18 October 2022: Articles 
Metolachlor Poisoning with Lactic Acidosis Improved by Thiamine Administration: A Case Report
Unusual clinical course, Unusual or unexpected effect of treatment
Akira Suekane12ABCDE*, Masato Edamoto3BCDEF, Keisuke Kubo24DEF, Tomohiro AbeDOI: 10.12659/AJCR.937873
Am J Case Rep 2022; 23:e937873
Abstract
BACKGROUND: Metolachlor is a chloroacetamide herbicide that is extensively used worldwide. Ingestion of metolachlor causes acute toxicity via the generation of methemoglobin. Elevated levels of methemoglobin inhibit the transport of oxygen to tissue, causing hypoxia and lactic acidosis. A common treatment approach has been to reduce methemoglobin by administration of methylene blue. Herein, we present a case of metolachlor poisoning causing lactic acidosis that was treatable by thiamine administration, in which the methemoglobin level was not elevated.
CASE REPORT: A 61-year-old man was admitted to the emergency room with seizures and impaired consciousness after the ingestion of metolachlor (250 mL, 83%) with the intent to commit suicide. The patient’s methemoglobin and lactate levels on admission were 0.9% and 11.8 mmol/L, respectively. After admission, the levels of lactate decreased gradually; however, they increased 13 h after admission. There was no evidence of heavy alcohol consumption, hyponutrition, or chronic thiamine deficiency. We initially administered a thiamine bolus (100 mg), which immediately improved his consciousness, followed by continuous administration of the same substance (1500 mg/day). The patient’s consciousness improved, and was discharged from the intensive care unit on day 4.
CONCLUSIONS: Metolachlor can cause metabolic dysfunction and lactic acidosis without an increase in methemoglobin. Moreover, thiamine administration may be beneficial for patients with metolachlor intoxication exhibiting symptoms of elevated lactate levels, impaired consciousness, and lack of elevated methemoglobin levels.
Keywords: Metolachlor, thiamine, Male, Humans, Middle Aged, Acidosis, Lactic, Methylene Blue, Methemoglobin, Lactates, Oxygen, Herbicides
Background
Suicide is a major global problem. The World Health Organization estimates that more than 700 000 people die annually due to suicide, accounting for approximately 1.5% of all deaths and among the top 20 causes of death worldwide [1]. Recently, the spread of coronavirus 2019 (COVID19) has caused social anxiety and has led to an increase in psychiatric disorders and suicide attempts among young people [2,3]. Self-ingestion of pesticides is a common suicide method, especially in low- and mid-income countries [4]. The mortality rate of acute drug intoxication has been increasing, and there is a need to consider and classify all these cases to improve treatment methods [5].
Metolachlor, an aniline derivative and a chloroacetamide (chloroacetanilide) herbicide, is extensively used around the world. Metolachlor can be absorbed by the skin and oral mucosa, inhaled, and ingested. It causes relatively mild toxicity effects in humans. Generally, the toxicity of metolachlor is caused by the generation of methemoglobin (MetHb), which contains oxidized iron (Fe3+), cannot transport oxygen, and induces tissue hypoxia. Hypoxia induces anaerobic metabolism and lac-tate production, leading to lactic acidosis. Lactic acidosis can be classified into 2 types: type A with tissue hypoxia, and type B without obvious tissue hypoxia and in practice is often difficult to classify. Acidosis caused by drug-induced abnormalities in cellular metabolism is included in type B. Methylene blue (MB) is a redox agent that reduces MetHb to hemoglobin. MB is an essential treatment in patients with very high MetHb levels [6].
Thiamine is an essential vitamin that acts as a cofactor for some metabolic reactions. Thiamine acts as a coenzyme of pyruvate dehydrogenase, which metabolizes pyruvic acid to acetyl-CoA, a substrate in the tricarboxylic (TCA) cycle. Thiamine deficiency results in adenosine triphosphate impairment as well as sequential accumulation of pyruvic acid and lactic acid; thus, thiamine deficiency is related to lactic acidosis [7]. Thiamine supplementation for lactic acidosis induced by thiamine deficiency is necessary for treatment.
Herein, we report a case of metolachlor intoxication showing marked lactic acidosis and impaired consciousness despite the absence of elevated methemoglobin levels. The patient was successfully treated with the administration of methylene blue and thiamine.
Case Report
This case involves a 61-year-old man with a history of hypertension, no psychiatric history, and no psychiatric genetic predisposition. His family found him lying supine on the floor of his house. He had generalized tonic convulsions that lasted for 10–20 s, followed by 4–5 episodes of vomiting a white mucus-like substance. An open bottle of herbicide (83% metolachlor) was found in the patient’s pocket; thus, herbicide poisoning following a suicide attempt was suspected, although the exact time and ingested amount were unknown. Upon the arrival of emergency medical technicians, the patient was comatose (Glasgow coma scale [GCS], 3). He was transported to our hospital’s emergency room.
