07 February 2022: Articles 
Multisystemic Sarcoidosis Presenting with Widespread Vertebral Osseous and Visceral Lesions Masquerading as Metastatic Disease: A Case Report and Literature Review
Challenging differential diagnosis, Rare disease
Eltaib SaadDOI: 10.12659/AJCR.935158
Am J Case Rep 2022; 23:e935158
Abstract
BACKGROUND: Sarcoidosis is a systemic granulomatous disease which predominantly affects the lungs, skin, and lymph nodes. Vertebral sarcoidosis is a rare entity. The clinical presentation of sarcoidosis with diffuse vertebral osseous and visceral lesions, simulating a disseminated metastatic cancer, is extremely unusual and has been reported only in a handful of cases in the current literature.
CASE REPORT: A 78-year-old White female patient with a remote history of asymptomatic pulmonary sarcoidosis presented with a 1-month history of generalized weakness. Physical examination was positive for upper and lower midline spinal tenderness. Laboratory findings showed anemia, hypercalcemia, and deranged liver functions. Abdominal imaging revealed an enlarged and nodular liver, ascites, splenomegaly, and enlarged retroperitoneal lymph nodes. Spinal imaging demonstrated several multi-level vertebral osseous lesions suspicious for metastatic bone cancer. Following extensive diagnostic work-up to rule out underlying metastatic cancers, a bone biopsy from an iliac lesion demonstrated active non-caseating granulomas, and a diagnosis of multisystemic sarcoidosis was made. The patient was started on systemic corticosteroids and demonstrated a gradual symptomatic improvement. Follow-up imaging revealed interval resolution of vertebral lesions.
CONCLUSIONS: The clinical and radiological features of vertebral sarcoidosis can be indistinguishable from metastatic bone cancers. The possibility of widespread extrapulmonary sarcoidosis should be considered in any patients with a remote history of pulmonary sarcoidosis who experience simultaneous onset of unexplained multisystemic symptoms.
Keywords: Bone Diseases, Osseus, Rare Diseases, sarcoidosis, Female, Granuloma, Humans, lymphadenopathy, Neoplasms, Spine
Background
Sarcoidosis is a chronic granulomatous inflammatory disease that can affect almost any organ system [1]. It predominantly affects the lungs, skin, and lymph nodes, followed by the liver, eyes, kidneys, and joints [1,2]. Bony involvement is typically unusual and tends to affect the long bones and phalanges of the hands and feet [2]. Nevertheless, vertebral sarcoidosis represents a rare occurrence that often poses a diagnostic dilemma, as it closely mimics metastatic bone cancers and multiple myeloma, both clinically and radiologically [3–5]. In this report, we present a rare case of a diffuse multisystemic sarcoidosis with extensive vertebral and visceral lesions, simulating disseminated metastatic carcinomas, in an elderly woman with a remote history of asymptomatic pulmonary sarcoidosis, which never required a medical treatment in the past.
Case Report
A 78-year-old White woman presented to our department with a 1-month history of generalized weakness, backpain, and vague abdominal discomfort. The patient denied recurrent fevers, chills, cough, nausea, vomiting, weight loss, itching, urinary, or bowel symptoms. The rest of the systemic review was insignificant. The patient notably had a past medical history significant for biopsy-proven sarcoidosis of the hilar lymph nodes, which was diagnosed 12 years prior to her index presentation. At that time, the patient had bilateral hilar lymph-adenopathy visualized on a routine chest radiography, which was indicated for a preoperative work-up, but she denied any respiratory symptoms at that time. The disease seemed clinically silent during the interim period, as the patient did not report any symptoms related to sarcoidosis nor had she received specific treatment pertinent for the latter throughout the 12 years, according to the patient and the electronic medical record search. Her past medical history was also relevant for hypertension and uterine fibroids, following a vaginal hysterectomy 12 years prior. Her regular home medications included amlodipine and cholecalciferol. The patient lived at home with her daughter and was independent in her daily life activities. She denied drinking alcohol and a history of smoking.
