13 January 2023: Articles 
An Unusual Combination of Arthrogryposis, Gastroschisis, Cecal Volvulus, and Malignant Hyperthermia in a Young Woman: A Case Report
Educational Purpose (only if useful for a systematic review or synthesis), Rare coexistence of disease or pathology
Justin Yeh1BEF, Amro Al Ashi1ABEF, Jennifer Hernandez2E*, Christopher Seaver12AEDOI: 10.12659/AJCR.938031
Am J Case Rep 2023; 24:e938031
Abstract
BACKGROUND: The purpose of this study is to discuss a patient with a history of conditions, including arthrogryposis, gastroschisis, and malignant hyperthermia, who presented with cecal volvulus requiring urgent surgical intervention.
CASE REPORT: A 29-year-old woman with a history of arthrogryposis, gastroschisis, malignant hyperthermia, and multiple childhood abdominal surgeries presents to the Emergency Department (ED) with 2 days of abdominal pain and bloody diarrhea. A CT abdomen/pelvis revealed findings concerning for a cecal volvulus. The patient was premedicated and monitored closely by the anesthesia team due to her history of malignant hyperthermia. She underwent an exploratory laparotomy, where a dilated cecum and proximal ascending colon were found to be completely volvulized around the mesentery. Manual bowel detorsion was performed, which resulted in reperfusion of the ischemic-appearing bowel, which then appeared viable. She recovered well after the procedure and was discharged on postoperative day 5.
CONCLUSIONS: This case highlights a patient who presented with a combination of 4 findings: arthrogryposis, gastroschisis, malignant hyperthermia, and cecal volvulus. With arthrogryposis reported to be associated with gastroschisis and malignant hyperthermia, this report not only corroborates this association, but also aims to draw attention to the fact that these conditions have potential to occur jointly with cecal volvulus. Given the patient’s history of gastroschisis requiring extensive abdominal surgeries that contribute as risk factors for cecal volvulus, it is possible there may be other arthrogryposis patients who present with cecal volvulus similar to that seen in this patient.
Keywords: Arthrogryposis, Gastroschisis, general surgery, Intestinal Volvulus, Malignant Hyperthermia, Female, Humans, Child, Adult, Cecal Diseases, Vascular Diseases
Background
Arthrogryposis, also known as arthrogryposis multiplex congenita, is a congenital condition characterized by contracture of 2 or more body parts [1–3]. These congenital contractures consist of hypoplastic muscle intermixed with deposits of fibrous and fatty tissue surrounding an affected joint [4]. The limbs often appear tubular and slender, with a “doughy” consistency upon palpation [4]. The incidence of arthrogryposis in the United States is estimated to be 0.03% [1,2,5,6]. It is a phenotypic symptom, rather than a diagnosis, and is associated with hundreds of syndromes [7]. The primary etiology of arthrogryposis is due to decreased fetal movement in utero [7,8]. Purported secondary etiologies include maternal toxin exposure, infections, genetic, neurological, skeletal, and connective tissue pathologies [2,4,8]. Nearly 220 mutations and genes have been associated with arthrogryposis, with more mutations and genes being identified yearly [2,9].
Gastroschisis is a congenital condition caused by paraumbilical protrusion of the viscera with no membranous cover [10,11]. Herniated viscera, including small and large bowel, liver, spleen, and bladder, are at a risk of stenosis or atresia, leading to further complications, including volvulus, vascular insufficiency, and necrosis [10,12,13]. Gastroschisis is most commonly located to the right of the intact umbilical cord and affects 0.045% of live births [10,12,14]. Hypotheses regarding pathogenesis of gastroschisis include teratogenic exposure, delayed umbilical ring closure during physiologic herniation, and right umbilical vein looping and strangulation of the bowels preventing development and/or return of viscera [15].
Cecal volvulus is the axial malrotation of the colon, including the cecum, ascending colon, and ileum. In the United States, the incidence of cecal volvulus is 2.8–7.1 per million [16,17]. The etiology of cecal volvulus is multifactorial and involves hypermobility of the cecum [18–20]. Risk factors for cecal volvulus include a history of abdominal surgery secondary to postoperative adhesion formation, malrotation, and colonic distention [16].
Malignant hyperthermia (MH) is an autosomal dominant, hypermetabolic, life-threatening condition described as development of an adverse reaction after exposure to certain anesthetic groups, including volatile inhaled anesthetics and nitric oxide [21,22]. In the United States, the incidence of MH is estimated to be 0.02% in the adult population and 0.01% in the pediatric population, with variable ranges existing across the available literature [22,23]. The pathogenesis of MH involves more than 300 identified pathologic variations of the ryano-dine gene (RYR1) located on chromosome 19, all of which lead to excessive calcium release from muscular endoplasmic reticulum during muscle contraction. To restore the released calcium, excessive ATP is utilized, leading to a hypermetabolic state that leads to increased carbon dioxide synthesis, muscular rigidity, tachycardia, hypertension, tachypnea, hyperthermia, and acidosis [21–23].