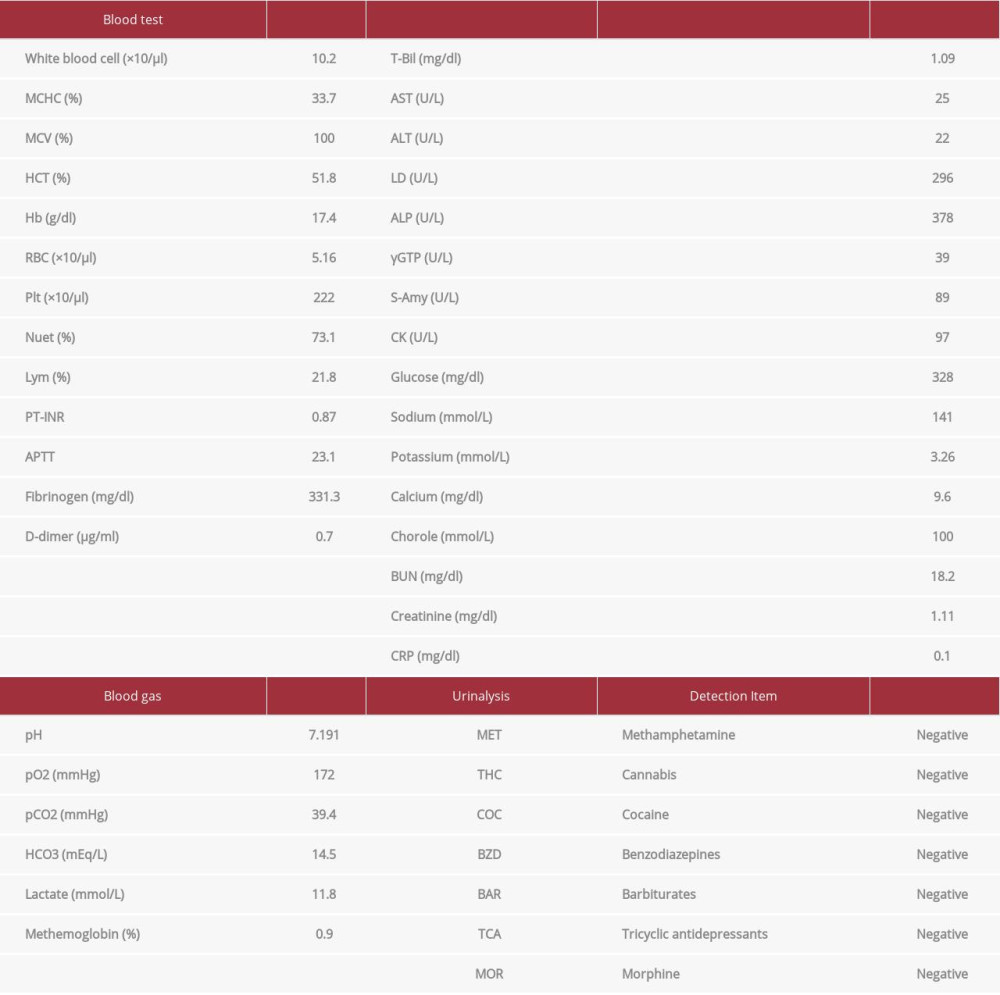
On arrival (7.40 a.m.), his vital signs were: GCS, 6 (E1V1M4); pupils (right/left), 3 mm/4 mm; pupils’ light reflexes were prompt; respiratory rate, 20/min; heart rate, 70 beats per min (bpm); blood pressure, 110/60 mmHg; oxygen saturation, 99% (with O2 10 L/min); and body temperature, 34.4°C. There was no obvious tetraplegia. Blood gas analysis showed metabolic acidosis (pH, 7.191; pCO2, 39.4 mmHg; HCO3, 14.5 mEq/L) with elevated lactate level of 11.8 mmol/L, but low MetHb level of 0.9%. Blood tests showed a mildly elevated leukocytes at 10 200/µL, but no leftward deviation, and no obvious electrolyte abnormalities or hepatic or renal dysfunction. Urinalysis also did not detect poisoning from any other drugs (Table 1). Computed tomography (CT) excluded any abnormalities that can cause obvious disturbance of consciousness. At the time, the patient was in respiratory failure, had impaired consciousness, required ventilatory management, and was at risk for seizures. Since limb movements could be observed during body movements and no findings suggestive of cerebral infarction or central infection were noted, we decided that the benefits of magnetic resonance imaging (MRI) did not outweigh the risks, considering the risk of sudden change during the MRI; therefore, we did not perform MRI at the time. An interview of the family revealed that the patient had not significantly decreased food intake, and there were no blood laboratory findings to suggest malnutrition: body mass index, 25; TP, 7.9 g/dl; and Alb, 4.9 g/dl. Alcohol was occasionally consumed but not on a daily basis. Although the blood alcohol concentration was not directly measured, there was no evidence of an osmotic gap. There was also no evidence of prolonged heavy alcohol intake or hyponutrition, and thiamine levels were not measured. Thus, the patient was diagnosed with metolachlor intoxication, despite the fact that the MetHb level was not elevated.
