01 December 2022: Articles 
Coma, Severe Hypotension, and Pinpoint Pupils After Olanzapine Intoxication in the Intensive Care Unit with Symptom Reversal After Administration of Flumazenil
Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents, Adverse events of drug therapy
Paul PålssonDOI: 10.12659/AJCR.938387
Am J Case Rep 2022; 23:e938387
Abstract
BACKGROUND: Olanzapine is an antipsychotic drug and is used in critical care to treat delirium. There is no known antidote to olanzapine intoxication. Overdosing olanzapine can cause, tremor, bradykinesia, hypotension somnolence, coma, and miosis.
CASE REPORT: We present the case of a previously healthy 69-year-old man who after routine mitral valve surgery developed pneumonia and severe sepsis requiring several weeks on a ventilator in the Intensive Care Unit. He developed delirium and paranoia and was prescribed olanzapine. After 4 doses, he became hypotensive and nonresponsive and developed pinpoint pupils. The symptoms were reversed minutes after administration of flumazenil. The clinical picture in this case corresponds well with an olanzapine intoxication. No other drugs, such as benzodiazepines or opioids, had been administered that could explain the reaction. Olanzapine intoxication is known to present with hypotension, coma, and miosis. The doses given were normal starting doses for olanzapine in the outpatient setting but much higher than recommended doses in the intensive care setting.
CONCLUSIONS: This case illustrates a risk for severe adverse effects, even within normal prescription range, when olanzapine is used in the intensive care setting. Finally, it is intriguing that the symptoms were reversed after administration of flumazenil, a selective competitive antagonist of the GABA receptor. Olanzapine mainly effects dopamine, serotonin, a1-adrenergic, histamine, and muscarinic receptors, but a low affinity to GABA and benzodiazepine sites can perhaps explain the observed effect.
Keywords: Drug Overdose, Flumazenil, olanzapine, Male, Humans, Aged, Coma, Intensive Care Units, Benzodiazepines, Miosis, Hypotension, Delirium
Background
Olanzapine is an antipsychotic drug used to treat schizophrenia and bipolar disorder. In the critical care setting, olanzapine is used to treat delirium. The mechanism of action for olanzapine is not fully known but it binds to a wide range of sites such as dopamine, serotonin, α1-adrenergic, histamine, and muscarinic receptors [1]. Taken as a rapidly disintegrating tablet, more than 80% of peak plasma concentration of olanzapine is reached within 2 h, and peak concentration is observed after 4 h [2]. Olanzapine is mainly metabolized in the liver and the mean half-life is 33 h, with even longer half-life in elderly patients [3]. Olanzapine is metabolized primarily by CYP1A2 and to a lesser extent by CYP2D6 [4]. When olanzapine is used in critical care, tremor, bradykinesia, and daytime somnolence have been described as adverse effects. There is no known antidote [5]. Here we present a case of a patient in the Intensive Care Unit (ICU) reacting with coma, hypotension, and pinpoint pupils after administration of olanzapine.
Case Report
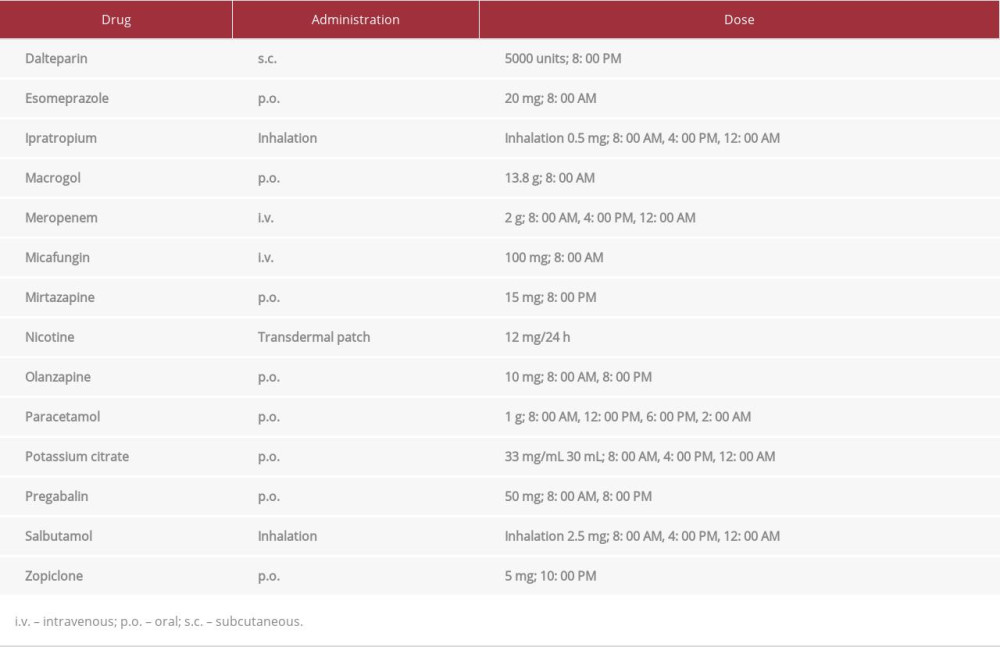
A previously healthy 69-year-old male patient acquired pneumonia after routine mitral valve surgery. He developed severe sepsis and was admitted to the ICU, where he was treated with high doses of vasopressors and required continuous hemodialysis, as well as invasive ventilator support. Initial postoperative pain was managed with a remifentanil infusion; no long-acting opioids were administered. After 2 weeks on ventilator support, he was weaned and decannulated. In the recovery phase, he developed a hyperactive delirium, with confusion, paranoia, hallucinations, and agitation. It was diagnosed as an ICU delirium, and it was decided that there was no need for magnetic resonance imaging. Non-pharmacological treatment, such as early mobility and sleep-wake cycle preservation, was tried according to local protocols, but the delirium persisted. To treat the delirium, he was prescribed 10 mg olanzapine orally. The reason for the choice of olanzapine to treat the delirium and why a starting dose of 10 mg was prescribed instead of the lower doses