27 June 2022: Articles 
A Rare Case of Extended Retroperitoneal Biloma Due to Spontaneous Perforation of Common Bile Duct, Mimicking a Strangulated Right Inguinal Hernia: A Case Report and Literature Review
Challenging differential diagnosis, Rare disease
Ioannis G. GkionisDOI: 10.12659/AJCR.936255
Am J Case Rep 2022; 23:e936255
Abstract
BACKGROUND: Biloma is the collection of bile outside the biliary tree as a result of visceral perforation. The most common site of disruption is the gallbladder, whereas common bile duct lesions usually occur following medical procedures or trauma. Spontaneous perforation of the common bile duct has been previously reported in the literature. Retroperitoneal biloma secondary to spontaneous perforation of the common bile duct is an extremely rare pathological entity. The purpose of this report is to inform clinical doctors of this rare entity, which can have fatal consequences for the patient.
CASE REPORT: We present the case of an 89-year-old man who was hospitalized with symptoms of vomiting, nausea, fatigue, and diffuse abdominal pain. The clinical examination and blood tests revealed peritonitis, a finding which was confirmed by the computed tomography of the abdomen as a retroperitoneal fluid collection, extending from the region posterior to the duodenum and head of the pancreas to the right inguinal fossa. As the patient’s clinical status deteriorated, an urgent laparotomy was performed, revealing the presence of retroperitoneal biloma secondary to spontaneous perforation of the common bile duct. The operation was never completed as the patient died during the operation.
CONCLUSIONS: The diagnosis of this entity is difficult and is made during surgery. A large spectrum of treatment approaches has been used, but, regardless of the method, the goal is to halt the spreading abdominal contamination with bile and to treat the associated biliary pathology.
Keywords: Common Bile Duct, Retroperitoneal Space, spontaneous perforation, Surgical procedure, Aged, 80 and over, Bile, Hernia, Inguinal, Humans, Male
Background
Biloma is the collection of bile outside the biliary tree and can be either encapsulated or not. Gould and Patel first used the term in 1979 describing an abdominally entrenched bile collection [1]. The formation of biloma is the result of a lesion in the biliary tree, which can be either intrahepatic or extrahepatic [2]. As a consequence, biloma can be intrahepatic, peritoneal, or retroperitoneal [2], with the latter being the most uncommon [2].
The most common site of lesion is the gallbladder [3]. Injury to the common bile duct mostly occurs after surgical, endoscopic, or traumatic interventions, although spontaneous perforation has also been reported [4–25]. This condition is extremely rare in adults, occurring more often in children, due to congenital anomalies [4–6,11,12].
Satake, in 1985, was the first to describe a retroperitoneal collection of bile secondary to spontaneous perforation of the common bile duct [8]. To date, 7 cases have been published in the literature, reporting retroperitoneal biloma due to spontaneous perforation of the common bile duct [8,10,15–18,25].
The diagnosis of this pathological entity is difficult and the main diagnostic modalities for evaluation are abdominal ultra-sound and computed tomography of the abdomen [1,2,4,9,25]. Despite these efforts, the diagnosis is usually made during surgery [1,2,4,9,25].
We present the case of an 89-year-old man with a retroperito-neal biloma with considerable extension; as a consequence, a mass was detectable in the right inguinal region, mimicking a strangulated right inguinal hernia. The patient was treated via urgent laparotomy, and spontaneous perforation of the common bile duct was identified.
Case Report
We present the case of an 89-year-old man who was admitted to the hospital with symptoms of vomiting, nausea, fatigue, and diffuse abdominal pain. The symptoms began 6 days before his admission. His vital signs on admission were: temperature=36.7ºC, heart rate=113 bpm, respiratory rate=25 bpm, and blood pressure=113/70 mmHg, SpO2=97%. The patient was pale but with good nutritional status (body mass index=24 kg/m2).
The medical history of the patient included high blood pressure, dyslipidemia, and chronic obstructive pulmonary disease. His medications were amlodipine for regulation of high blood pressure, statin for treatment of dyslipidemia, and budesonide for management of chronic obstructive pulmonary disease. He had no history of previous surgical interventions and he did not consume alcohol or tobacco, and he had no history of abdominal or thoracic trauma.
