively examined data from patients with GDM who were treated with insulin and analyzed outcomes in those whose need for insulin decreased.
Case Reports
PROGRESS OF PATIENTS WITH GDM:
There were 30 patients with GDM, all of whom had singleton pregnancies. They were all Asian, well-nourished, and had no financial problems. The average age at diagnosis in all cases was 33.1±5.1 years, the average height was 157.5±5.2 cm, the average weight at pre-pregnancy was 60.6±14.3 kg, the average BMI calculated based on pre-pregnancy weight was 24.4±5.6 kg/m2, the average HOMA-IR (immunoreactive insulin [µu/mL]×fasting plasma insulin [mg/dL]÷405) was 2.03±1.4, the average HbA1c level was 5.4±0.4%, and the average GA level was 13.1±1.2%. There were 18 nulliparous women (5 uniparous, 6 biparous, and 1 multiparous [with 3 live births]). Concerning obstetric history, 5 patients had conceived after in vitro fertilization, 4 patients had a history of cesarean section, 1 had conceived after uterine myoma enucleation, 1 had a history of stillbirth with multiple malformations, 1 had preexisting epilepsy during pregnancy, 1 had preexisting hyper-thyroidism during pregnancy, and 1 had preexisting optic neuromyelitis during pregnancy (prednisolone sodium received at 10 mg/d). There were no cases of preeclampsia requiring hospitalization or medication (Table 1).
The average insulin dosage in all patients was 27.7±17.8 U/d, with the maximum and minimum insulin doses being 74 and 4 U/d, respectively. The changes in insulin dosage in all cases are shown in the line graph in Figure 1.
Concerning delivery outcomes, there were no stillbirths or intrauterine fetal deaths; 1 fetus was born prematurely and the remaining 29 were born at term. One case of preterm birth occurred at 33 weeks and 4 days gestation; the infant weighed 2037 g at birth. The average birth weight of term infants was 2841.1±322.6 g. The delivery patterns were as follows: vaginal delivery in 19 cases, elective cesarean section in 6 cases (previous cesarean section, post-fibroid pregnancy, and pregnancy with epilepsy in 4, 1, and 1 case, respectively), and emergency cesarean section in 5 cases. The breakdown of the emergency cesarean sections included 3 cases of labor arrest and 2 cases of hemolysis, elevated liver enzymes, and low platelet (HELLP) syndrome/clinical acute fatty liver of pregnancy (AFLP).
Blood test results from 2 patients with HELLP/AFLP (cases 24 and 28) are presented in Table 2. The patient in Case 24 underwent an emergency cesarean section at a gestational age of 33 weeks and 4 days and delivered a male infant with a birthweight of 2037 g. The infant’s Apgar scores were 7 (1 min) and 8 (5 min). The patient in Case 28 underwent an emergency cesarean section at a gestational age of 38 weeks and 2 days and delivered a female infant with a birthweight of 2445 g. The infant’s Apgar scores were 8 (1 min) and 10 (5 min). Because the infant in Case 24 was born prematurely, management in the Neonatal Intensive Care Unit was required, but in all other cases, no abnormalities were observed in the mother or baby.
The rate of change in insulin dosage measured from 14 days before delivery is presented in Figure 2. It was defined as the difference (Δ insulin dosage) between the amount of insulin used 14 days before delivery and during labor divided by 14. The formula is as follows:Rate of change in insulin dosage=(Δ insulin dosage)÷14
When the change in insulin dosage was positive, it indicated an increase in insulin dosage as delivery approached. Conversely, if it was negative, it meant that insulin dosage decreased near delivery.
The average rate of change in insulin dosage was 0.13±0.7. The rate of change in insulin dosage in Case 24 was −1.93; thus, the degree of deviance from the average rate of change was −2.06 and the rate of change in insulin dosage in Case 28 was −0.86. The degree of deviance from the average rate of change was −0.99 (Figure 2). The 2 cases (Cases 24 and 28), in which insulin requirements decreased by the greatest magnitude were those presumed to be in the patients who had HELLP/AFLP.
Discussion
We found that the 2 patients in whom the rate of change in insulin dosage was significantly negative were those presumed to have HELLP/AFLP (Figure 2). We investigated whether a decrease in insulin dosage suggested maternal abnormalities.
