10 February 2022: Articles 
Case Report of Cardiorenal Syndrome with Ascites and Peritonitis: The Role of Large-Volume Paracentesis and Albumin Replacement
Challenging differential diagnosis, Unusual or unexpected effect of treatment, Rare disease
Minas Karagiannis1BEF*, Panagiotis Giannakopoulos1BF, Aggeliki Sardeli1D, Ourania Tsotsorou1D, Dimitra Bacharaki1D, Demetrios V. Vlahakos1DEFDOI: 10.12659/AJCR.934423
Am J Case Rep 2022; 23:e934423
Abstract
BACKGROUND: Spontaneous bacterial peritonitis is a common infection in hospitalized patients with ascites, particularly in patients with cirrhosis. Spontaneous bacterial peritonitis is often associated with acute kidney injury. The causative agents of spontaneous bacterial peritonitis are usually gram-negative bacteria, but lately, the prevalence of spontaneous bacterial peritonitis caused by gram-positive bacteria is rising.
CASE REPORT: In this report, we present the case of a 77-year-old woman with a history of cardiorenal syndrome with ascites and chronic kidney disease who was admitted with diarrhea, fever, and abdominal pain. Ascitic fluid paracentesis revealed spontaneous bacterial peritonitis due to Listeria monocytogenes. During hospitalization, her ascites gradually enlarged and her kidney function deteriorated. The deterioration of kidney function was at least partially attributed to sepsis caused by spontaneous bacterial peritonitis. In addition to proper antibiotic therapy with ampicillin and daily hemodialysis sessions, large-volume paracentesis and albumin infusions were instituted. After 5 days, she showed a fast improvement, the ascites subsided, and her renal function returned to baseline.
CONCLUSIONS: Spontaneous bacterial peritonitis caused by Listeria monocytogenes is associated with a poor outcome. Acute kidney injury in patients with spontaneous bacterial peritonitis is common and related with a poor outcome. Data about the role of large-volume paracentesis and albumin replacement in patients with spontaneous bacterial peritonitis are still ambiguous. In the literature, all patients with spontaneous bacterial peritonitis due to Listeria monocytogenes who underwent large-volume paracentesis survived.
Keywords: Acute Kidney Injury, Listeria monocytogenes, Paracentesis, peritonitis, Renal Dialysis, Albumins, Ascites, Cardio-Renal Syndrome, Female, Humans
Background
Spontaneous bacterial peritonitis (SBP) is an infection of the ascitic fluid without a detectable intraabdominal surgically treatable source of infection. SBP develops in up to 30% of patients with ascites who are admitted to hospitals, particularly patients with cirrhosis [1]. The major mechanism is considered to be the bacterial translocation of gram-negative enteric bacteria, which have been found to be the main causative agents. Of particular interest is, however, that an increasing prevalence of SBP (48–62%) due to gram-positive bacteria has been observed over the last decade, particularly in Europe [2].
In this report, we present the first case of a patient with cardiorenal syndrome and ascites who was diagnosed with peritonitis due to
Case Report
The case of a 77-year-old woman who presented with fever, abdominal pain, and diarrhea for the past 5 days is presented in this report. The patient’s medical history was significant for hypertension, insulin-treated diabetes mellitus, coronary artery disease, right-sided congestive heart failure with severe tricuspid regurgitation, chronic atrial fibrillation with acenocumarol treatment, and chronic kidney disease, with a baseline creatinine value of 2.5 mg/dL and an estimated glomerular filtration rate by MDRD formula of 20 mL/min/1.73 m 2. There was no history of liver disease or alcohol or drug use. She underwent a percutaneous transluminal coronary angioplasty 4 years earlier, a partial colectomy for repeated diver-ticular bleeding 2 years earlier, and a pacemaker implantation 8 months earlier.
On physical examination, she was awake and oriented to self and place. Her blood pressure was 100/70 mmHg, heart rate was 90 beats per min, temperature was 38°C, and oxygen saturation was 97% on room air. Notable findings were a large firm liver, large ascites with tenderness in the lateral abdominal wall, and 1+ pitting edema in the lower extremities.