On inspection, he was ill-looking and demonstrated signs of dehydration. The clinical examination revealed sensitivity and tenderness in all abdominal quadrants, with bowel sounds being absent. On digital rectal examination, there was no blood or palpable mass detectable. The clinical examination of cardiopulmonary and urogenital systems revealed no abnormal signs, and, apart from a feeling of fatigue, there were no other findings of physical and neurological examinations. Additionally, in the right inguinal fossa and scrotum there was a mass, giving the impression of a strangulated right inguinal hernia, but without elicited pain on palpation.
The blood tests revealed elevated inflammatory markers (WBC: 47.150/mL with normal values 3.800–10.500/mL and CRP 44.25 mg/dL with normal values <0.05 mg/dL), jaundice (TA-BIL: 3.5 mg/dL with normal values 0.3–1.2 mg/dL and D-BIL: 2.41 mg/dL with normal values between 0–0.5 mg/dL), as well as deterioration of the renal and liver functions (Ur: 57 mg/dL with normal values 15–50 mg/dL, Cr: 1.49 mg/dL with normal values 0.7–1.3 mg/dL, GGT: 139 U/L with normal values 0–50 U/L and ALP: 162 U/L with normal values 40–150 U/L). The results of all other laboratory markers were within normal range (Table 1). The blood cultures were negative for bacterial growth.
Taking into consideration all findings from the clinical examination and the blood tests, an abdominal X-Ray was performed, which was not diagnostic, followed by ultrasound of the abdomen and the right inguinal region. The former depicted cholelithiasis, without signs of inflammation or perforation of the gallbladder, and choledocholithiasis with normal diameter of the common bile duct (0.9 cm), while the latter revealed a fluid collection in the right inguinal region and scrotum. The abdominal computed tomography confirmed these findings, additionally detecting a retroperitoneal fluid collection (Figures 1, 2). The collection was extending from the space dorsally to the duodenum and the head of the pancreas to the right inguinal region through Told’s and Gerota’s fascia, and right iliopsoas muscle (Figure 3). Furthermore, the liquid was extending into the right inguinal canal where there was no omentum, mesenteric fat, or part of the bowel detected (Figure 4).
Deterioration of the patient’s clinical status with symptoms of vomiting, exacerbation of abdominal pain, and hemodynamic instability led to an urgent laparotomy with a midline incision 3 h after his admission to the hospital. The gallbladder was intact and there were no significant findings in the peritoneal cavity. A palpable mass was recognized at the right retroperitoneal space. The mobilization of ascending colon, hepatic angle and right mesocolon released substantial amount of green fluid, which was sent for biochemical and microbial analysis (Table 2). Through a Kocher’s maneuver, the space located posteriorly to the duodenum and head of the pancreas was exposed and a small lesion of the common bile duct was detected. The operation was never completed because the patient had cardiorespiratory arrest with subsequent unsuccessful resuscitation, and he died. Taking into account that the patient did not have any known coronary artery disease, we assume that sepsis was the main contributor to cardiorespiratory arrest.
Discussion
The most common site of perforation in the biliary tree, leading to the formation of a biloma, is the gallbladder [3]. The causes are typically cholelithiasis and cholecystitis [3]. McWilliams was the first to report 114 cases of perforation in the biliary tree in 1912 [21]. Most of these cases were in the gallbladder, 4 of them in the common bile duct, and 1 in the hepatic duct [21].
Injury to the common bile duct happens mostly after medical interventions or trauma, but a few cases of spontaneous perforation have been described [4–25]. It is a rare condition and the first to describe a non-traumatic perforation of the bile duct was Freeland in 1882 [13]. Chu reported 7 cases in 1984 and Kang another 11 in 2004 of spontaneous disruption of the common bile duct [4,14]. To our knowledge, these are the 2 largest series of non-traumatic perforation of the common bile duct ever to be reported.