Pregnancy-related insulin resistance increases toward the end of the third trimester [2]. One of the reasons for this is hPL, which is produced by the placenta in pregnant women. The anti-insulin effect of hPL causes maternal blood glucose levels to rise, enabling the fetus to use glucose as a nutrient. Furthermore, hPL promotes lipolysis, resulting in production of free fatty acids and glycerol, which can be used as a nutrient source for the mother [3]. Beginning in gestational week 15, when placental function is complete, hPL increases rapidly and plateaus at around gestational week 36 [4]. Therefore, increased maternal insulin resistance is a natural phenomenon, and compensation for the increase in insulin secretion is required. In late pregnancy, insulin secretion is 2 to 3 times higher than that in a woman who is not pregnant [5]. If maternal insulin secretion is insufficient, insulin resistance becomes excessive and GDM develops [5]. Diet is the first line of treatment for GDM, but if glycemic control is poor, insulin injections are required.
hPL is a hormone produced by human placental syncytium cells and can be used as an index of placental function [6]. The amount of hPL gradually increases as pregnancy progresses, but it decreases in cases of intrauterine growth restriction and preeclampsia [6]. Therefore, when placenta function declines, hPL produced by the placenta decreases, resulting in decreased insulin resistance and insulin requirements.
The patients in Cases 24 and 28 both had acute onset of upper abdominal pain, which led to further examination, such as blood tests. There is no international consensus on the diagnostic criteria for HELLP/AFLP; however, in general, HELLP syndrome is diagnosed in patients who have lactate dehydrogenase (LDH) >600 IU/L, aspartate aminotransferase (AST) >70 IU/L, and platelet count <150×103/μL [7]. The platelet counts of the 2 patients in the present study who were presumed to have HELLP/AFLP met the criterion. However, some of the other values did not meet the diagnostic criteria, such as an LDH of 482 IU/L and AST of 115 IU/L in Case 24 and an LDH of 352 IU/L and an AST of 50 IU/L in Case 28. Moreover, 80% of patients with HELLP syndrome have hypertension. However, because no hypertension was observed in the 2 patients in the present study, the likelihood of AFLP was increased, given the similar clinical symptoms and blood test findings [7].
No diagnostic criteria have been established for AFLP. However, according to the Swansea criteria used in Europe and the United States, AFLP is diagnosed if 6 or more of the following 14 criteria are met: clinical symptoms: vomiting, abdominal pain, significant fluid intake and frequent urination, and encephalopathy; blood test findings: hyperbilirubinemia (>0.8 mg/dL), hypoglycemia (<72 mg/dL), elevated uric acid levels (>5.7 mg/dL), leukocytosis (>11000 cells/μL), elevated liver enzymes (AST and alanine transaminase [ALT] levels >42 IU/L), hyperammonemia (>27.5 mg/dL), elevated creatinine (>1.7 mg/dL), and abnormal coagulation (PT >14 s or APTT >34 s); radiographic findings: ultrasound findings of ascites or bright liver; and liver biopsy indicative of microvesicle steatosis [8]. The patient in Case 24 had abdominal pain, hyperbilirubinemia, and elevated liver enzyme levels; in the patient in Case 28, abdominal pain, hyperbilirubinemia, an increased uric acid level, and increased liver enzyme levels were present, which are in accordance with the aforementioned criteria. However, AFLP was not diagnosed. Furthermore, AFLP is characterized by a decrease in antithrombin (AT) activity. However, AT activity was not measured in Case 24 and AT activity was found to be 82% in Case 28, which was within the standard range. Thus, a decrease in AT activity was not observed [9]. Therefore, although the diagnosis of HELLP/AFLP was not confirmed in the 2 patients in the present study, their platelet counts were significantly reduced and there was no question that rapid delivery by emergency cesarean section was required to prevent disseminated intravascular coagulation.
The exact cause of HELLP syndrome remains unknown, but hepatic ischemia due to vascular endothelial damage and spasm of the proper hepatic artery is considered the main pathology [10]. In the patient in Case 24, a histopathological examination of the placenta was performed, but there was no infarction; only mild chorioamnionitis was observed. Moreover, there were no findings suggestive of vascular endothelial damage.
The etiology of AFLP remains unknown, but there is a theory that it is caused by abnormal fatty acid metabolism during pregnancy. Free fatty acids increase, especially in late pregnancy, and promote fetal placenta development. In cases in which there is a defect in fatty acid metabolism in the mother and fetus, metabolic intermediates may accumulate in the blood and hepatocytes of the mother, where they can cause adverse effects [11].
