05 April 2023: Articles 
The Importance of Dopamine Deficiency Evaluation in Non-Alzheimer Disease Dementias
Mistake in diagnosis
Bader Alkharisi1ADEF, Khaled Dostzada2ABD, Harleen Kaur2B, Manoj Kumar2B, Jeanne Y. Wei1AF, Gohar Azhar1ADEFDOI: 10.12659/AJCR.938344
Am J Case Rep 2023; 24:e938344
Abstract
BACKGROUND: Dementia with Lewy bodies (DLB) is a common cause of dementia. Given the similarities between the symptoms of DLB and non-DLB Alzheimer disease (AD) and related dementias, patients can sometimes be misdiagnosed with AD. To increase the sensitivity of current DLB guidelines, the DLB Consortium published its fourth revised report in 2017 with increased diagnostic weight given to dopamine transporter (DAT) uptake in the basal ganglia, demonstrated by single-photon emission computed tomography or positron emission tomography imaging. We aimed to describe the role of DAT scans in evaluating dopamine deficiency in patients with overlapping symptoms of AD and DLB.
CASE REPORT: We present case studies of 3 patients with memory impairment who had a diagnosis of probable AD and were being treated with cholinesterase inhibitors. During treatment, dopamine deficiency was suspected and DAT scans were performed. All 3 patients revealed severe DAT deficits in the bilateral corpus striatum. These results were consistent with probable DLB as per the current revised DLB Consortium report. All patients received treatment with carbidopa/levodopa and demonstrated improved overall function.
CONCLUSIONS: All 3 of our cases demonstrated the role of DAT scans in evaluating dopamine deficiency syndromes in patients with overlapping symptoms of neurocognitive disorders. Thus, a DAT scan is critical for establishing an earlier and more definitive diagnosis of DLB, which provides treatment options for dopamine replacement. It also assists providers with prognostication of dopamine deficiency syndromes and is therefore beneficial in counseling patients and caregivers.
Keywords: Alzheimer Disease, Diagnostic Errors, Dopamine Plasma Membrane Transport Proteins, Lewy Body Disease, Parkinson Disease, Humans, Dopamine, Tomography, Emission-Computed, Single-Photon, Positron-Emission Tomography
Background
Lewy body dementia is an umbrella term that encompasses the clinical conditions of dementia with Lewy bodies (DLB) and Parkinson disease with dementia (PDD). These conditions are characterized by the accumulation of aggregated α-synuclein into Lewy bodies and Lewy neurites in neurons and neuronal processes [1–3]. The diagnosis and management of DLB is often a challenge because cognitive impairment and hallucinations can also occur in Alzheimer disease (AD) and PDD. Often there is significant amyloid or tau deposition with co-pathology of AD in patients with DLB and PDD and hence acetylcholinesterase inhibitors may be beneficial [1–3]. However, unlike AD, patients with DLB and PDD suffer from severe neuroleptic sensitivity [1,2], and this sensitivity to antipsychotics can complicate the management of hallucinations. In differentially diagnosing these conditions, it is also important to establish a dopamine deficient state so that therapy with either dopa-mine precursors, dopamine agonists, or anticonvulsants might be used to ameliorate the symptomatology of Parkinson disease. The distinction between DLB and PDD has been made easier by the current guidelines suggesting that DLB should be diagnosed when dementia occurs before, or concurrently with, parkinsonism; whereas PDD should be diagnosed in the context of well-established Parkinson disease [3].
The DLB Consortium report further emphasized the need to carefully review clinical features and biomarkers to increase the criteria sensitivity in diagnosing DLB and distinguishing it from other neurocognitive disorders [4]. These include rapid eye movement (REM) sleep behavior disorder, 123iodine-metaiodobenzylguanidine myocardial scintigraphy, and dopamine transporter (DAT) uptake in the basal ganglia demonstrated by single-photon emission computed tomography (SPECT) or positron emission tomography (PET) imaging. Dopamine transporter single-photon emission computerized tomography (DATSPECT) is a valuable tool in evaluating and managing patients with possible DLB. Based on studies, it carries a mean sensitivity of 77.7% for detecting probable DLB, with a specificity of 90.4% for excluding non-DLB dementia, which is predominantly due to AD. A mean value of 85.7% was achieved for overall diagnostic accuracy [5]. In the following 3 cases, we present the role of DAT scans in evaluating dopamine deficiency in patients with overlapping symptoms of AD and DLB.