Initial laboratory tests revealed a white blood cell count of 8510 K/μL, C-reactive protein of 200 mg/L (reference range, below 5 mg/L), and procalcitonin of 22 ng/mL (reference range, below 0.5 ng/mL). Additional results of the analysis of the blood chemistry were as follows: serum creatinine of 3.5 mg/dL, international normalized ratio (INR) of 5, brain natriuretic peptide of 9487 pg/mL, serum bicarbonate 17 mEq/L, blood urea nitrogen of 111 mg/dL, total bilirubin of 1.21 mg/dL, direct bilirubin of 0.86 mg/dL, aspartate aminotransferase of 22 U/L, alanine aminotransferase of 7 U/L, alkaline phosphatase of 73 U/L, and γGT of 23 U/L. Her urinalysis was negative for infection.
A transthoracic echocardiogram was performed and was notable for an ejection fraction of 55%, with global hypokinesis, a dilated inferior vena cava, and an elevated pulmonary artery pressure of 52 mmHg. An abdominal computed tomography (CT) scan showed a small right pleural effusion and a large amount of free intraperitoneal fluid.
Because of concern for sepsis, she was empirically started on metronidazole and ceftolozane-tazobactam. After normalization of the INR, a diagnostic paracentesis of the ascites was performed. The aspirated fluid was dark yellow and turbid with total fluid protein of 5.21 g/dL and white blood cell count of 5120/mm3 (98% polymorphonuclear cells). The culture of the ascitic fluid revealed
During hospitalization, before
Discussion
In this case, SBP was caused by an uncommon bacterial agent,
Patients with cirrhosis with listeria-infected ascites have been estimated to have mortality in the range of 30%. Patients usually die within 6 days of contracting the infection [5].
Acute kidney injury has been long known to be associated with SBP in up to 43% of such patients, and this relation is associated with a 6-fold mortality increase [6,7]. The acute kidney injury in SBP can be related to inflammatory molecules and endotoxemia [8]. The concentration of lipopolysaccha-ride is higher among cirrhotic patients with SBP and is associated with lower renal blood flow, glomerular filtration rate, and stagnation of the microvascular flow. Accompanying antibiotics with albumin therapy has been demonstrated to reduce the incidence of renal impairment and in-hospital mortality from 29% to 10% [9], compared with antibiotics alone. Similarly, a recent Cochrane review supported the use of albumin for SBP and demonstrated protective effects on renal function and mortality [10]. These findings emphasize the significance of the correction of effective volume and the reduction of ascitic volume anticipated by the improvement of the intravascular colloid osmotic pressure induced by albumin infusion.
Since our patient developed acute-on-chronic kidney injury, daily hemodialysis sessions were initiated to control uremia, balance volume and electrolytes, and allow the administration of intravenous albumin infusion and the performance of LVP to decrease intraabdominal pressure and possibly reduce toxic burden. It is important to mention that there is an extreme paucity of evidence regarding the role and safety of LVP in SBP, and there are no clinical guidelines to provide recommendations on whether LVP can be considered in SBP. One small, randomized controlled study showed no worse outcomes with LVP and maybe a faster symptom relief course [11]. However, postulation of removing toxic burden through paracentesis was not confirmed in another nonrandomized trial [12].
There are 9 reported cases with
Conclusions
In conclusion, diagnostic paracentesis should immediately be performed in any patient with ascites and signs suggestive of SBP, such as fever, gastrointestinal discomfort, altered mental status, and hypotension. Broad-spectrum antibiotic therapy is recommended initially and can be narrowed when susceptibility results become available. Acute kidney failure should be recognized and treated with hemodialysis, if needed. Intravenous albumin infusion and LVP seem to improve patient outcome (Figure 1). However, further investigations are warranted to delineate the clinical risks and benefits of LVP in SBP.