In the 2 patients in the present study who were suspected of developing HELLP/AFLP, placenta function declined for some reason, resulting in a decrease in hPL production by the placenta. Therefore, maternal insulin resistance and the subsequent requirement for insulin were believed to have decreased. Presumably, the decrease in hPL production caused stagnation of lipolysis in the liver, resulting in abnormal lipid metabolism, damage to the organ and vascular endothelium, an increase in hepatic enzymes (AST and ALT), and a decrease in platelet counts.
Complications in maternal infants associated with abnormal glucose metabolism include large-for-dates infants, neonatal hypoglycemia, neonatal respiratory distress, preterm birth (PTB), neonatal asphyxia due to shoulder dystocia, intrauterine fetal death, and congenital abnormalities [12–15]. Of the 30 patients whose cases were examined in the present study, only 1 (3.3%) had PTB. The frequency of PTB in women with GDM is 14%. Therefore, it seems that our hospital’s GDM management was adequate [11].
The present study had some limitations. First, the sample size was small. In addition, important clinical and metabolic characteristics were not examined, as maternal dyslipidemia and hPL were not assessed. Therefore, it is necessary to examine more cases in the future.
Conclusions
We investigated changes in insulin dosage in patients with GDM who required insulin. Insulin requirements usually increase in late pregnancy. However, there were many cases in the present study in which insulin requirements decreased and those patients developed a condition suspected to be HELLP/AFLP and required emergency cesarean section. However, none of the patients developed preeclampsia or hypertension that required hospitalization or medication.
If a pregnant woman cannot produce enough insulin, she may develop GDM. Conversely, if her insulin requirement decreases, she may develop HELLP/AFLP. This finding suggests that a decrease in insulin requirement can predict HELLP/AFLP.
Figures
References:
1.. : Guidelines for obstetrical practice in Japan, 2020, Tokyo, JSOG
2.. Sonagra AD, Biradar SM, Dattatreya K, Normal pregnancy – a state of insulin resistance: J Clin Diagn Res, 2014; 8; CC013