Case Reports
CASE 1:
An 80-year-old woman came to the clinic accompanied by her husband for evaluation of memory loss that had been ongoing for the past 9 months. She also reported having hallucinations of seeing people and animals. She was highly anxious and needed help with medication management, although she could cook and drive. Her mother had AD.
Physical examination was normal, with no rigidity, hypertonia, or bradykinesia. Her Montreal Cognitive Assessment (MoCA) was 14/30. Neuropsychological testing revealed that the most pronounced declines were in complex attentional tasks. Clinical chemistry showed no significant abnormalities. Magnetic resonance imaging (MRI) showed mild-to-moderate loss in brain volume, and minimal periventricular and subcortical small vessel ischemic changes.
She was started on donepezil (5 mg/day). However, her memory impairment, functional abilities, and hallucinations worsened. She developed anxiety, and, when agitated, she exhibited trembling of her hands and legs, along with difficulty walking. A diagnosis of DLB was suspected and a DAT scan was done. The results were consistent with severe DAT deficit in the bilateral corpus striatum (Figure 1A, Table 1A). Given her progressive hallucinations, she was started on a low dose of an antipsychotic (quetiapine), prior to beginning therapy with levodopa. Subsequently, there was some improvement in her gait and tremors with carbidopa-levodopa therapy.
CASE 2:
An 83-year-old woman presented with generalized weakness that she had been experiencing for 2 years. Her presenting list of complaints included memory difficulties, fatigue, weak voice, difficulty with getting up from a chair, and numbness in her hands. The patient’s husband reported that she was very weak and required assistance with dressing and grooming. She had been diagnosed with AD in the past and was on memantine.
Physical examination was significant for a slender frame with sarcopenia, decreased facial expressions, and slow speech. There were no noticeable tremors, rigidity, or bradykinesia. She was in a wheelchair and was unable to get up, stand, or walk without assistance. She was tearful and upset with her weakness. Her MoCA was 21/30. Blood chemistry was unre-markable and a brain MRI revealed mild deep white matter changes and mild volume loss.
She was started on donepezil (5 mg/day). Her course was significant for worsening depression with crying spells. She was dependent on the help of others for activities of daily living. Parkinson disease was suspected and a DAT scan was performed which revealed severe dopamine transporter deficiency in the bilateral putamen and caudate nuclei, with the right posterior putamen being mildly more affected (Figure 1B, Table 1B). She was started on carbidopa-levodopa with improvements in her mobility, stiffness, and energy level. At subsequent visits, she got up from the chair unassisted and walked independently. Her stiffness and tremors were significantly reduced and her mood was much better. Her memory impairment remained stable and did not worsen.
CASE 3:
An 85-year-old man came to the clinic, accompanied by his son, complaining of memory problems that had been worsening for the past 5 years. The patient reported feeling useless since he had retired. His son indicated that the patient had become argumentative, depressed, and anxious. In addition, the patient complained of dizziness. He had restless legs and occasional dream enactment. He was independent in activities of daily living, but required assistance with shopping, transportation, and housekeeping. He was taking memantine, rivastigmine (patch), sertraline, and duloxetine.
Physical examination was normal aside from memory deficits. His MoCA was 19/30. Blood chemistry showed moderate microcytic anemia, mild hypothyroidism, and low vitamin B12 and vitamin D. Brain MRI demonstrated diffuse mild volume loss and chronic microvascular ischemic changes.
On a subsequent followup visit, he admitted to having a history of hallucinations, which included seeing people walking in the house. He also reported a history of frequent, unexplained falls. Given his hallucinations, dementia, and falls, a decision was made to perform a DAT scan which showed a severe dopamine transporter deficiency in the bilateral corpus striatum (Figure 1C, Table 1C). He was started on carbidopalevodopa and was referred to neurology. His carbidopa-levodopa was titrated up with an improvement in his Parkinson disease symptomatology.