suggested in literature [9,10] was not documented. The first prescription was 10 mg once daily, but as the delirium worsened during the day, the doctor on call for the night changed the dosage to twice daily. For a complete medication schedule, see Table 1. During morning rounds, at 8: 00 AM, just after he was given the fourth dose of olanzapine, he was awake and could recite his social security number. Half an hour later, at 8: 30 AM, he started to become hypotensive, with a blood pressure of 70/40 mmHg and heart rate of 90 beats per min. By 10: 00 AM, he was nonresponsive, with a Glasgow coma scale score of 7 (eyes: 1, verbal: 1, motor response: 5). In addition, he had pinpoint pupils. He still maintained his airway and had a respiratory rate slightly elevated, at 22 breaths per min. An arterial blood gas showed normal pO2 (10.0 kPa) and low pCO2 (4.6 kPa). His blood sugar level was slightly elevated (7.6 mmol/L). A norepinephrine infusion was started to treat his hypotension, but the Glasgow coma scale score remained at 7 despite normal blood pressure. After ruling out other causes of the symptoms, such as hypoxia, hypercapnia, low blood sugar, and severe hypotension, our clinical suspicion was intoxication. He was given 0.4 mg naloxone i.v. but without effect as an attempt to treat a suspected opioid intoxication. After 15 min, he was given 0.5 mg of flumazenil i.v., as, at the time, we thought that he might have received benzodiazepines. Within a minute, he opened his eyes spontaneously and could answer questions. At the same time, we could observe that his pupils dilated back to normal. When investigating his chart, we noted that he had not been given any opioids for the last 48 h. The only sedative given was 7.5 mg zolpidem 12 h before this incident.
Discussion
Olanzapine intoxication predominantly presents with anticholinergic symptoms, miosis, and central nervous system depression [6]. We found that the clinical picture in the present case corresponded well with an olanzapine intoxication. The patient had not been given any other sedatives or opioids that could cause the sedation. The symptoms of coma, hypotension, and miosis are all described in olanzapine overdoses [6,7]. He developed symptoms half an hour after he was given olanzapine, which corresponds well with the pharmacokinetics [2,3]. Other causes of coma, such as hypoxia, hypercapnia, low blood sugar, and severe hypotension were ruled out.
It is intriguing that the patient presented with a severe reaction to a dose within the standard prescription range of olanzapine, 10 mg twice daily [8]. A retrospective study with 26 cases of olanzapine intoxication described one patient who had taken 30 mg. In most cases, doses causing intoxication were much higher, ranging up to 840 mg [6]. However, starting doses for olanzapine in the ICU suggested in literature are much lower, range from 1.25 mg to 2.5 mg daily [9,10]. Our patient was therefore given significantly higher doses than what is suggested for treatment in the ICU. With a half-life potentially as long as 50 h [3], it is plausible that the patient had accumulated olanzapine and eventually reached a plasma concentration high enough to give severe adverse effects. Since olanzapine is mainly metabolized in the liver by CYP1A2, any drug inhibiting CYP1A2 could potentially slow down the metabolism of olanzapine and elevate plasma concentrations. As far as we know, none of the other drugs administered to the patient are primarily metabolized by CYP1A2 and no CYP1A2 inhibitor was used. There are also genetic polymorphisms on CYP1A2 activity in humans, and some haplotypes have lower activity, decreasing olanzapine metabolism [4,11].
Another factor to consider is central anticholinergic syndrome, a syndrome not unusual in the intensive care setting, presenting with somnolence, confusion, agitation, hallucinations, delirium, and sometimes coma. The syndrome can present itself when multiple drugs with anticholinergic action are used simultaneously [12]. Our patient was treated with ipratropium inhalations, which have an anticholinergic effect. Since olanzapine also has an antagonistic action on cholinergic receptors, this might have worsened a preexisting central anticholinergic syndrome.
