30 November 2022: Articles 
Long-Term Retrograde Global Amnesia Following Minor Trauma
Unusual clinical course, Challenging differential diagnosis
Christina Stilling1EF*, Balázs Pazdera1CD, Annette Bennedsgaard Jespersen2B, Tue Hartmann1BC, Andreas Halgreen EisetDOI: 10.12659/AJCR.937845
Am J Case Rep 2022; 23:e937845
Abstract
BACKGROUND: Retrograde amnesia has several causes and may be the core concern in several conditions. When acute, somatic, and neurologic causes are excluded, along with substance use, a consideration of psychiatric disease is imminent. Here, we present a case with amnesia, where diagnostics and treatment were challenging due to severe psychiatric symptoms and course of the disease.
CASE REPORT: After a minor trauma while driving an electric scooter, a 41-year-old man lost all memories of the past 20 years. The patient was raised in a refugee camp, where he experienced traumatic events, and later came to Denmark and established family and work life. He had 1 prior contact with the psychiatric ward. After the incident, the patient was brought to the emergency room. The patient could not recognize his wife or children and believed he was 21 years old and living with his mother in the refugee camp. A full somatic and neurological workup was performed and no somatic or organic cause could explain the retrograde amnesia. He developed post-traumatic stress disorder (PTSD) and psychotic symptoms. Treatment consisted of a combination of psychoeducation, cognitive remediation, and medical treatment for psychotic symptoms and PTSD.
CONCLUSIONS: The diagnosis “prolonged delirium”, “PTSD”, and “dissociative amnesia” were considered. Psychiatric comorbidity and previous traumatic experiences might have contributed to the development of long-term amnesia, which eventually was considered to be dissociative. During 8 months, the patient slowly regained his memory. It is impossible to conclude with certainty whether the successful outcome was the result of psychological treatment, pharmacological treatment, the passing of time, or a mixture of these.
Keywords: Amnesia, Amnesia, Retrograde, Delirium, Psychological Trauma, Stress Disorders, Post-Traumatic, Child, Male, Female, Humans, Adult, young adult, Emergency Service, Hospital, Mothers
Background
Memory loss or retrograde amnesia has several origins and may be the core concern in several conditions. We present this case to help in the evaluation and treatment of sudden, severe global amnesia, in which somatic causes eventually were excluded and severe psychiatric symptoms, post-traumatic stress syndrome (PTSD), and psychotic symptoms made diagnosis and treatment challenging. Below, we give a short introduction to some of the most common conditions which were considered during the investigation.
The most important causes of amnesia with acute onset are brain damage due to stroke, tumors, encephalitis, and concussion. Neurological causes include transient epileptic amnesia, global transient amnesia, and dementia, but the latter rarely has an acute onset. Transient global amnesia is defined as a sudden onset of an anterograde and retrograde amnesia that lasts up to 24 h, predominately in individuals older than 50 years of age. Mild subclinical neuropsychological deficits can last for days after the event [1]. Transient epileptic amnesia involves amnestic episodes, often when awake and at a frequency of around once a month, typically lasting 15–30 min [2].
In cases of substance use and delirium in which cognitive function is diminished, the course is usually fluctuating, whereas with organic amnestic disorder, cognitive function usually is intact (ICD 10, F04, and F05) [3]. Dissociative disorders have several subcategories, with amnesia as a diagnostic criterion. Dissociative amnesia is loss of memory, usually of important recent events, that is not due to an organic mental disorder, and is too significant to be explained by ordinary forgetfulness or fatigue. The amnesia is usually centered on traumatic events, and is usually partial and selective (ICD-10, F44.0) [3]. Complete and generalized amnesia is rare and usually part of dissociative fugue (ICD-10, F44.1) [3]. Dissociative amnesia is often diagnosed in individuals aged 20–40 years [4] and with comorbid psychiatric disease, especially depression, family or relationship difficulties, exposure to psychological stress [5,6], and substance abuse [6]. Published case reports on memory loss vary from complete autobiographic and semantic memory to only memory loss of a few days or periods of life [5–7]. A large gap in memory without recognition of close family has been described in several case reports [5,7], as well as dissociative amnesia and psychotic symptoms, where the patient afterwards was diagnosed with schizophrenia [8]. The new classification in ICD-11 (not yet implemented) has generalized amnesia included in dissociative amnesia (ICD-11, 6B61) [9], and dissociative reactions and symptoms are included in the diagnosis complex post-traumatic stress syndrome (ICD-11, 6B41) [9]. In DSM-5, dissociation is described in the diagnosis PTSD [10], where the amnesia characteristically is related to the traumatic events.