References:
1.. Marciano S, Díaz JM, Dirchwolf M, Gadano A, Spontaneous bacterial peritonitis in patients with cirrhosis: Incidence, outcomes, and treatment strategies: Hepat Med, 2019; 11; 13-22
2.. Fiore M, Maraolo AE, Gentile I, Current concepts and future strategies in the antimicrobial therapy of emerging Gram-positive spontaneous bacterial peritonitis: World J Hepatol, 2017; 9(30); 1166-75
3.. Liatsos GD, Thanellas S, Pirounaki M: Scand J Gastroenterol, 2012; 47(10); 1129-40
4.. Gaspar R, Rodrigues S, Macedo G: Clin Res Hepatol Gastroenterol, 2017; 41(5); e68-70
5.. Tablang MV: Case Rep Gastroenterol, 2008; 2(3); 321-25
6.. Follo A, Llovet JM, Navasa M, Renal impairment after spontaneous bacterial peritonitis in cirrhosis: Incidence, clinical course, predictive factors and prognosis: Hepatology, 1994; 20(6); 1495-501
7.. Devani K, Charilaou P, Jaiswal P, Trends in hospitalization, acute kidney injury, and mortality in patients with spontaneous bacterial peritonitis: J Clin Gastroenterol, 2019; 53(2); e68-74
8.. Peng JL, Techasatian W, Hato T, Liangpunsakul S, Role of endotoxemia in causing renal dysfunction in cirrhosis: J Investig Med, 2020; 68(1); 26-29
9.. Sort P, Navasa M, Arroyo V, Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis: N Engl J Med, 1999; 341(6); 403-9
10.. Zaccherini G, Tufoni M, Bernardi M, Albumin administration is efficacious in the management of patients with cirrhosis: A systematic review of the literature: Hepat Med, 2020; 12; 153-72
11.. Choi CH, Ahn SH, Kim DY, Long-term clinical outcome of large volume paracentesis with intravenous albumin in patients with spontaneous bacterial peritonitis: A randomized prospective study: J Gastroenterol Hepatol, 2005; 20(8); 1215-22
12.. Abd Elaal MM, Zaghloul SG, Bakr HG, Evaluation of different therapeutic approaches for spontaneous bacterial peritonitis: Arab J Gastroenterol, 2012; 13(2); 65-70