Case Report
A 29-year-old woman with a past medical history of arthrogryposis, gastroschisis, and malignant hyperthermia presented to the Emergency Department (ED) in May 2021 with 2 days of abdominal pain associated with bloody diarrhea. She had a history of multiple abdominal surgeries, including gastroschisis closure with multiple revisions and colostomy with eventual reversal in 2011.
On presentation, the patient was alert, oriented, tachycardic, and had significant abdominal distention (Figure 1), tenderness to palpation, and hypoactive bowel sounds. A nasogastric tube (NGT) was placed for bowel decompression. The position of the NGT in the left upper quadrant was confirmed with abdominal X-ray, which also showed evidence of a distended cecum in the right lower quadrant (Figure 2). Lab results were unremarkable except for neutrophilia. A CT abdomen/pelvis showed findings suspicious for a cecal volvulus (Figures 3, 4) and the patient underwent an exploratory laparotomy on the same day.
Due to her history of malignant hyperthermia, the patient was premedicated with esmolol prior to the procedure, and inhaled volatile anesthetics and succinylcholine were strictly avoided. Once her abdomen was entered, her peritoneal cavity was noted to contain a clear-appearing sac adherent to the small bowel. This was incised laterally and carefully released from the small bowel, after which dense adhesions were found between small bowel loops in the left abdomen, which were also carefully incised sharply. The falciform ligament was taken down and the abdomen was able to be explored. A dilated cecum and proximal ascending colon were found to be completely volvulized around the mesentery (Figure 5). Manual bowel detorsion was performed to release the volvulus, resulting in transformation of the bowel from ischemic-appearing to viable. No additional bowel ischemia was found, and no bowel resection was indicated. It was noted that the patient’s mesentery was significantly elongated, spanning throughout the entirety of the colon, with associated redundant colon. Based on these findings, the surgical team determined that any attempt to pexy the cecum or the right hemi colon would likely result in a second traction point and increase the risk of another mesenteric volvulus. It was thus decided to return her bowels to the abdominal cavity and proceed with closure. The fascia was approximated with a #1 running looped PDS suture.
The skin was closed with staples and a Prevena wound VAC was placed. The patient tolerated the procedure well without any surgical complications. Total operative time was 1 hour, and estimated blood loss was 5 cc.
The patient was admitted for a total of 5 days and had an uneventful postoperative course. Bowel and bladder habits returned normally, and her diet was advanced stepwise. She was cleared for discharge by Surgery with a scheduled follow-up in 2 weeks. During follow-up, the patient recovered well from a surgical perspective and was cleared for unrestricted activity and regular diet as tolerated.
Discussion
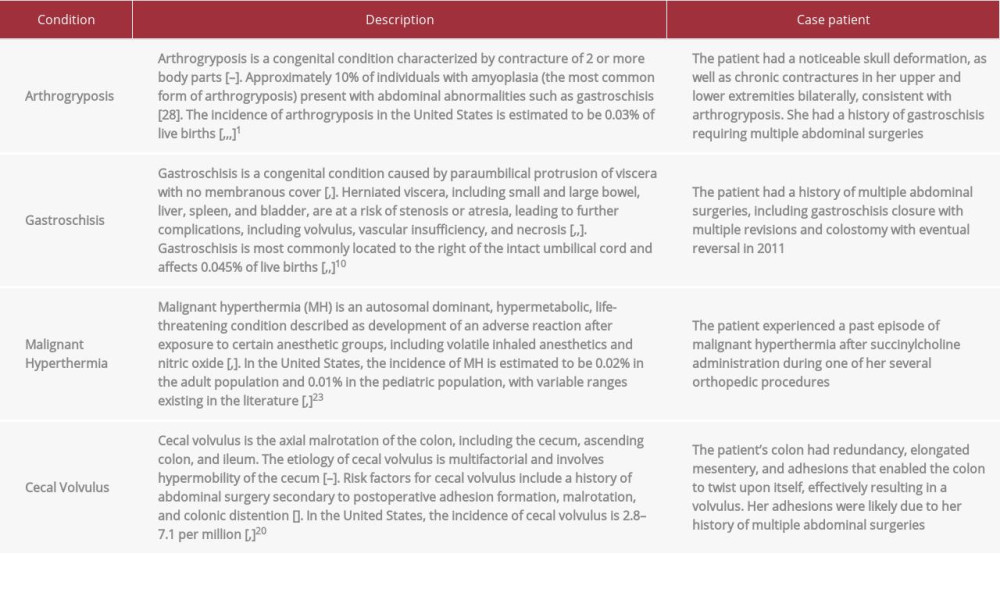
The purpose of this case report is to document an interesting patient who had a history of arthrogryposis, gastroschisis, and malignant hyperthermia who presented with a cecal volvulus. Despite their typically isolated presentations, this patient has been affected by all 4 conditions. Here, we will discuss the associations between the conditions and how each condition relates to the patient presented, which are summarized in Table 1.