Several propositions have been made for the pathogenesis of this entity [3,9,10,14]. The most widespread is the increased intraductal pressure due to obstruction caused by gallstones, tumor, or reflux spasm of the sphincter of Oddi [3,9,10,14]. Other possible explanations include intramural infection of the common bile duct as a result of cholangitis, thrombosis of a mural vessel leading to necrosis of the affected part, diverticulitis of the common bile duct, acute pancreatitis, parasitic infections, and regurgitation of pancreatic secretions into the common bile duct [3,9,10,14].
If the site of perforation leads to the retroperitoneal space, a retroperitoneal bile collection will develop. A retroperito-neal biloma occurs as a result of bile tracking along the embryological fascial planes, with only 13 cases being reported [3,7,8,10,15–20,23–25]. To date, only 7 cases of a retroperitoneal biloma following spontaneous perforation of the common bile duct have been described in the literature [8,10,15–18,25] (Table 3).
In our case, the biloma was so extended that a mass in the right inguinal region, mimicking a strangulated right inguinal hernia was developed. This is an extremely rare condition. Only 1 similar case has ever been reported [16]. Brady in 2006 described a palpable mass in the right inguinal fossa in a 73-year-old man with a retroperitoneal biloma [16]. In some of these cases, the surgeons could not identify the exact site of perforation, despite an extensive examination [10,16,18]. The diagnosis of spontaneous perforation of the common bile duct was made during the surgical procedure from indirect evidence such as the site of biloma and the integrity of the gall-bladder [10,16,18].
In the management of a retroperitoneal biloma due to perfo-ration of the common bile duct, various approaches have been described and a large spectrum of methods have been used [4,8–10,12,15–18,22,25]. The goals are to halt the spreading abdominal contamination with infected bile and to treat the associated biliary pathology [12]. The most frequent treatments to be reported are intraoperative drainage of the collection, ductal exploration, and T-tube intubation. An endoscopic approach using endoscopic retrograde cholangiopancreatography and percutaneous catheter drainage have also been used [4,8–10,12,15–18,22,25].
Conclusions
We report a rare case of retroperitoneal biloma following spontaneous perforation of the common bile duct. The diagnosis of this pathological entity is difficult and the management remains controversial. Having a high level of suspicion, performing appropriate imaging tests, and offering definitive treatment for this life-threatening condition as soon as possible is the only way to increase patient’s chances for survival.
Figures
Tables
Table 1.. Blood test results on admission. Table 2.. Laboratory findings of the retroperitoneal fluid.
Table 2.. Laboratory findings of the retroperitoneal fluid.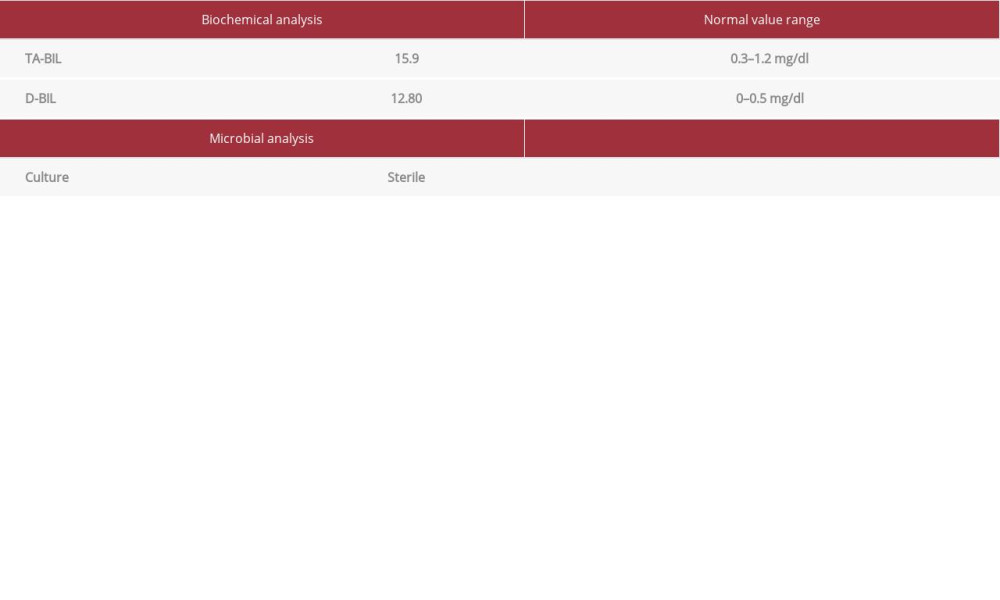 Table 3.. Comparison of the 7 cases with retroperitoneal biloma due to spontaneous perforation of the common bile duct, regarding the site of perforation and management. All 7 cases had cholelithiasis.