Patients with retrograde amnesia form a heterogeneous group and our patient had similarities with patients described in many published case reports with experienced trauma, a psychiatric history, and a triggering event. However, the amnesia is often the core problem, and neuropsychological tests, causality, and treatment are directed towards this. In the present case, the patient developed PTSD and psychotic symptoms, which also had to be considered. The patient had no memories from the stable and peaceful period of his life but solely memories from his upbringing in a refugee camp with various traumatic events. The entire process, with triggering event, amnesia, and subsequent psychiatric symptoms, is an interesting case to share with other clinicians who may encounter a similar case in the future.
Case Report
After a minor trauma, a 41-year-old man lost all his memories of the past 20 years and during the next 8 months slowly regained most memories. He was raised in a refugee camp in the Middle East. In the refugee camp he experienced war and bombings and he spent time in jail, where he was exposed to beatings and torture. He came to Denmark in 2000, aged 21 years, where he married and fathered 2 children. He had various jobs and during the past 12 years he worked full time as a janitor and was fluent in Danish.
The patient was brought to the emergency room after a low-energy trauma when he was hit by a car while he was driving an electric scooter. The car was slowly backing up and he was pushed onto the road from the sidewalk. He was conscious during the incident and there was no report of a blow to the head. In the ambulance, he reported having pain in the neck and back. He was alert and oriented (Glasgow Coma Scale score of 15) in the ambulance and at the arrival to the emergency room, but during the somatic examination he was confused and disoriented. Suddenly, he could not speak or understand Danish, only his mother tongue, Arabic. He believed he was in his home country, 21 years old, and living with his mother. He did not recognize his wife or children, nor being married or having children at all. His mother, still living in the home country, was contacted to ensure him that the woman was his wife and that she was a “good person”.
The patient had a medical history, including a single prior contact with the psychiatric ward 10 years prior, where he developed psychotic symptoms with imperative hallucinations, paranoia, and suicidal thoughts some months after losing his job. The paranoia manifested itself as suspicion that people wanted to harm him and his family and he felt chased by cars when in traffic. He heard a voice telling him to hang himself and drive into a truck while in his car. He carried on conversations with the voice, and his wife was frightened by this and travelled with their children to their home country. He was initially treated by his general practitioner and thereafter was admitted to a psychiatric ward and discharged after 20 days with the diagnosis adjustment disorder. He had no follow-up at the psychiatric ward and there were no records of his well-being in the interim period. According to his wife, he had experienced nightmares for many years and was affected by previous traumas from his upbringing in the refugee camp. He talked to his wife about these traumas. In spite of previous experiences, the family had a good life and he had a stable job and was well-liked. The only psychological strain was around 4–5 months prior to the incident described in this case report when his wife was diagnosed with a benign tumor and was operated on a couple of months thereafter. According to his wife, this had caused worry, as the operation could cause minor paralysis.