Upon literature review, it was found that arthrogryposis is associated with gastroschisis and malignant hyperthermia. Approximately 10% of individuals with amyoplasia (the most common form of arthrogryposis) present with abdominal abnormalities such as gastroschisis [24]. Furthermore, it has been reported that arthrogryposis patients seem to experience more complications during operations; most commonly difficulties with airway management, intravenous access, and intraoperative hyperthermia [3,25]. Despite several documented cases of arthrogryposis patients who have experienced malignant hyperthermia in the peer-reviewed literature, there is insufficient evidence to suggest patients with arthrogryposis are at increased risk of developing malignant hyperthermia compared to control patients without arthrogryposis syndromes (OR, 1.49; 95% CI, 0.78–2.82;
Gastroschisis is a common condition, and it fortunately has an excellent prognosis and survival rate of 91.29%, given proper and timely surgical treatment [14]. Prenatal ultrasound allows for early screening of this condition as early as 12 weeks’ gestation. Other screening exams such as periodic measuring of alpha fetoprotein (AFP) also allow for early detection of abdominal wall defects [26]. Treatment of gastroschisis involves immediate covering of exposed visceral organs with sterile saline dressing covered with plastic wrap to preserve the integrity and moisture as the newborn is transferred to the operating room or neonatal intensive care unit (NICU) for treatment. Depending on the severity of abdominal wall defect, retraction of visceral organs into the abdominal cavities may require a multi-step approach, including temporary silo placement followed by definitive closure. Like other abdominal surgeries, surgical intervention for gastroschisis increases the risk for infection, sepsis, intestinal adhesions, intestinal volvulus, and ileus.
As previously stated, one of the strongest risk factors for cecal volvulus is colonic hypermobility. In this patient’s case, her redundant colon, elongated mesentery, and adhesions enabled the colon to twist upon itself, effectively resulting in a volvulus. If treatment of cecal volvulus is delayed, it carries a mortality rate of more than 30% [19]. The time to treat should be within 24–72 hours after diagnosis [19]. Our patient presented almost 48 hours after the onset of symptoms, but she was promptly taken to the OR once a diagnosis was established. Treatments such as barium enema or colonoscopy may offer a non-operative reduction of a cecal volvulus, but these interventions are rarely successful, and definitive management typically requires surgical intervention [19]. During surgery, patients may undergo an ileocolic resection or a right hemicolectomy [19]. In patients who undergo ileocolic resection, a colopexy is then performed to secure the right remnant colon to the posterior peritoneum, reducing the risk of recurrence [19]. During our patient’s surgery, no resection or colectomies were performed since manual detorsion of the volvulus immediately relieved the bowel ischemia. In the event of dusky or borderline-appearing bowel, indocyanine green (ICG) may be used to assess for bowel perfusion, which assists in the decision of whether to resect the bowel. The surgical team did not pexy the cecum or the right hemi colon to the posterior peritoneum as they postulated this could result in a second traction point that would increase the risk of another mesenteric volvulus. Therefore, the best option was to return the bowels to the abdominal cavity and free up the proximal small bowel from the lateral abdominal wall. This decision was discussed with the patient and her mother postoperatively.
Conclusions
In this case report, we described a young patient with an odd combination of conditions, including arthrogryposis, malignant hyperthermia, and gastroschisis, who presented with cecal volvulus. We also corroborated the association reported between arthrogryposis, gastroschisis, and malignant hyper-thermia. Given the patient’s history of gastroschisis requiring extensive abdominal surgeries that contribute as risk factors for cecal volvulus, it is possible there may be other arthrogryposis patients who present with cecal volvulus similar to that seen in this patient. Therefore, we hope to raise awareness of the potential associations existing between these conditions.