Table 3.. Comparison of the 7 cases with retroperitoneal biloma due to spontaneous perforation of the common bile duct, regarding the site of perforation and management. All 7 cases had cholelithiasis.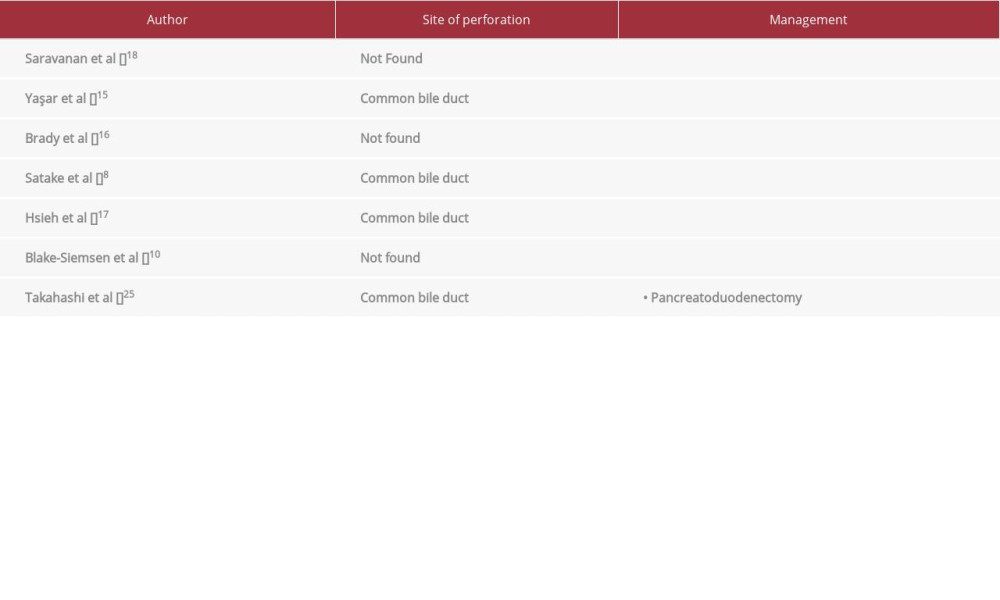
References:
1.. Gould L, Patel A, Ultrasound detection of extrahepatic encapsulated bile: “Biloma”: Am J Roentgenol, 1979; 132; 1014-15
2.. Copelan A, Bahoura L, Tardy F, Etiology, diagnosis, and management of bilomas: A current update: Tech Vasc Interv Radiol, 2015; 18; 236-43
3.. Ishii K, Matsuo K, Seki H, Retroperitoneal biloma due to spontaneous perforation of the left hepatic duct: Am J Case Rep, 2016; 17; 264-67
4.. Kang SB, Han HS, Min SK, Lee HK, Nontraumatic perforation of the bile duct in adults: Arch Surg, 2004; 139; 1083-87
5.. Hasegawa T, Udatsu Y, Kamiyama M, Does pancreatico-biliary maljunction play a role in spontaneous perforation of the bile duct in children?: Pediatr Surg Int, 2000; 16; 550-53
6.. Davenport M, Heaton ND, Howard ER, Spontaneous perforation of the bile duct in infants: Br J Surg, 1991; 78; 1068-70
7.. Cólović R, Perisić-Savić M, Retroperitoneal biloma secondary to operative common bile duct injury: HPB Surg, 1991; 3; 193-97
8.. Satake K, Ikehara T, Shim K, A large retroperitoneal encapsulation of bile from a spontaneous perforation of the common bile duct: Am J Gastroenterol, 1985; 80; 279-83
9.. Faridi SH, Aslam M, Siddiqui B, Khan RA, Challenges in the diagnosis and management of spontaneous bile duct perforation: A case report and review of literature: J Indian Assoc Pediatr Surg, 2015; 20; 143-45
10.. Blake-Siemsen JC, Kortright-Farias M, [Spontaneous retroperitoneal biloma: A case report.]: Cir Cir, 2017; 85; 552-56 [in Spanish]
11.. Khanna R, Agarwal N, Singh AK, Spontaneous common bile duct perforation presenting as acute abdomen: Indian J Surg, 2010; 72; 407-8
12.. Paladugu R, Rau A, Schein M, Wise L, Spontaneous perforation of the hepatic duct in adults: Dig Surg, 1998; 15; 417-20