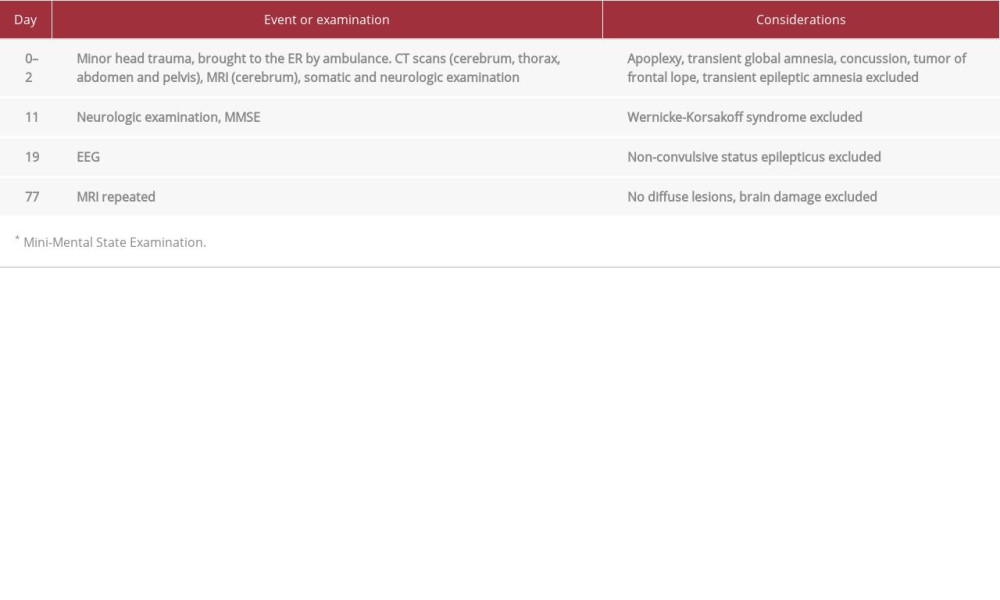
When the patient arrived in the emergency room, a full somatic and neurologic workup was performed, including scans and computed tomography (CT) on day 0 in the trauma center, magnetic resonance imaging (MRI) on day 1, and an electroencephalogram (EEG) on day 19 (Table 1). All the examinations were normal. On day 11, he was tested with a Mini-Mental State Examination (MMSE), with a score 15/30, which was not considered valid because he was illiterate. He scored 4/10 on orientation to time and place, was able to repeat 3 words, and recall 2 of the words. He scored 1/5 on attention/concentration and calculating, 5/8 on language skills, and 0 in the visuo-spatial task. Parts of the examination were repeated on day 54, where he had trouble participating in and understanding the tasks. When presented with 3 words, including ‘apple’, he thought he would be given one. A lumbar puncture was never performed, as the patient declined the procedure. Instead, a blood test for autoimmune encephalitis was performed and was negative. Standard blood samples were normal and a urine drug screen was negative for all substances. There was no history of alcohol or substance abuse. A repeated MRI scan on day 77 was collectively evaluated with the neurosurgical department and showed no abnormalities, especially no diffuse lesions (Table 1).
The first day after the incident and the ensuing sudden global amnesia, he was observed to have confusion, anxiety, impairment of short-term memory, and lack of orientation. On day 2, he began recognizing the nurses on the ward and his wife as “the lady who helps him”. He acknowledged that he had a wife and children but did not recognize them. He was sad and tearful during conversations with personnel at the ward. He was discharged on day 4 with the diagnosis ‘Reaction to severe stress, unspecified’ (F43.9 ICD10) [3] because it was believed he would regain memories in familiar surroundings and have a follow-up at his general practitioner. Instead, he was readmitted to the psychiatric ward on day 13 due to anxiety and paranoid delusions. He believed the mafia was watching him and wanted to take his organs. He was afraid of people around him and that the hospital staff were part of the mafia. His last memory was dying and being put in a freezer and waking up in Denmark. He did not recognize himself in the mirror. He developed visual and hearing hallucinations, in which he interacted and talked with his friend Ali, a deceased person whom he used to work with in the refugee camp. Most of the time he was polite and kept to himself in his room. He was disoriented and at times he could not be corrected in his belief of being 20 years old and living with his mother. A few times he was observed to be anxious, and acted as if he was a prisoner in a cell. During a home visit, his wife reported that he was irritable and mistrustful. He was prescribed the same kind of antipsychotic medicine he was treated with 10 years prior, and was discharged on day 27, with follow-up in an outpatient clinic.