The physical examination revealed stable vital signs. The neurological examination revealed mild lower-extremity weakness, with a power of grade 4 bilaterally. The sensory examination demonstrated intact sensation to light touch bilaterally. The back examination revealed upper and lower midline spinal tenderness with no focal tenderness or overlying skin erythema. No paraspinal masses or bony deformities were noted. The anal reflex was intact. Notably, the neurological examination of the upper extremities was essentially normal. The abdominal examination elicited a distended abdomen with mild diffuse tenderness over all quadrants, and the percussion note was positive for minimal ascites. No guarding or rigidity was appreciated. The cardiovascular and respiratory examinations were unremarkable, and no palpable lymphadenopathy was elicited.
The complete blood count showed mild normocytic anemia (hemoglobin of 9.5 g/dL; reference range, 12–14 g/dL). The serum creatinine level was mildly elevated at 1.89 mg/dL (reference range, 0.6–1.3 mg/dL), there was hypercalcemia (calcium level was 11.5 mg/dL; reference range, 8–10 mg/dL), and the phosphorus level was normal. The erythrocyte sedimentation rate was slightly raised at 39 mm/h (reference range, 0–30 mm/h). The liver function parameters were newly de-ranged as transaminases were elevated with alanine transaminase at 88 IU/L (reference range, 7–50 IU/L), and aspartate transaminase at 99 IU/L (reference range, 14–40 IU/L). The alkaline phosphatase level was also elevated at 169 IU/L (reference range, 35–104 IU/L). Considering the patient’s history, physical examination findings, and laboratory results that pointed toward multi-organ involvement, a provisional diagnosis of an indolent systemic disease process, likely an occult metastatic disease or multiple myeloma, was initially suggested. Serial laboratory work-up and imaging studies were warranted for further investigations.
Magnetic resonance imaging (MRI) of the spine revealed multiple osseous lesions throughout the thoracic spine, lumbar spine, sacrum, and iliac bones, which were very highly concerning of metastatic disease or multiple myeloma. The lumbar lesions were described as T2-hyperintense-enhancing lesions in the vertebral bodies of L1, L3, L4, and S1 (Figure 1A, 1B). Similar lesions were also encountered on the right and left iliac bones. On the thoracic spine, T2-hpyperintesne lesions were demonstrated on the vertebral bodies of T1, T2, T4, T6, T8, and T12 (Figure 1C). No signs of discitis or epidural abscess were demonstrated all along the spine. Ultrasonography of the abdomen revealed moderate ascites with a nodular liver. Moderate-sized bilateral renal lesions were also seen. There were no signs of obstructive nephropathy. Computed tomography (CT) of the abdomen depicted a nodular-appearing liver with hypodense lesions, moderate splenomegaly up to 15 cm, and moderate ascites (Figure 2). Small-sized retroperitoneal lymph nodes were visualized. No para-aortic or mesenteric lymphadenopathy was noted. The scan was negative for any suspicious colonic or pancreatic masses. A thoracic CT scan revealed nodular lesions on both upper lobes bilaterally (Figure 3A, 3B). There were no hilar or mediastinal masses or lymphadenopathy, and no discrete masses or pleural effusions were demonstrated.