13.. Freeland J, Rupture of the hepatic duct: Lancet, 1882; 1; 731-32
14.. Chu CS, Spontaneous perforation of the common hepatic duct: report of seven cases: Surg Gastroenterol, 1984; 3; 69-76
15.. Yaşar NF, Yaşar B, Kebapçı M, Spontaneous common bile duct perforation due to chronic pancreatitis, presenting as a huge cystic retroperitoneal mass: A case report: Cases J, 2009; 2; 6273
16.. Brady RRW, McAteer E, Weir CD, Biliscrotum and retroperitoneal biloma: Spontaneous rupture of the biliary system presenting as an incarcerated inguinal hernia: Ulster Med J, 2006; 75; 85-87
17.. Hsieh TJ, Chiang IC, Kuo KK, Spontaneous retroperitoneal biloma: A case report: Kaohsiung J Med Sci, 2002; 18; 412-16
18.. Saravanan B, Ahiaku EK, Gash A, An unusual cause of right perirenal collection: Eur J Radiol, 2007; 62; 53-55
19.. Kaushik R, Attri AK, Choleretroperitoneum – an unusual complication of cholelithiasis: Indian J Surg, 2004; 66; 358-60
20.. Horovitz L, Spontaneous retroperitoneal perforation of the gallbladder: Int Surg, 1975; 60; 235-36
21.. McWilliams CA, Acute, spontaneous perforation of the biliary system into the free peritoneal cavity: A report of six cases from the Presbyterian hospital of New York and 108 cases from the literature: Ann Surg, 1912; 55; 235-63
22.. Mason JC, Babbs C, Lee SH, Connolly MJ, Spontaneous biloma in an elderly patient: Postgrad Med J, 1993; 69; 740-42
23.. Neoptolemos JP, Harvey MH, Slater ND, Carr-Locke DL, Abdominal wall bile staining and ‘biliscrotum’ after retroperitoneal perforation following endoscopic sphincterotomy: Br J Surg, 1984; 71; 684
24.. Bui BT, Oliva VL, Ghattas G, Percutaneous removal of a biliary stent after acute spontaneous duodenal perforation: Cardiovasc Intervent Radiol, 1995; 18; 200-2
25.. Takahashi K, Okabe Y, Orino A, Spontaneous rupture of a biliary diverticulum in the distal common bile duct, with formation of a retroperitoneal biloma: Gastrointest Endosc, 2005; 61; 783-87
Figures
Tables
 Table 1.. Blood test results on admission.