In the emergency room, he had another generalized tonic seizure. We administered midazolam (5 mg) and performed tracheal intubation. We inserted a nasogastric tube and aspirated the remains of the stomach contents, including a large amount of the white, viscous mucus, with odor and color similar to that of the metolachlor herbicide, which was thought to be in the bottle. We then infused activated charcoal (50 g).
The patient was admitted to the intensive care unit 80 min after arrival for close monitoring. We administered MB (1 mg/kg), although the MetHb level was low. Six hours after arrival, respiration and circulation were stable, and the lactate level decreased to 5.6 mmol/L. However, the level of lactate then increased to 9.3 mmol/L at 13 h after arrival.
The patient had stable circulation with adequate urine output. He did not show any signs of seizure or infection, which are common causes of an elevated lactate level. Therefore, we believed that metolachlor had induced intracellular metabolic dysfunction just before the TCA cycle. We administered 100 mg of thiamine every 4 h at 16 h after his arrival. The levels of lactate decreased to 1.40 mmol/L at 26 h after arrival. A dramatic improvement of consciousness was noticed after administration of 100 mg thiamine, despite the fact that it only lasted for a short time. We initiated continuous thiamine administration (1500 mg/day) from 28 h to 48 h after arrival. After continuous infusion of thiamine, the level of lactate did not increase, and the patient’s consciousness gradually improved (Figure 1).
On day 3, we terminated mechanical ventilation. On day 4, the patient was transferred to the psychiatric ward, and mirtazapine (15 mg) was started for depression. On day 22, he was admitted voluntarily, and on day 24 he was transferred to the hospital.
Discussion
We present a case of metolachlor-induced lactic acidosis that was successfully treated with thiamine administration. This case yielded some remarkable findings, including metolachlor intoxication without an elevated MetHb level, elevated lactate level, and demonstrated effectiveness of thiamine. For metabolic failure due to metolachlor, methemoglobinemia should be suspected, and methylene blue should be administered first. Subsequently, if lactic acid retention or acidosis progression is observed, thiamine should be considered as a treatment option while ruling out other causes of lactic acidosis.
In the presented case, the patient exhibited bi-phasic elevation of lactate levels. Initially, he showed generalized convulsions along with an elevated level of lactate, although the level of MetHb was not elevated. Seizure can independently elevate the level of muscle lactate owing to anaerobic metabolism caused by systemic convulsions [8]. Our patient did not have any obvious seizure lesion as demonstrated by the head CT, and he did not show signs of seizure after the hospitalization. These findings allowed us to exclude primary brain lesions (which cause seizures), and to consider that the seizure was caused by a secondary metabolic disorder [9]. However, the time of ingestion of the herbicide was unknown, and it is possible that the methemoglobin level had not yet increased; therefore, we decided to administer MB (1 mg/kg).
The second elevation of lactate levels without apparent factors that caused systemic tissue hypoxia in this case was treated with thiamine administration. Notably, the patient’s consciousness was dramatically recovered immediately after the injection of thiamine, thus indicating that the brain function was dependent on thiamine. Taken together, and considering the absence of an increase in MetHb level, the course of seizure occurrence, lactate elevation, and thiamine treatment, it appears that metolachlor possibly induced directly thiamine deficiency and disturbance of intracellular glucose metabolism.
The pathophysiology is attributed to the possible inhibition of pyruvate dehydrogenase by metolachlor. Pyruvate dehydrogenase consists of 3 major complexes and requires 5 coenzymes: thiamine pyrophosphate, lipoic acid, coenzyme A, nicotinamide adenine dinucleotide, and flavin adenine dinucleotide [10]. Chloroacetamide herbicides can alkylate lipoic acid and coenzyme A [11]. Metolachlor can inhibit thiamine pyrophosphate reversibly and/or competitively, although direct inhibition of thiamine pyrophosphate has yet to be elucidated. Additionally, metolachlor can activate thiaminase I activity as an aniline in the human gut by acting as a co-substrate [12], thus leading to thiamine malabsorption and deficiency.