A hepatic panel was ordered. Viral hepatitis screening (HAV, HBV, HCV, and HIV) was negative. The titers of anti-mitochondrial and anti-smooth muscle autoantibodies were non-reactive. Serum ceruloplasmin, iron studies, and lactate dehydrogenase were all within normal limits. An ultrasound-guided transcutaneous liver biopsy displayed expanded portal triads and several non-caseating granulomas. A hepatology consultation recommended an autoimmune and infectious screening to identify the underlying etiology of the granulomatous disease. Autoantibodies (ANA, ANCA, immunoglobulin G4) were negative, and angiotensin-converting enzyme levels were within the reference range. Acid-alcohol-fast bacilli staining and Giemsa staining were negative for any tuberculous and fungal organisms, respectively. Infectious work-up for granulomatous liver disease was negative for
A rheumatology consultation recommended high-dose methylprednisolone (30 mg every 12 h) for 3 days followed by oral prednisolone (40 mg daily) for 7 days as inpatient. The patient was discharged on oral prednisolone (30 mg daily) with a gradual tapering over 8 weeks. Of note, the patient was re-admitted after 5 weeks of discharge with a urinary tract infection while she was on steroids, but she appreciated a gradual improvement of backpain and lower extremity weakness. A follow-up spinal MRI after 2 months revealed interval resolution of some thoracic and lumbar vertebral lesions, without new interval findings.
Discussion
Sarcoidosis predominantly affects the lungs, skin, and lymph nodes, and the subclinical involvement of other organ systems is not uncommon [1–5]. However, presentation with a clinically apparent multisystem disease with disseminated vertebral and visceral lesions, as reported in our patient, is rare, as this pattern of presentation has been reported in only a handful of cases [4–7]. An interesting case of a 59-year-old woman who had a clinically silent and incidentally diagnosed multisystemic sarcoidosis with extensive osseous, hepatic, and pulmonary lesions was described by Mehrotra et al [8]; the patient had presented with a facial nerve palsy, which complicated a viral infection, but further diagnostic work-up revealed a widespread sarcoidosis, and the patient was deemed ineligible for steroids treatment as she was utterly asymptomatic from the perspective of sarcoidosis. This is in contrast to our reported patient, who actively experienced sarcoidosis-related symptoms that necessitated medical intervention.
In fact, it is quite challenging for clinicians to suspect a disseminated extrapulmonary sarcoidosis, as its clinical features are rather diverse and largely nonspecific, as demonstrated in our case [4–7], and the diagnosis warrants the exclusion of other causes of chronic granulomatous diseases, including infections, such as tuberculosis and histoplasmosis, systemic autoimmune diseases, such as Crohn disease, and metastatic cancers, including lymphomas and multiple myeloma [7]. The latter are great mimickers of multisystemic sarcoidosis with vertebral involvement, and similar cases of osseous sarcoidosis were initially thought to be or misdiagnosed as meta-static bone diseases, owing to the extreme clinical and radiological similarities between the 2 disease entities [4,5,8–10].
Vertebral sarcoidosis is a rare occurrence [4,5,8,9] and tends to exhibit a peculiar involvement to the thoracic and upper lumbar vertebral bodies (as observed in our case), with much less frequent affection of the cervical vertebrae [5,9]. It typically presents with persistent back pain [1,4]. Vertebral compression fractures and neurological sequalae are unusual complications, but they have been reported [1,4,5,9]. MRI imaging in vertebral sarcoidosis demonstrates low signals on T1-weighted images and hyper-intense signals on T2-weighted images owing to a granulomatous infiltration of the marrow [5,9]. These MRI appearances are extremely similar to those of multiple myeloma and osteolytic bone metastases [10]. Other radiological findings include mixed osteolytic and osteosclerotic lesions, and rarely, predominant osteosclerotic lesions simulating osteoblastic metastases [5]. It is worth mentioning that positron emission tomography with 18-fluorodeoxyglucose imaging (FDG) might not be very differentiating between the vertebral sarcoidosis and metastatic cancers [5], as FDG also accumulates within the activated macrophages and epithelioid cells in active granulomatous inflammation [5]; therefore, only the bone biopsy is considered the criterion standard to prove sarcoidosis and to exclude metastatic cancers or multiple myeloma [4,5].