Table 1.. Blood test results on admission.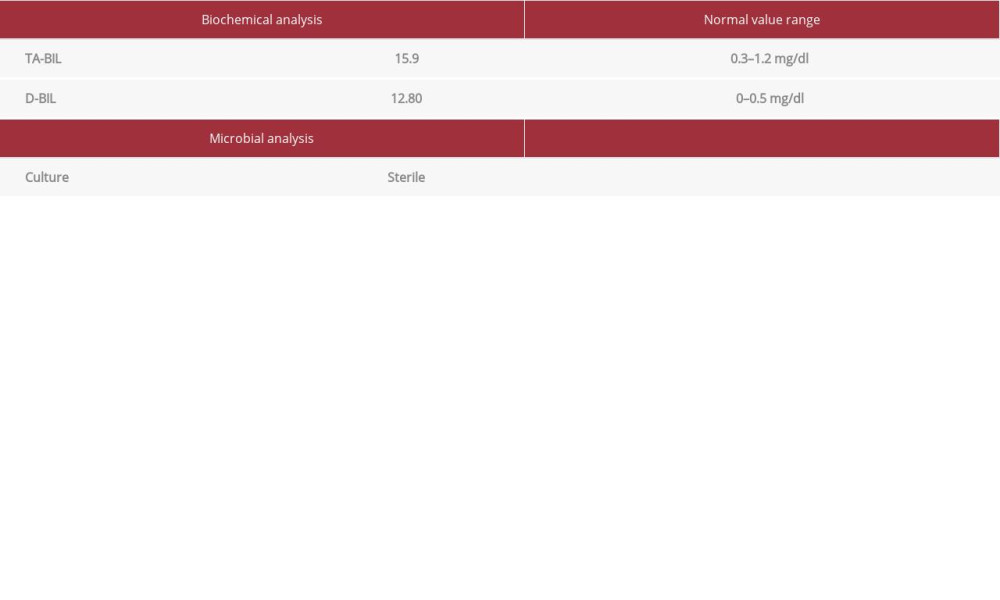 Table 2.. Laboratory findings of the retroperitoneal fluid.
Table 2.. Laboratory findings of the retroperitoneal fluid.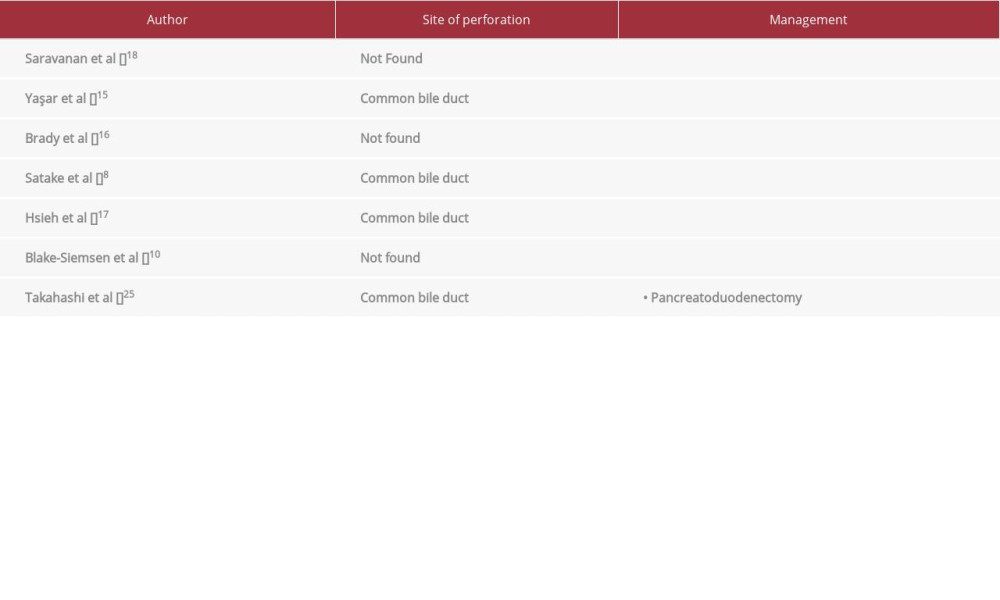 Table 3.. Comparison of the 7 cases with retroperitoneal biloma due to spontaneous perforation of the common bile duct, regarding the site of perforation and management. All 7 cases had cholelithiasis.
Table 3.. Comparison of the 7 cases with retroperitoneal biloma due to spontaneous perforation of the common bile duct, regarding the site of perforation and management. All 7 cases had cholelithiasis. Table 1.. Blood test results on admission.