Finally, we were puzzled by the reversal of symptoms after the administration of flumazenil. There is no accepted antidote to olanzapine intoxication. However, there are a few case reports suggesting potential candidates. One describes successful use of intravenous lipid infusion [13]. Another presents 2 patients treated with physostigmine [14]. Flumazenil is used as an antidote to benzodiazepines and binds to GABA receptors [15]. To the best of our knowledge, it has not been tried as an antidote to olanzapine. Although it binds to many sites, the main effect of olanzapine is on dopamine, serotonin, α1-adrenergic, histamine, and muscarinic receptors. A low affinity to GABA and benzodiazepine sites is described [1]. It is plausible that high doses of olanzapine can have an effect on GABA receptors. Stimulation of GABA receptors, as seen in benzodiaze-pine intoxication, can cause unconsciousness. It is plausible that the effect on consciousness from toxic doses of olanzapine is mediated through GABA receptors as well. In that case, our observation with the patient waking up after receiving flumazenil was a consequence of flumazenil competing with olanzapine at the GABA-receptor site, which is similar to its mechanism of action in benzodiazepine intoxications. However, unpredictable fluctuations between somnolence and agitation are common in olanzapine intoxications [6]. Such spontaneous reversal of symptoms can be an alternative explanation of our case. Another explanation, however unlikely, would be an error in administration of the fourth dose of olanzapine. Confusion between olanzapine and a potent benzodiazepine or opiate could perhaps mimic an olanzapine intoxication and explain the rapid response to antidote. Experimental and clinical studies are needed to further investigate whether flumazenil has potential as an antidote to olanzapine intoxications.
Conclusions
It is important to consider a risk for severe adverse effects, even within the normal prescription range, when olanzapine is used in the intensive care setting. In our case, symptoms were reversed after the administration of flumazenil. Further research is needed to investigate its potential use as an antidote to olanzapine intoxication.
References:
1.. Bymaster FP, Calligaro DO, Falcone JF, Radioreceptor binding profile of the atypical antipsychotic olanzapine: Neuropsychopharmacology, 1996; 14; 87-96
2.. Markowitz JS, DeVane CL, Malcolm RJ, Pharmacokinetics of olanzapine after single-dose oral administration of standard tablet versus normal and sublingual administration of an orally disintegrating tablet in normal volunteers: J Clin Pharmacol, 2006; 46; 164-71
3.. Callaghan JT, Bergstrom RF, Ptak LR, Beasley CM, Olanzapine pharmacokinetic and pharmacodynamic profile: Clin Pharmacokinet, 1999; 37; 177-92
4.. Desta Z, Flockhart DA, Chapter 18 – Pharmacogenetics of drug metabolism: Clinical and translational science, 2017; 327-45, Cambridge, MA, Academic Press
5.. Kim S-W, Yoo J-A, Lee S-Y, Risperidone versus olanzapine for the treatment of delirium: Hum Psychopharmacol, 2010; 25; 298-302
6.. Palenzona S, Meier PJ, Kupferschmidt H, Rauber-Luethy C, The clinical picture of olanzapine poisoning with special reference to fluctuating mental status: J Toxicol Clin Toxicol, 2004; 42; 27-32
7.. Petersen AB, Andersen SE, Christensen M, Larsen HL, Adverse effects associated with high-dose olanzapine therapy in patients admitted to inpatient psychiatric care: Clin Toxicol, 2014; 52; 39-43
8.. , Food and Drug Administration Web site [Accessed September 4, 2022]https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/020592s062021086s040021253s048lbl.pdf
9.. Rivière J, van der Mast RC, Vandenberghe J, Van Den Eede F, Efficacy and tolerability of atypical antipsychotics in the treatment of delirium: A systematic review of the literature: Psychosomatics, 2019; 60; 18-26
10.. Wang M, Yankama TT, Abdallah GT, A retrospective comparison of the effectiveness and safety of intravenous olanzapine versus intravenous haloperidol for agitation in adult Intensive Care Unit patients: J Intensive Care Med, 2022; 37(2); 222-30
11.. Thorn CF, Aklillu E, Klein TE, Altman RB, PharmGKB summary: Very important pharmacogene information for CYP1A2: Pharmacogenet Genomics, 2012; 22; 73-77
12.. Schneck HJ, Rupreht J, Central anticholinergic syndrome (CAS) in anesthesia and intensive care: Acta Anaesthesiol Belg, 1989; 40; 219-28
13.. Yurtlu BS, Hanci V, Gür A, Turan IO, Intravenous lipid infusion restores consciousness associated with olanzapine overdose: Anesth Analg, 2012; 114; 914-15
14.. Weizberg M, Su M, Mazzola JL, Altered mental status from olanzapine overdose treated with physostigmine: Clin Toxicol, 2006; 44; 319-25
15.. An H, Godwin J, Flumazenil in benzodiazepine overdose: CMAJ, 2016; 188; E537
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250