3.. Mochizuki M, Morikawa H, Ohga Y, Tojo S, Lipolytic action of human chorionic somatomammotropin: Endocrinol Jpn, 1975; 22; 123-29
4.. Furuhashi N, Tachibana Y, Shinkawa O, Simultaneous and serial measurement of serum levels of human placental lactogen, beta-human chorionic gonadotropin and unconjugated estriol levels in pregnant women: Tohoku J Exp Med, 1984; 144; 211-15
5.. Catalano PM, Tyzbir ED, Roman NM, Longitudinal changes in insulin release and insulin resistance in nonobese pregnant women: Am J Obstet Gynecol, 1991; 165; 1667-72
6.. Ronin-Walknowska E, Holmgren PA, von Schoultz B, Stigbrand T, Placental alkaline phosphatase compared with human placental lactogen and oestriol in high-risk pregnancies: Gynecol Obstet Invest, 1984; 18; 206-11
7.. Sibai BM, Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count: Obstet Gynecol, 2004; 103; 981-91
8.. Ch’ng CL, Morgan M, Hainsworth I, Kingham JGC, Prospective study of liver dysfunction in pregnancy in Southwest Wales: Gut, 2002; 51; 876-80
9.. Minakami H, Morikawa M, Yamada T, Differentiation of acute fatty liver of pregnancy from syndrome of hemolysis, elevated liver enzymes and low platelet counts: J Obstet Gynaecol Res, 2014; 40; 641-49
10.. Barton JR, Riely CA, Adamec TA, Hepatic histopathologic condition does not correlate with laboratory abnormalities in HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count): Am J Obstet Gynecol, 1992; 167; 1538-43
11.. Ibdah JA, Bennett MJ, Strauss AW, A fetal fatty-acid oxidation disorder as a cause of liver disease in pregnant women: N Engl J Med, 1999; 340; 1723-31
12.. Persson M, Pasupathy D, Hanson U, Norman M, Birth size distribution in 3,705 infants born to mothers with type 1 diabetes: A population-based study: Diabetes Care, 2011; 34; 1145
13.. Cordero L, Treuer SH, Landon MB, Gabbe SG, Management of infants of diabetic mothers: Arch Pediatr Adolesc Med, 1998; 152; 249
14.. Weindling AM, Offspring of diabetic pregnancy: Short-term outcomes: Semin Fetal Neonatal Med, 2009; 14; 111-18
15.. Kodama Y, Sameshima H, Ikenoue T, Regional population-based study on pregnancy outcomes in women with diabetes mellitus in Japan: J Obstet Gynaecol Res, 2007; 33; 45-48
Figures
Tables
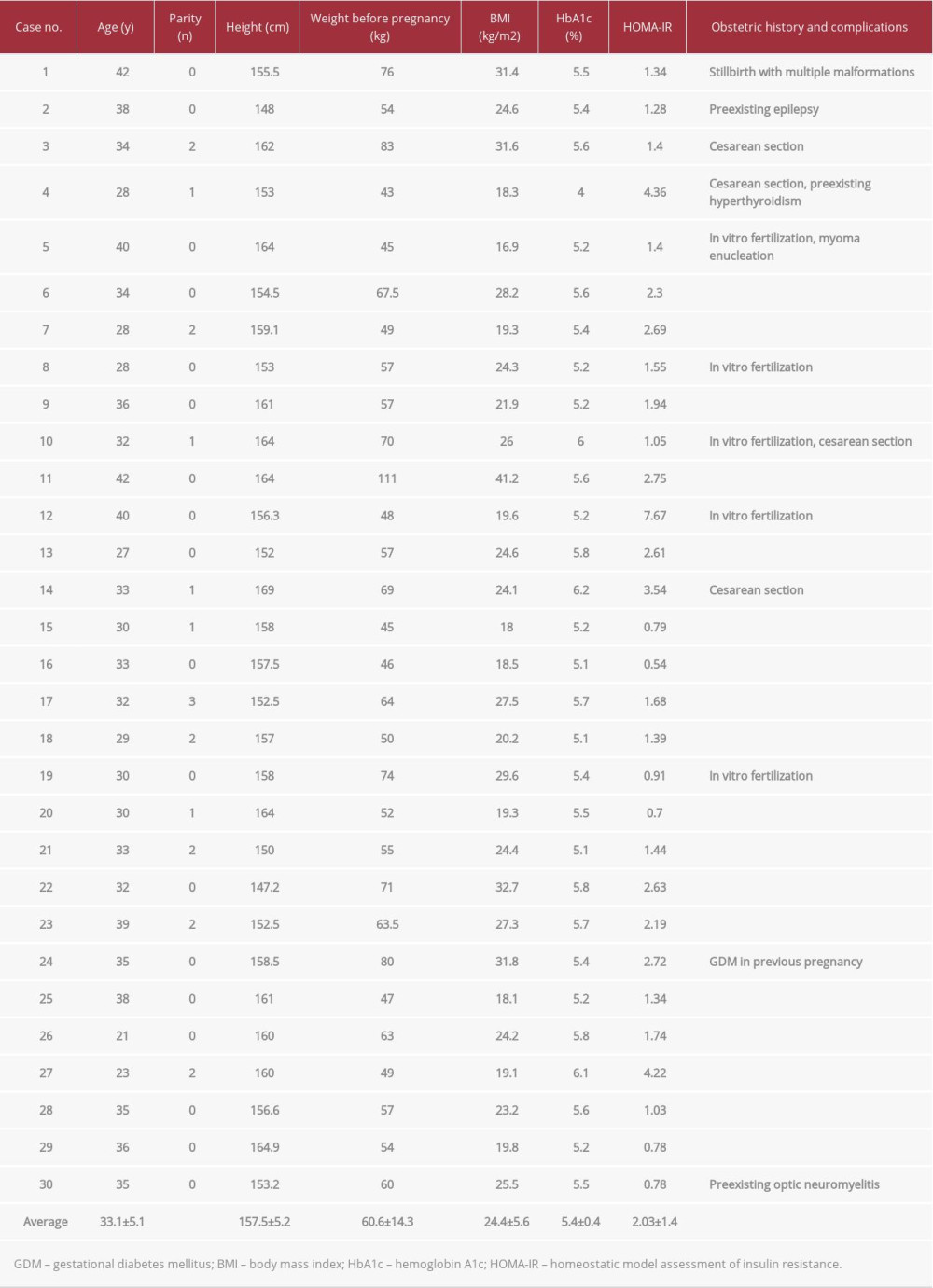 Table 1.. Baseline characteristics of the 30 patients with GDM.