Table 1.. Blood test results on admission.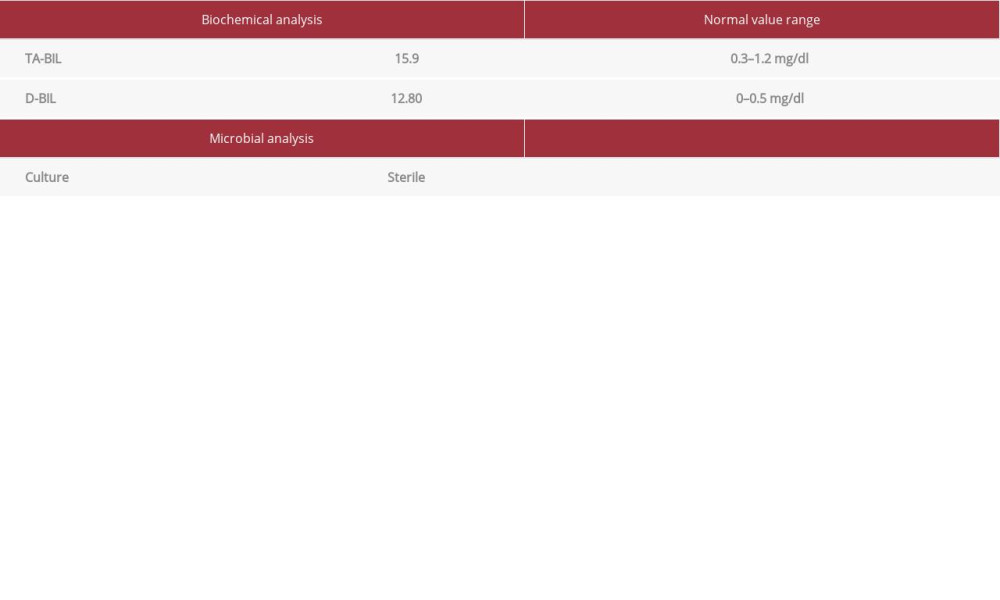 Table 2.. Laboratory findings of the retroperitoneal fluid.
Table 2.. Laboratory findings of the retroperitoneal fluid.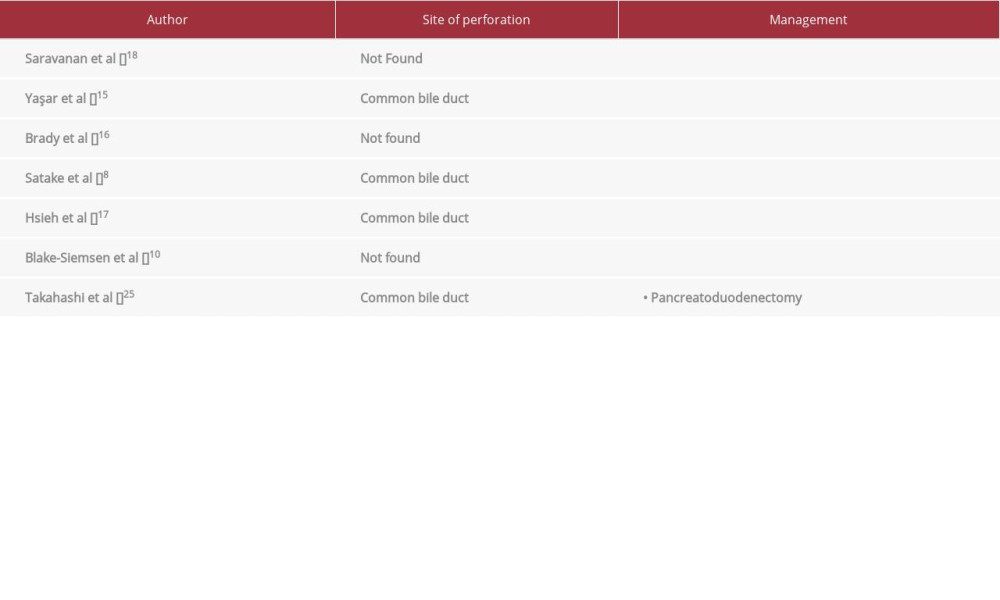 Table 3.. Comparison of the 7 cases with retroperitoneal biloma due to spontaneous perforation of the common bile duct, regarding the site of perforation and management. All 7 cases had cholelithiasis.
Table 3.. Comparison of the 7 cases with retroperitoneal biloma due to spontaneous perforation of the common bile duct, regarding the site of perforation and management. All 7 cases had cholelithiasis. In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