Discussion
DLB accounts for 10–20% of all cases of dementia. It is often regarded as the second or third most common cause of dementia after AD [6]. On brain MRIs, the medial temporal lobe is often reduced in size in AD compared with DLB with normal aging, but there is no dopamine deficiency in patients with AD and normal aging [4]. The diagnostic dilemma is in overlapping symptomatology of cognitive impairment, hallucinations, and movement disorder in DLB and PDD, making it particularly challenging for providers to accurately distinguish between these dementia subtypes.
The need to accurately diagnose DLB is important given its different outcomes and management. A major tool for increasing diagnostic accuracy is through a DAT scan. One study suggested its sensitivity reaches 77.7% for detecting clinically probable DLB, with a specificity of 90.4% for excluding non-DLB dementia [5]. Another study suggested a sensitivity of 78% and specificity of 94% [7]. Another study showed sensitivity of 63% and a specificity of 100% [8].
In all 3 of our cases, the initial symptomatology was unclear for dopamine deficiency and patients were treated for AD with only cholinesterase inhibitors. Worsening of their memory, reduced functional ability, and new symptomatology were also attributed to dementia of the Alzheimer type by the primary care provider. DAT scans were ordered in a memory clinic by a geriatrician within a few months of the initial visit, and assisted in differentially diagnosing DLB from AD and instituting appropriate management.
Conclusions
All 3 of our cases demonstrated the role of DAT scans in evaluating dopamine deficiency syndromes in patients with symptoms overlapping those of AD. A DAT scan provides supporting evidence for a diagnosis of dopamine deficiency syndromes so that providers might feel more confident in trying specific treatment options related to dopamine replacement. It also helps in better monitoring and prognostication of diseases associated with dopamine deficiency and can thus assist providers in counseling patients and caregivers. Although not all dopamine deficiency states respond well to treatment, earlier diagnosis and treatment can significantly improve the quality of life of these patients. It is unfortunate that there is a dearth of experts in dementia, and severe dopamine deficiency often goes unrecognized. Therefore, it is imperative that primary care physicians become aware of dopamine deficiency states that mimic or co-exist with AD, and the usefulness of obtaining a DAT scan to assist them with the diagnosis and appropriate management of these conditions.