Interestingly, osseous sarcoidosis rarely occurs without symptomatic pulmonary disease and is usually identified at the time of initial diagnosis of thoracic sarcoidosis [3]; however, our patient presented with the bony disease after 12 years of the diagnosis of the thoracic disease, an unusual pattern of presentation of osseous sarcoidosis [1]. Table 1 summarizes the patient characteristics and clinical features of similar cases of multisystemic sarcoidosis with vertebral involvement. It remains largely unexplained why our patient’s sarcoidosis remained clinically silent for almost 12 years and then suddenly progressed to involve multiple organs [4,5].
Careful consideration should be given to rule out a sarcoidosislymphoma syndrome in patients with asymptomatic sarcoidosis who suddenly experience interval enlargement of pre-exiting lymphadenopathy or those who develop new-onset lymph-adenopathy [11]. The presumed association between sarcoidosis and malignancy remains controversial, with a questionable 2-way potential relationship between the 2 entities [12]. A recent systematic review revealed an association between sarcoidosis and malignancy, with an increased risk for hematological, gastrointestinal, and skin cancers [13]. Sarcoidosis may represent a paraneoplastic manifestation of an underlying malignancy [12]. It remains unclear, however, whether a patient with sarcoidosis who develops a sudden flare-up should be screened for an occult malignancy or not [13], as no compelling evidence to support this assumption is currently available [12]. It is also crucial to exclude chronic granulomatous infections, particularly tuberculosis and histoplasmosis in endemic regions, in patients with a history of a clinically silent disease who present with widespread extrapulmonary manifestations, as inappropriate immunosuppression can cause a worsening dissemination of the latter infections [7].
The reviewed literature reported that the pattern of involvement of various organ systems in sarcoidosis depends on a triad of age, sex, and race [4,14]. For instance, hypercalcemia is more common in men older than 40 years, while ocular involvement is more commonly seen in women. Furthermore, hepatic and osseous involvement are more frequent in African Americans [14]; therefore, our patient’s demographic is not much in keeping with the literature, as we describe an extensive osseous and hepatic lesion without symptomatic pulmonary disease in an elderly White patient.
There is no consensus presently for the management of vertebral sarcoidosis owing to the rarity of the disease [15,16]. Medical treatment is reserved for symptomatic patients with pain and bone destruction [4,5,16]. Systemic corticosteroids remain the main modality of treatment of osseous sarcoidosis [15]. The benefits of steroids in bony disease include improvement of skeletal pain and reduction of soft tissue swelling, but they do not completely reverse bony abnormalities [5]. Furthermore, long-term treatment for resistant osseus disease includes methotrexate, hydroxychloroquine, and anti-tumor necrosis factor therapy [15]. Interestingly, a spontaneous resolution of vertebral sarcoidosis was described in the 2 cases that documented a radiological resolution of the previously reported vertebral lesions without medical intervention [16,17].
Conclusions
Sarcoidosis is a chronic granulomatous inflammatory disease that can affect almost any organ system. It predominantly affects the lungs, skin, and lymph nodes, and the subclinical involvement of other organ systems is not uncommon. Nevertheless, the presentation with a clinically apparent multisystem disease with disseminated vertebral and visceral lesions, as reported in our patient, is rare. Clinical and radiological features of vertebral sarcoidosis can be almost indistinguishable from metastatic bone diseases and multiple myeloma. The possibility of widespread extrapulmonary sarcoidosis should be considered in any patient with a remote history of clinically silent sarcoidosis who experiences simultaneous onset of unexplained multisystem-related symptoms.