Table 1.. Baseline characteristics of the 30 patients with GDM.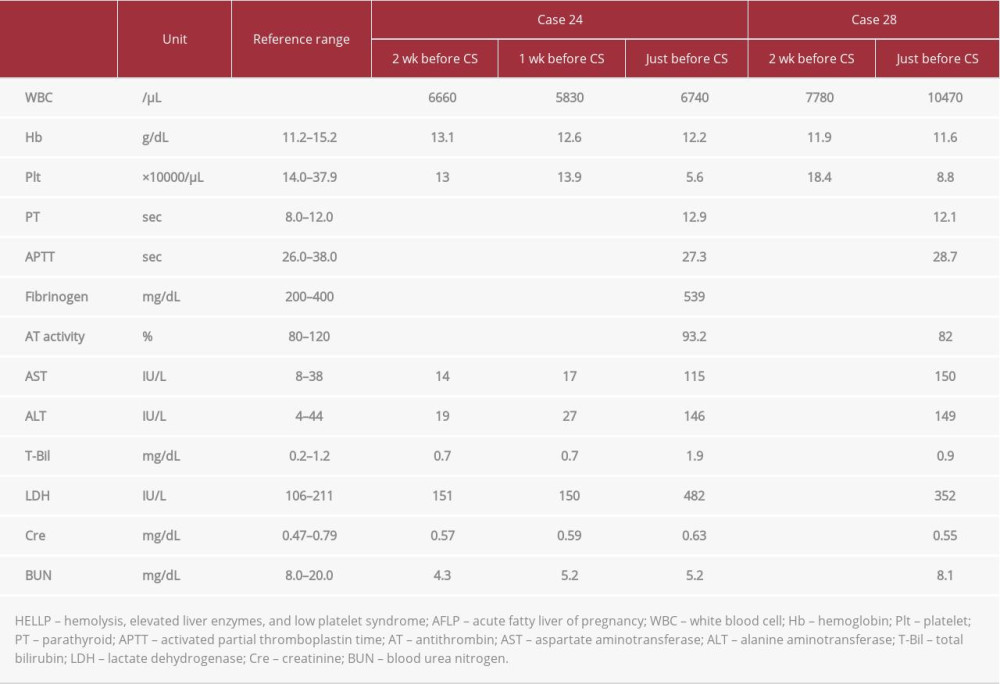 Table 2.. Results of biochemical blood tests in 2 patients suspected of developing HELLP/AFLP.
Table 2.. Results of biochemical blood tests in 2 patients suspected of developing HELLP/AFLP.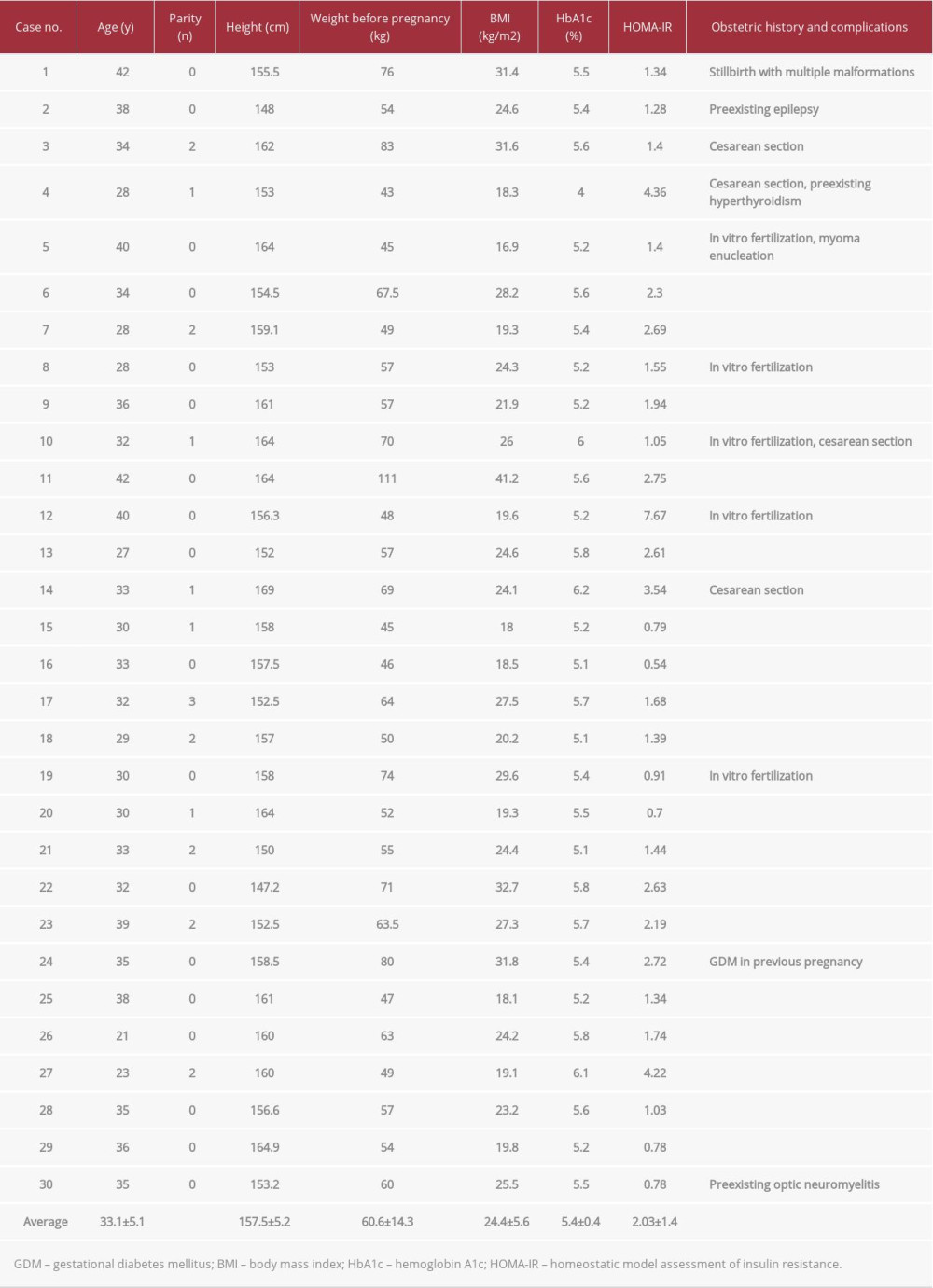 Table 1.. Baseline characteristics of the 30 patients with GDM.