13.. Eisa M, Tefera K, Alvanpour A: IDCases, 2018; 14; e00430
14.. Gaspar R, Rodrigues S, Macedo G: Clin Res Hepatol Gastroenterol, 2017; 41(5); e68-70
15.. Beckerleg W, Keskar V, Karpinski J, Peritonitis as the first presentation of disseminated listeriosis in a patient on peritoneal dialysis – a case report: Perit Dial Int, 2017; 37(2); 239-40
16.. How J, Azar MM, Meyer JP: Conn Med, 2015; 79(1); 31-36
17.. Shaikh B, Pathak R, Mainali NR, Gupta S: J Community Hosp Intern Med Perspect, 2015; 5(1); 26153
18.. Yecies T, Inagami S: Case Reports Hepatol, 2013; 2013; 832457
19.. Cardoso C, Cremers I, Oliveira AP: Ann Hepatol, 2012; 11(6); 955-57
20.. Galan SR, Kann PH, Gress TM, Michl P: Z Gastroenterol Jul, 2011; 49(7); 832-35
21.. Haneche F, Brocard A, Garioud A, Cadranel JF, [Spontaneous bacterial peritonitis with listeria monocytogenes leading to a cirrhosis discovery]: Presse Med, 2017; 46(3); 332-34 [in French]
22.. Kubiak BD, Albert SP, Gatto LA, Peritoneal negative pressure therapy prevents multiple organ injury in a chronic porcine sepsis and ischemia/ reperfusion model: Shock, 2010; 34(5); 525-34
Tables
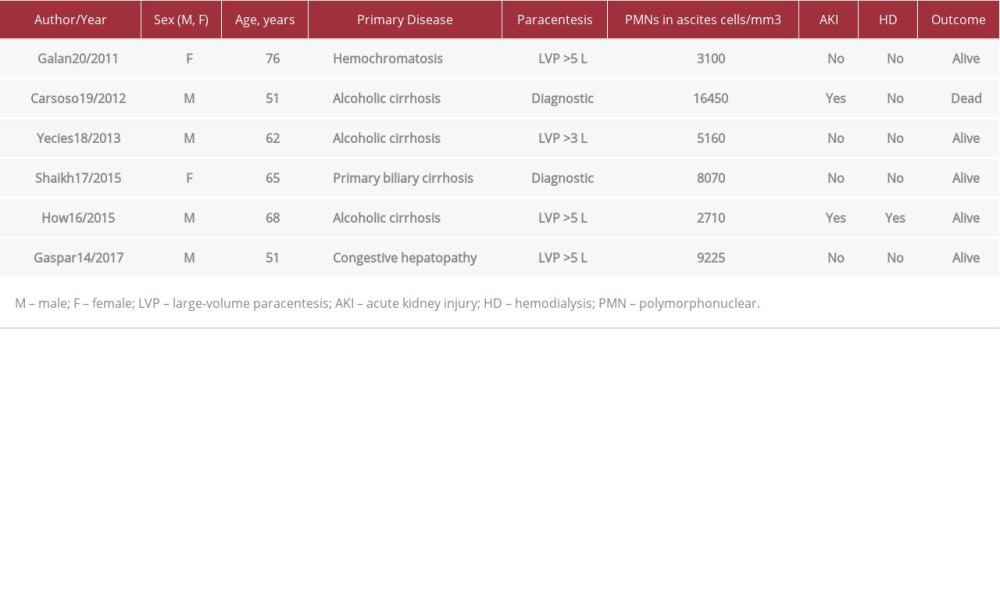 Table 1.. Nine case reports of spontaneous bacterial peritonitis with Listeria monocytogenes reporting volume of paracentesis published over the past decade.
Table 1.. Nine case reports of spontaneous bacterial peritonitis with Listeria monocytogenes reporting volume of paracentesis published over the past decade.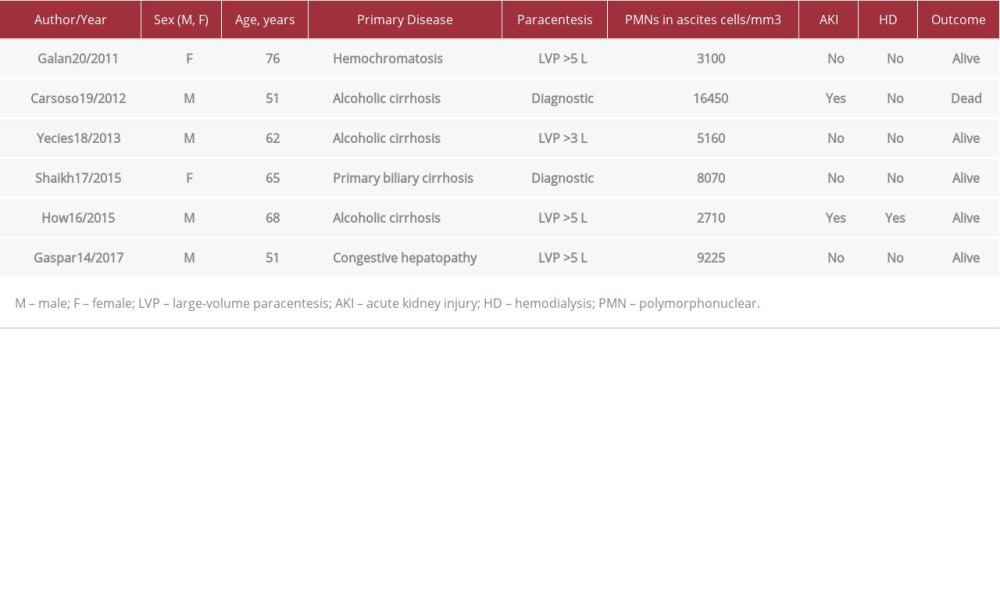 Table 1.. Nine case reports of spontaneous bacterial peritonitis with Listeria monocytogenes reporting volume of paracentesis published over the past decade.
Table 1.. Nine case reports of spontaneous bacterial peritonitis with Listeria monocytogenes reporting volume of paracentesis published over the past decade. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