References:
1.. Chandler J, Georgieva M, Desai U, Disease progression and longitudinal clinical outcomes of Lewy body dementia in the NACC database: Neurol Ther, 2023; 12(1); 177-95
2.. Hershey LA, Coleman-Jackson R, Pharmacological Management of dementia with Lewy bodies: Drugs Aging, 2019; 36(4); 309-19
3.. Meng YH, Wang PP, Song YX, Wang JH, Cholinesterase inhibitors and memantine for Parkinson’s disease dementia and Lewy body dementia: A meta-analysis: Exp Ther Med, 2019; 17(3); 1611-24
4.. McKeith IG, Boeve BF, Dickson DW, Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium: Neurology, 2017; 89(1); 88-100
5.. McKeith I, O’Brien J, Walker Z, Sensitivity and specificity of dopamine transporter imaging with 123I-FP-CIT SPECT in dementia with Lewy bodies: A phase III, multicentre study: Lancet Neurol, 2007; 6(4); 305-13
6.. McKeith IG, Burn DJ, Ballard CG, Dementia with Lewy bodies: Semin Clin Neuropsychiatry, 2003; 8(1); 46-57
7.. O’Brien JT, Colloby S, Fenwick J, Dopamine transporter loss visualized with FP-CIT SPECT in the differential diagnosis of dementia with Lewy bodies: Arch Neurol, 2004; 61(6); 919-25
8.. O’Brien JT, McKeith IG, Walker Z, Diagnostic accuracy of 123I-FPCIT SPECT in possible dementia with Lewy bodies: Br J Psychiatry, 2009; 194(1); 34-39
Tables
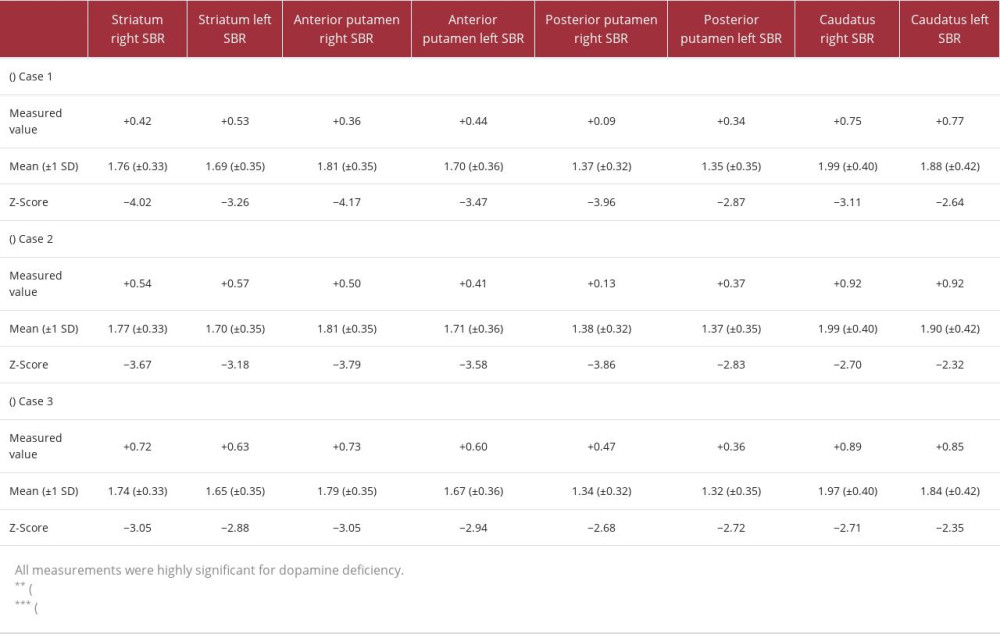 Table 1.. DAT scan-measured values compared with age-specific mean values, followed by the Z-Score for (A) Case 1, (B) Case 2, and (C) Case 3, respectively.
Table 1.. DAT scan-measured values compared with age-specific mean values, followed by the Z-Score for (A) Case 1, (B) Case 2, and (C) Case 3, respectively.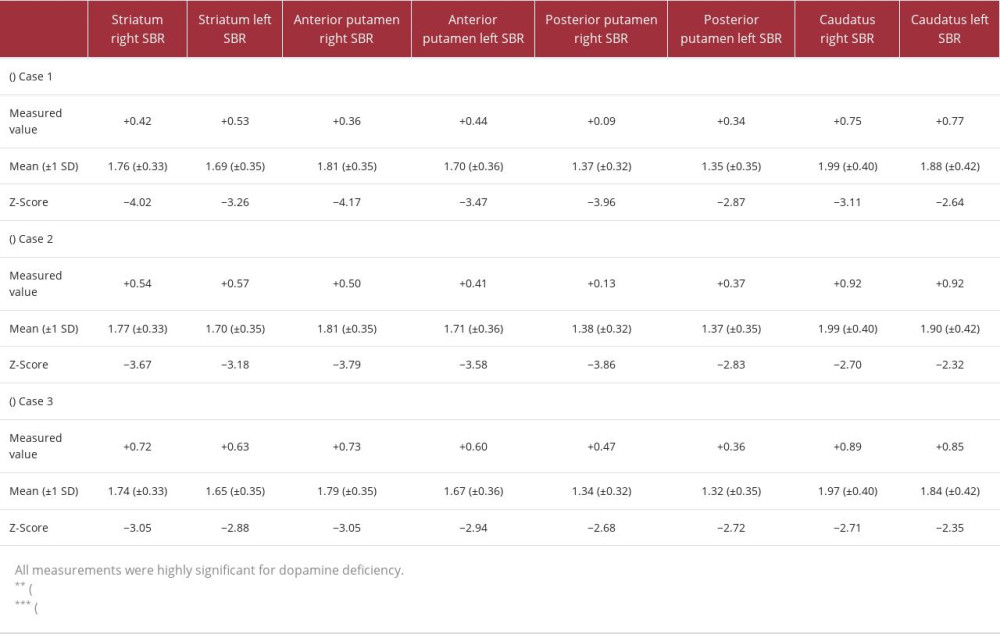 Table 1.. DAT scan-measured values compared with age-specific mean values, followed by the Z-Score for (A) Case 1, (B) Case 2, and (C) Case 3, respectively.
Table 1.. DAT scan-measured values compared with age-specific mean values, followed by the Z-Score for (A) Case 1, (B) Case 2, and (C) Case 3, respectively. In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