Table 1.. Baseline characteristics of the 30 patients with GDM.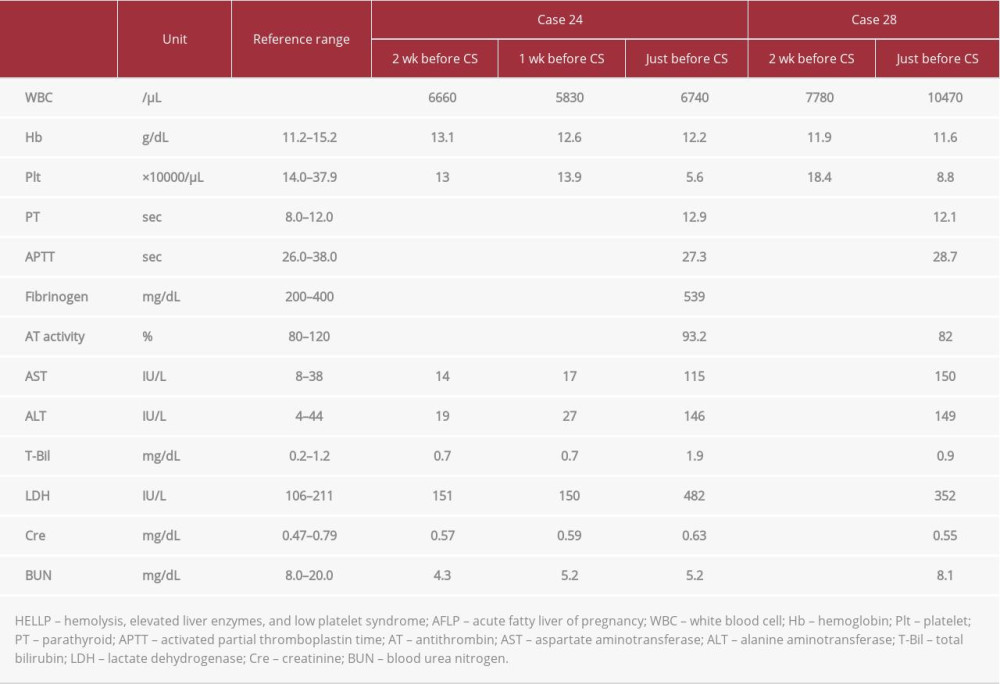 Table 2.. Results of biochemical blood tests in 2 patients suspected of developing HELLP/AFLP.
Table 2.. Results of biochemical blood tests in 2 patients suspected of developing HELLP/AFLP. In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