The patient developed symptoms compatible with PTSD, with intrusive memories from past experiences in the refugee camp, nightmares and anxiety, and hypervigilance when he was out walking with his wife. At home he kept on hallucinating and he would sit in his room with the lights off due to fear that airplanes would spot them and bomb the apartment. Treatment in the outpatient clinic was conducted over 6 months and was a combination of psychoeducation, cognitive remediation, and medical treatment for psychotic symptoms and PTSD. The amnesia persisted for a total of 8 months, with gradual recovery of memories. In the first sessions of the psychological treatment, a lifeline was established. Examples of memories from the refugee camp were stories of bombings, where he and Ali afterwards would drive dead people to the hospital for their organs to be sold. He was given psychoeducation on PTSD and his reactions, emotions, and guilt. At first, he was irritable when shown photos from the amnestic period, and when told that ‘Ali’ was a hallucination. He appeared anxious and kept asking if the therapist would hit him, believing that the outpatient clinic was a police station. Gradually, he appeared less anxious and participated more, and was able to share more of his traumatic experiences. After 5 months, he slowly accepted that he was in Denmark and his life in the refugee camp was in the past. The patient had no desire for actual trauma processing, and at the end of the course he distanced himself more emotionally from the severe traumas, although he still had memories of them, including the memory of Ali’s death, which he also accepted at the end. He was exposed to familiar places and to the location where the traumatic incident had happened. He remembered events from his life in Denmark, and after 6 months, he recognized familiar places in Denmark and gradually remembered more Danish words. After 8 months, he understood Danish and his vocabulary was so advanced that the final contact in the outpatient clinic was conducted without an interpreter. He resumed his work as a janitor, and overall psychotic symptoms and PTSD-symptoms gradually declined.
Discussion
In this case the complex combination of amnesia, cognitive impairment, PTSD-symptoms, and psychotic symptoms following a trauma made diagnosis and treatment challenging. The diagnoses “PTSD”, “delirium”, and “dissociative amnesia” were considered.
No structural abnormalities were found on the scans, and as the amnesia persisted past 24 h, the diagnosis transient global amnesia was rejected. The patient did not meet the criteria for transient epileptic amnesia or Wernicke-Korsakoff syndrome. Initially, the main symptoms were amnesia, disorientation, and cognitive impairment and the psychotic symptoms were interpreted as confabulations. Many of his symptoms and interpretations could be explained by his memories at that time, such as believing his organs would be sold at a hospital, due to his prior experiences. It was discussed whether the mild trauma with a possible concussion could have entailed prolonged delirium. We considered treating the delirium with electroconvulsive therapy treatment (ECT), but due to the risk of further deterioration of cognitive functioning and his difficulty in cooperating with the procedure due to paranoia and delusions, it was decided not to follow through. ECT has been reported to successfully treat delirium [11,12], but in-depth research on the subject is sparse. Ultimately, in the presented case, the temporal development and severity of symptoms were unlikely to arise from such a mild trauma. Due to the progression of symptoms, a somatic or organic origin was carefully considered and the patient was evaluated by various departments: Neurosurgical, Neurology, and Neuropsychiatric. Eventually, all somatic diagnoses were ruled out and a psychiatric cause was considered most likely.
The patient did not meet the criteria for schizophrenia and he did not present any symptoms which could imply bipolar disorder, especially no signs of mood swings with elevated or expansive mood or prolonged irritability. His symptoms and prolonged amnesia suggested dissociative amnesia. Most studies on dissociative amnesia concentrate on causalities, background, underlying mechanisms, or neuropsychological profile and very little is known about treatment. Two reviews have shown that pharmacological treatment has been used to treat comorbid depression, but there is no evidence-based treatment for dissociative amnesia, and a variety of hypnosis, hypnotherapy, anxiolytic medications, psychotherapy, and psychoeducation are reported as different approaches to help patients retrieve memories [4,13]. ECT as treatment for dissociative amnesia has been reported in 2 cases, 1 with successful outcome and 1 without relief of symptoms [14,15].
The patient was treated with standard evidence-based pharmacological medicine for PTSD, and second-generation antipsychotics were added for both PTSD and psychotic symptoms. Our patient was prescribed Sertraline and was treated for approximately 2 months, reaching a dose of 100 mg before discontinuation. He failed to comply with treatment with Quetiapine, and it was concluded that it would not have had an impact on the patient’s improvement. No other pharmacological treatment was considered, and would have been speculative. Education about the condition is important [4]. In this case, psychoeducation regarding PTSD and amnesia was provided, including helping the patient create life timeline. The patient’s everyday life was included, and Danish words related to his job as a janitor (especially names of tools) were taught or recognized before more common words like ‘table’. A common treatment for PTSD is trauma-focused psychotherapy, but our patient declined this therapy, and it was not considered as a treatment option due to his condition and the psychotic symptoms.