Figures
References:
1.. Baughman RP, Teirstein AS, Judson MA, Case Control Etiologic Study of Sarcoidosis (ACCESS) research group. Clinical characteristics of patients in a case control study of sarcoidosis: Am J Respir Crit Care Med, 2001; 164(10 Pt 1); 1885-89
2.. Johns CJ, Michele TM, The clinical management of sarcoidosis. A 50-year experience at the Johns Hopkins Hospital: Medicine (Baltimore), 1999; 78(2); 65-111
3.. Judson MA, Boan AD, Lackland DT, The clinical course of sarcoidosis: Presentation, diagnosis, and treatment in a large white and black cohort in the United States: Sarcoidosis Vasc Diffuse Lung Dis, 2012; 29(2); 119-27
4.. Abdallah MA, Ellithi M, Sharma R, The sudden development of multi-organ lesions in a patient with pulmonary sarcoidosis: A case report: J Investig Med High Impact Case Rep, 2019; 7; 2324709619836139
5.. Packer CD, Mileti LM, Vertebral sarcoidosis mimicking lytic osseous metastases: Development 16 years after apparent resolution of thoracic sarcoidosis: J Clin Rheumatol, 2005; 11(2); 105-8
6.. Wessendorf TE, Bonella F, Costabel U, Diagnosis of sarcoidosis: Clin Rev Allergy Immunol, 2015; 49(1); 54-62
7.. Spagnolo P, Sarcoidosis: A critical review of history and milestones: Clin Rev Allergy Immunol, 2015; 49(1); 1-5
8.. Mehrotra P, Muller M, Higgins B, Zammit-Maempel I, An unusual cause of widespread lytic bone lesions caused by sarcoidosis: J Radiol Case Rep, 2011; 5(9); 1-7
9.. Bel-Ange A, Tal S, Rapoport M, A rare case of spinal sarcoidosis presenting as multiple bone marrow oedematous lesions: Eur J Case Rep Intern Med, 2018; 5(8); 00907