Similar to the presented case, a case of biguanide-induced hyperlactatemia was reported previously, during which the circulatory status improved immediately after thiamine administration [13]. The authors of that study considered the possible pathophysiology related to the direct inhibition of thiamine activity and to the disturbance of the thiamine absorption by biguanides. Moreover, ifosfamide, an alkylating antineoplastic agent, often induces encephalopathy in a manner similar to this case [14]. Although retrospective analyses could not reveal the effectiveness of thiamine on ifosfamide-induced encephalopathy [15], some patients are clearly responsive to thiamine treatments [16,17].
The major limitation of our pathophysiological considerations is that we could not exclude the effects of MetHb as the principal etiology of metolachlor toxicity. In the present case, we did not measure the level of MetHb after hospitalization, which was low on admission. There have been reports of delayed methemoglobinemia caused by metolachlor [5]. Therefore, we could not exclude the possibility of delayed methemoglobinemia, despite the fact that we administered MB.
Metolachlor is extensively used around the world, and it can be accidentally or incidentally absorbed and cause intoxication. Because of its low cost and increased effectiveness, thiamine can be a good treatment option for metolachlor intoxication in patients presenting with neurological symptoms associated with lactate elevation.
Conclusions
We present a case of metolachlor intoxication that led to coma, in which the patient had an elevated lactate level but no elevation of MetHb level. He responded well to thiamine treatment. This case indicates a neurotoxic effect of metolachlor other than MetHb generation, and demonstrates the usefulness of thiamine. Thiamine administration can be a treatment option for encephalopathy related to alkylating agents and/or hyperlactatemia.
References:
1.. [cited 2022 Jul 18]. Available from: https://www.who.int/news-room/fact-sheets/detail/suicide
2.. Sakamoto H, Ishikane M, Ghaznavi C, Ueda P, Assessment of suicide in Japan during the COVID-19 pandemic vs. previous years: JAMA Netw Open, 2021; 4; e2037378
3.. Fuse-Nagase Y, Marutani T, Tachikawa H, Increase in suicide rates among undergraduate students in Japanese national universities during the COVID-19 pandemic: Psychiatry Clin Neurosci, 2021; 75; 351-52
4.. Mew EJ, Padmanathan P, Konradsen F, The global burden of fatal self-poisoning with pesticides 2006–15: Systematic review: J Affect Disord, 2017; 219; 93-104
5.. Macmadu A, Batthala S, Correia Gabel AM, Comparison of characteristics of deaths from drug overdose before vs. during the COVID-19 pandemic in Rhode Island: JAMA Netw Open, 2021; 4; e2125538
6.. Yang CC, Hwang SF, Chou MM, Deng JF, Metobromuron/metolachlor ingestion with late onset methaemoglobinemia in a pregnant woman successfully treated with methylene blue: J Toxicol Clin Toxicol, 1995; 33; 7136
7.. Andersen LW, Mackenhauer J, Roberts JC, Etiology and therapeutic approach to elevated lactate levels: Mayo Clinic Proc, 2013; 88(10); 1127-40
8.. Lipka K, Bülow HH, Lactic acidosis following convulsions: Acta Anaesthesiol Scandinavica, 2003; 47(5); 616-18
9.. Almannai M, al Mahmoud RA, Mekki M, El-Hattab AW, Metabolic seizures: Front Neurol, 2021; 12; 640371
10.. King MW: Integrative Medical Biochemistry Examination and Board Review, 2014, McGraw Hill
11.. Fuerst EP, Understanding the mode of action of the Chloroacetamide and Thiocarbamate herbicides: Weed Technol, 1987; 1(4); 270-77
12.. Kreinbring CA, Remillard SP, Hubbard P, Structure of a eukaryotic thiaminase I: Proc Natl Acad Sci USA, 2014; 111(1); 137-42
13.. Godo S, Yoshida Y, Fujita M, The dramatic recovery of a patient with biguanide-associated severe lactic acidosis following thiamine supplementation: Int Med, 2017; 56(4); 455-59
14.. Ajithkumar T, Parkinson C, Shamshad F, Murray P, Ifosfamide encephalopathy: Clin Oncol, 2007; 19; 108-14
15.. Lentz KL, Clark SM, Ayarza M, Evaluation of thiamine for the prevention of ifosfamide-induced encephalopathy: J Oncol Pharm Pract, 2020; 26(2); 406-12
16.. Imtiaz S, Muzaffar N, Ifosfamide neurotoxicity in a young female with a remarkable response to thiamine: J Pak Med Assoc, 2010; 60(10); 867-69
17.. Hamadani M, Awan F, Role of thiamine in managing ifosfamide-induced encephalopathy: J Oncol Pharm Pract, 2006; 12(4); 237-39
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250