As part of PTSD, we could expect the traumatic events or periods of his life to be suppressed with occasional elements of flashbacks, instead of the safe and established period of his life being the ‘target’ of his amnesia. In light of the dissociation theory of Pierre Janet [16] and the dissociative state the patient was in, it could make sense that the patient remembered a dysfunctional and traumatic part of his life, when he lived in fear and performed actions he was now ashamed of. He had memories that were difficult to integrate into his current life and self-perception, and he normally repressed these, which is a dissociated self- and psychological defense against his traumatic experiences. A published study on immigration and dissociative amnesia [17] sums up previous theories on how “immigration posed a significant threat to feelings of identity and self-cohesiveness”, which could include our patient. The patient’s amnesia lasted a long time, but many patients retrieve most of their memories or relearn them within days, weeks, or months; however, examples of persistent amnesia are reported [6,8]. Retrograde amnesia due to malingering is seen with criminal offenders and reported in 1 case in a neuropsychological study, where the subject felt need for sanctuary at a hospital and feigned his amnesia [6]. Malingering was considered and could have been tested for with the test of memory malingering (TOMM), but it was determined that the patient would not be able to participate at that time. As the psychopathological symptoms were consistent over time and present across contexts, and the patient would not gain in any way from amnesia, hospital admissions, or outpatient treatment, we can with great certainty exclude that the present case involved malingering.
Conclusions
In the presented case, the patient had a psychiatric history and possible comorbid undiagnosed PTSD, which was expressed simultaneously with retrograde amnesia. This comorbidity and previous traumatic experiences might have contributed to the long-term amnesia and dissociative state. It is impossible to conclude with certainty whether the successful outcome was the result of psychological treatment, pharmacological treatment, the passing of time, or a mixture of these.
References:
1.. Spiegel DR, Smith J, Wade RR, Transient global amnesia: Current perspectives: Neuropsychiatr Dis Treat, 2017; 13; 2691-703
2.. Baker J, Savage S, Milton F, The syndrome of transient epileptic amnesia: A combined series of 115 cases and literature review: Brain Commun, 2021; 3; fcab038
3.. : The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic criteria for research, 1993, Geneva, World Health Organization
4.. Staniloiu A, Markowitsch HJ, Dissociative amnesia: Lancet Psychiatry, 2014; 1; 226-41
5.. Harrison NA, Johnston K, Corno F, Psychogenic amnesia: Syndromes, outcome, and patterns of retrograde amnesia: Brain, 2017; 140; 2498-510
6.. Kritchevsky M, Chang J, Squire LR, Functional amnesia: Clinical description and neuropsychological profile of 10 cases: Learn Mem, 2004; 11; 213-26
7.. Fujiwara E, Brand M, Kracht L, Functional retrograde amnesia: A multiple case study: Cortex, 2008; 44; 29-45
8.. Li K, Yang WT, Perez AG, Man of mystery: A case report of dissociative amnesia in schizophrenia: Cureus, 2021; 13; e20688
9.. : International Classification of Diseases Eleventh Revision (ICD-11), 2019/2021, World Health Organization (WHO) https://icd.who.int/browse11
10.. Shalev A, Liberzon I, Marmar C, Post-traumatic stress disorder: N Engl J Med, 2017; 376; 2459-69
11.. Nielsen RM, Olsen KS, Lauritsen AO, Boesen HC, Electroconvulsive therapy as a treatment for protracted refractory delirium in the Intensive Care Unit – five cases and a review: J Crit Care, 2014; 29; 881.e1-e6
12.. van den Berg KS, Marijnissen RM, van Waarde JA, Electroconvulsive therapy as a powerful treatment for delirium: a case report: J ECT, 2016; 32; 65-66
13.. Brandt J, van Gorp WG, Functional (“psychogenic”) amnesia: Semin Neurol, 2006; 26; 331-40
14.. Kumar S, Rao SL, Sunny B, Gangadhar BN, Widespread cognitive impairment in psychogenic anterograde amnesia: Psychiatry Clin Neurosci, 2007; 61; 583-86
15.. Kosidou K, Lindholm S, A rare case of dissociative fugue with unusually prolonged amnesia successfully resolved by ECT: European Psychiatry, 2007; 22; S264-65
16.. van der Hart O, Horst R, The dissociation theory of Pierre Janet: J Trauma Stress, 1989; 2; 397-412
17.. Staniloiu A, Bender A, Smolewska K, Ganser syndrome with work-related onset in a patient with a background of immigration: Cogn Neuropsychiatry, 2009; 14(3); 180-98
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250