Figures
References:
1.. Bamshad M, Van Heest AE, Pleasure D, Arthrogryposis: A review and update: J Bone Joint Surg Am, 2009; 91(Suppl. 4); 40-46
2.. Bayram Y, Karaca E, Coban Akdemir Z, Molecular etiology of arthrogryposis in multiple families of mostly Turkish origin: J Clin Invest, 2016; 126(2); 762-78
3.. Gleich SJ, Tien M, Schroeder DR, Anesthetic outcomes of children with arthrogryposis syndromes: No evidence of hyperthermia: Anesth Analg, 2017; 124(3); 908-14
4.. Langston S, Chu A, Arthrogryposis multiplex congenita: Pediatr Ann, 2020; 49(7); e299-e304
5.. Binkiewicz-Glinska A, Sobierajska-Rek A, Bakula S, Arthrogryposis in infancy, multidisciplinary approach: Case report: BMC Pediatr, 2013; 13; 184
6.. Ponde V, Desai AP, Shah D, Comparison of success rate of ultrasound-guided sciatic and femoral nerve block and neurostimulation in children with arthrogryposis multiplex congenita: A randomized clinical trial: Paediatr Anaesth, 2013; 23(1); 74-78
7.. Hall JG, Aldinger KA, Tanaka KI, Amyoplasia revisited: Am J Med Genet A, 2014; 164A(3); 700-30
8.. Seidahmed MZ, Al-Kindi A, Alsaif HS, Recessive mutations in SCYL2 cause a novel syndromic form of arthrogryposis in humans: Hum Genet, 2020; 139(4); 513-19
9.. Pehlivan D, Bayram Y, Gunes N, The genomics of arthrogryposis, a complex trait: Candidate genes and further evidence for oligogenic inheritance: Am J Hum Genet, 2019; 105(1); 132-50
10.. Bhat V, Moront M, Bhandari V, Gastroschisis: A state-of-the-art review: Children (Basel), 2020; 7(12); 302
11.. Aktoz F, Ozyuncu O, Tanacan A, Gestational outcomes of pregnancies with prenatally detected gastroschisis and omphalocele: Fetal Pediatr Pathol, 2019; 38(4); 282-89
12.. Abdullah F, Arnold MA, Nabaweesi R, Gastroschisis in the United States 1988–2003: Analysis and risk categorization of 4344 patients: J Perinatol, 2007; 27(1); 50-55
13.. Ledbetter DJ, Gastroschisis and omphalocele: Surg Clin North Am, 2006; 86(2); 249-vii
14.. Ferreira RG, Mendonça CR, Gonçalves Ramos LL, Gastroschisis: A systematic review of diagnosis, prognosis and treatment: J Matern Fetal Neonatal Med, 2022; 35(25); 6199-212
15.. Feldkamp ML, Carey JC, Sadler TW, Development of gastroschisis: Review of hypotheses, a novel hypothesis, and implications for research: Am J Med Genet A, 2007; 143A(7); 639-52
16.. Halabi WJ, Jafari MD, Kang CY, Colonic volvulus in the United States: Trends, outcomes, and predictors of mortality: Ann Surg, 2014; 259(2); 293-301
17.. Hasbahceci M, Basak F, Alimoglu O, Cecal volvulus: Indian J Surg, 2012; 74(6); 476-79
18.. Le CK, Nahirniak P, Qaja E, Cecal Volvulus. [Updated 2021 Sep 14].: StatPearls [Internet], 2021, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK470305/
19.. Perrot L, Fohlen A, Alves A, Lubrano J, Management of the colonic volvulus in 2016: J Visc Surg, 2016; 153(3); 183-92
20.. Lawal TA, Wires ES, Terry NL, Preclinical model systems of ryanodine receptor 1-related myopathies and 113 malignant hyperthermia: A comprehensive scoping review of works published 1990–2019: Orphanet J Rare Dis, 2020; 15(1); 113
21.. Rosenberg H, Davis M, James D, Malignant hyperthermia: Orphanet J Rare Dis, 2007; 2; 21
22.. Kim DC, Malignant hyperthermia: Korean J Anesthesiol, 2012; 63(5); 391-401
23.. Filges I, Hall JG, Failure to identify antenatal multiple congenital contractures and fetal akinesia – proposal of guidelines to improve diagnosis: Prenat Diagn, 2013; 33(1); 61-74
24.. Martin S, Tobias JD, Perioperative care of the child with arthrogryposis: Paediatr Anaesth, 2006; 16(1); 31-37
25.. Harris EL, Minutillo C, Hart S, The long-term physical consequences of gastroschisis: J Pediatr Surg, 2014; 49(10); 1466-70
26.. Van Manen M, Hendson L, Wiley M, Early childhood outcomes of infants born with gastroschisis: J Pediatr Surg, 2013; 48(8); 1682-87
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250