10.. Mangino D, Stover DE, Sarcoidosis presenting as metastatic bony disease. A case report and review of the literature on vertebral body sarcoidosis: Respiration, 2004; 71(3); 292-94
11.. Herráez-Albendea MM, Jarilla-Fernández MC, Sarcoidosis-lymphoma syndrome: Reumatol Clin, 2017; 13(6); 365
12.. Mahmood R, Al Banaa K, Ibrahim I, Sarcoidosis vs. colon cancer metastasis: Diagnostic dilemma and the role of PET scan in monitoring disease activity: Case Rep Rheumatol, 2021; 2021; 5529523
13.. Bonifazi M, Bravi F, Gasparini S, Sarcoidosis and cancer risk: Systematic review and meta-analysis of observational studies: Chest, 2015; 147(3); 778-91
14.. Judson MA, Boan AD, Lackland DT, The clinical course of sarcoidosis: Presentation, diagnosis, and treatment in a large white and black cohort in the United States: Sarcoidosis Vasc Diffuse Lung Dis, 2012; 29(2); 119-27
15.. Gibson GJ, Prescott RJ, Muers MF, British Thoracic Society Sarcoidosis study: Effects of long term corticosteroid treatment: Thorax, 1996; 51(3); 238-47
16.. Rahmouni S, Maatallah K, Ferjani H, Spontaneous improvement of sarcoidosis mimicking a vertebral metastatic lesion: It’s indeed possible!: Clin Case Rep, 2020; 8(12); 2423-28
17.. Johnson AK, Johnson JM, Ames E, Filippi C, Spontaneous clinical and radiological resolution of vertebral sarcoidosis: A case report: Spine (Phila Pa 1976), 2012; 37(6); E414-16
Figures
Tables
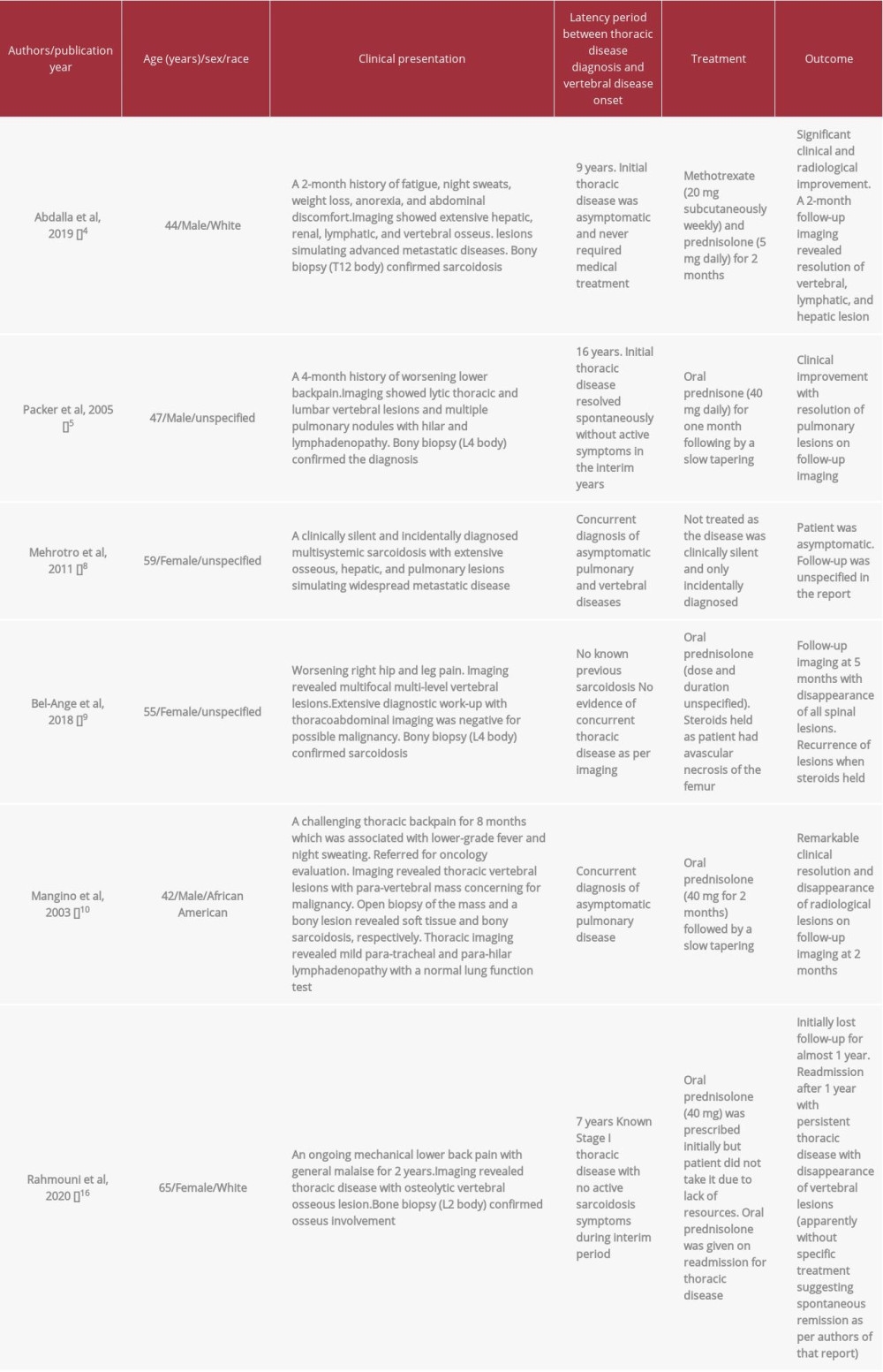 Table 1.. Summary of patient characteristics and clinical features of cases of multisystemic sarcoidosis with vertebral osseous disease in the literature.
Table 1.. Summary of patient characteristics and clinical features of cases of multisystemic sarcoidosis with vertebral osseous disease in the literature.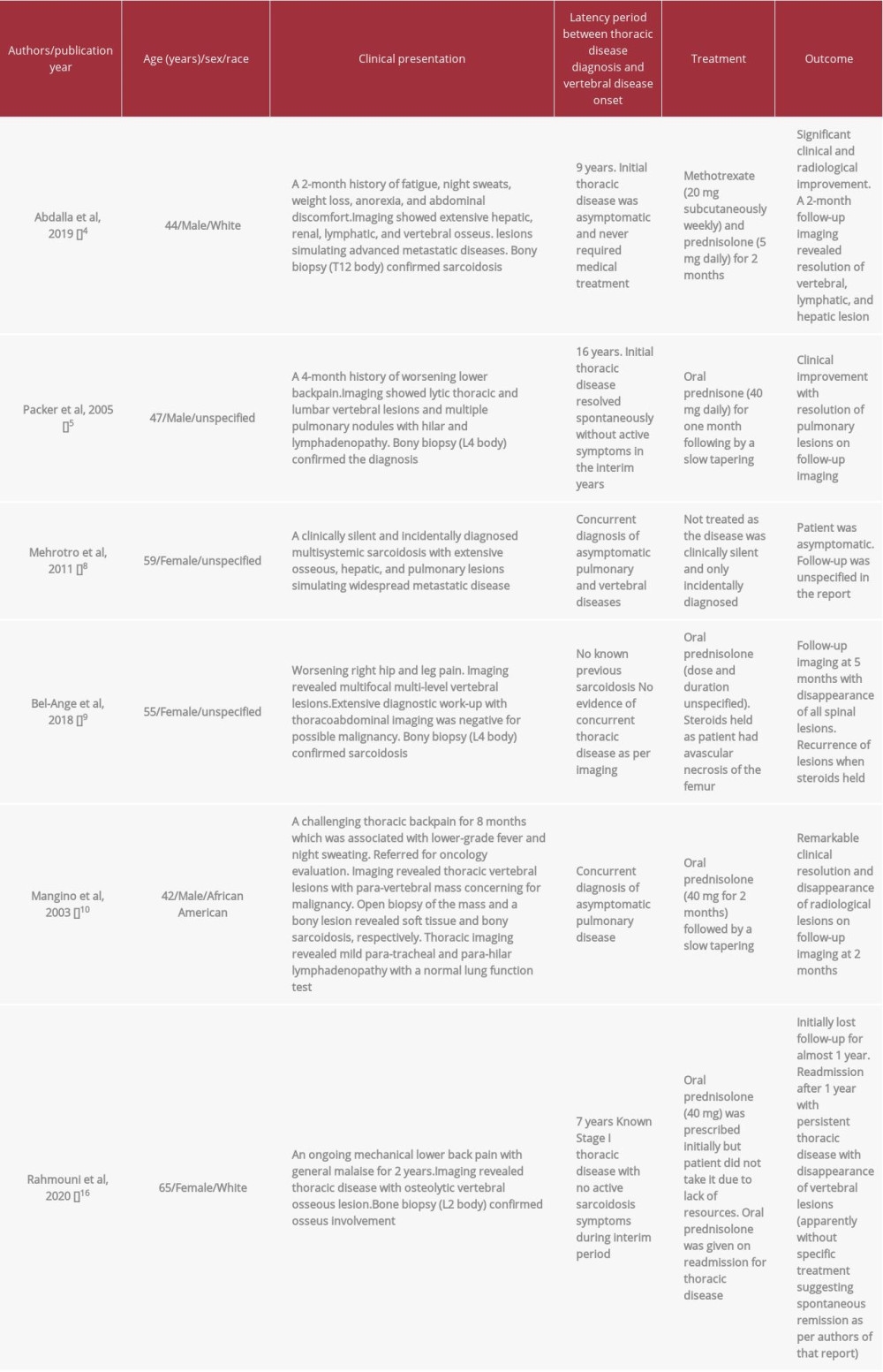 Table 1.. Summary of patient characteristics and clinical features of cases of multisystemic sarcoidosis with vertebral osseous disease in the literature.
Table 1.. Summary of patient characteristics and clinical features of cases of multisystemic sarcoidosis with vertebral osseous disease in the literature. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








