31 January 2023: Articles 
A 36-Year-Old Woman with Acute Liver Failure Following Acetaminophen Overdose, Raised INR of 8.7, and Normal Blood Viscosity Measured by Rotational Thromboelastometry (ROTEM)
Unusual clinical course, Challenging differential diagnosis, Diagnostic / therapeutic accidents, Unusual setting of medical care
Uzung Yoon1ABCDEF*, Manny Lai1E, Tho Nguyen1EF, Elia Elia1EDOI: 10.12659/AJCR.938500
Am J Case Rep 2023; 24:e938500
Abstract
BACKGROUND: Fulminant hepatic failure (FHF) is commonly associated with elevated prothrombin time (PT) and international normalized ratio (INR). There is a commensurate decline in pro- and anti-hemostatic factors, and hemostatic function is rebalanced, not reflected in INR. This report presents the case of a 36-year-old woman with FHF following acetaminophen overdose, an increased INR above 8.7, and normal blood viscosity measured by rotational thromboelastometry (ROTEM).
CASE REPORT: A 36-year-old woman presented with FHF following an acetaminophen overdose. On arrival, she was lethargic but arousable and followed commands. Her King’s College Criteria for acetaminophen toxicity was 2 and her MELD score was 36. Her INR was unmeasurably high (>8.7). To evaluate whole-blood coagulation, a ROTEM analysis was performed. All parameters (CT, CFT, alpha-angle, A10, MCF) of the NATEM were within reference range. Despite the normal ROTEM, spontaneous bleeding was a concern. The patient received 5 units of cryoprecipitate and 9 units of FFP prior to a central venous line placement. She was started on molecular adsorbent recirculating system and continuous veno-venous hemodialysis, but died on day 7.
CONCLUSIONS: Patients with FHF can have normal whole-blood coagulation based on ROTEM even if INR levels are unmeasurably high. Viscoelastic tests such as ROTEM, which assesses whole-blood coagulation properties, are preferrable for coagulation monitoring in these patients. Blood product transfusion to correct coagulation abnormality, like FFP and cryoprecipitate, may be used based on the result of viscoelastic testing over conventional coagulation testing.
Keywords: Blood Coagulation, Liver Transplantation, Female, Humans, Adult, Thrombelastography, International Normalized Ratio, Acetaminophen, Blood Viscosity, Blood Coagulation Disorders, Liver Failure, Acute
Background
Acetaminophen hepatotoxicity accounts for more than 50% of overdose-related acute liver failure cases and approximately 20% of liver transplant cases [1]. Metabolism primarily occurs through glucuronidation and sulfuration in the liver. In an overdose, these pathways are saturated, thereby forming the noxious NAPQI metabolite. NAPQI is a toxic substance that causes irreversible hepatic necrosis [2,3]. Current management of acetaminophen overdose involves administering intravenous or oral acetylcysteine. Previous systematic reviews have indicated that treatment with acetylcysteine can decrease morbidity and mortality [4].
Fulminant hepatic failure (FHF) can occur from acetaminophen hepatotoxicity and is commonly associated with elevated prothrombin time (PT) and international normalized ratio (INR). There is a commensurate decline in pro- and anti-hemostatic factors, and hemostatic function is rebalanced. This is not reflected in INR [5], which is derived from PT. It is calculated as a ratio of the patient’s PT to a control PT standardized for the potency of the thromboplastin reagent. This was developed by the World Health Organization (WHO) using the following formula: INR=Patient PT÷Control PT [6]. The reference values for INR consider PT measurement in device-related variations, type of reagents used, and sensitivity differences in the tissue factor (TF) activator. At our institution, the reference value for INR is 0.82–1.13.
PT/INR can be prolonged in liver dysfunction, vitamin K deficiency, malnutrition, disseminated intravascular coagulation, factor deficiency, drug interactions, anemia, sepsis, advanced-stage cancer, end-stage renal disease, or laboratory errors. The viscoelastic test of whole-blood hemostasis was first developed by Hartert in 1948 [7]. TEG was introduced by Kang et al in 1985 in liver transplantation [8]. The ROTEM® (Instrumentation Laboratory, Bedford, MA, USA) system is a development of the classic TEG and has been used widely in liver transplantation, cardiovascular surgery and trauma, and other clinical settings for coagulation management [9–11]. The system records the kinetic changes during the interaction of platelets with the coagulation factors from initial platelet–fibrin interaction through platelet aggregation, clot strengthening, and fibrin cross-linking to eventual clot lysis [12].
At our institution, the conventional coagulation testing laboratory and the ROTEM® laboratory are in full compliance with the College of American Pathologists (CAP) and the Clinical Laboratory Improvement Amendments (CLIA) regulations and certified by CLIA and the Department of Health.
To address the risk of bleeding in FHF patients with an elevated INR, fresh frozen plasma (FFP) is commonly transfused prior to an invasive procedure. However, PT/INR is a poor indicator of hemostatic function in acute liver disease, and recent evidence has shown that ROTEM is a better tool for whole-blood coagulation monitoring [13,14]. This report presents the case of a 36-year-old woman with FHF following acetaminophen overdose, an increased INR of 8.7, and normal blood viscosity measured by ROTEM.
Case Report
A 36-year-old woman was admitted for FHF due to acetaminophen overdose. On arrival, she was lethargic but arousable and followed commands. Her vital signs were stable. There was no evidence of focal neurological deficits, and both cardiopulmonary examinations were unremarkable. The patient’s medical history included depression, remote history of polysubstance abuse, and suicide attempts. Her home medications were cetirizine-pseudoephedrine, famotidine, fluticasone, and paroxetine. The patient had ingested up to 80 pills of acetaminophen in the past few days and had a serum acetaminophen (APAP) level of 110 mcg/mL (<25 mcg/mL) with AST: 1900 IU/L (7–35 IU/L), ALT 1900 IU/L (<30 IU/L). Her Model for End-Stage Liver Disease (MELD) score was 36 [Na+: 141 mmol/L (135–146 mmol/L), creatinine: 0.9 mg/dL (0.7–1.4 mg/dL), INR >8.71 (0.82–1.13), bilirubin: 3.6 mg/dL (0.1–0.9 mg/dL)]. Her King’s College Criteria for Acetaminophen Toxicity was 2 [INR> 6.5, grade IV hepatic encephalopathy]. Her other labs were hemoglobin 11 g/dL (12.5–15 g/dL); hematocrit 33% (36–46%); platelets 156 000 (140–400 B/L); fibrinogen 116 mg/dL (204–462 mg/dL); PT >100 s (8.9–13.1 s); partial thromboplastin time (PTT) 30 s; factor V activity 7% (normal 50–150%); D-dimer: 10658 ng/ml (<204 ng/ml). To rule out laboratory errors, INR was repeated within 4 h of the initial result, showing INR >8.7 and PT >100 s. Her clinical history, physical exam, and other lab results did not reveal any other cause for the high INR.
Upon admission, a liver transplantation anesthesiologist was consulted to evaluate the patient for possible liver transplantation. A viscoelastic test was performed with ROTEM®-Delta due to the elevated PT/INR and concern for spontaneous bleeding. The NATEM test was used. Clotting Time (CT), Clot Formation Time (CFT), alpha-angle, Clot Amplitude at 10 min (A10) and 20 min (A20), and Maximum Clot Firmness (MCF) were all within reference range (Figure 1).
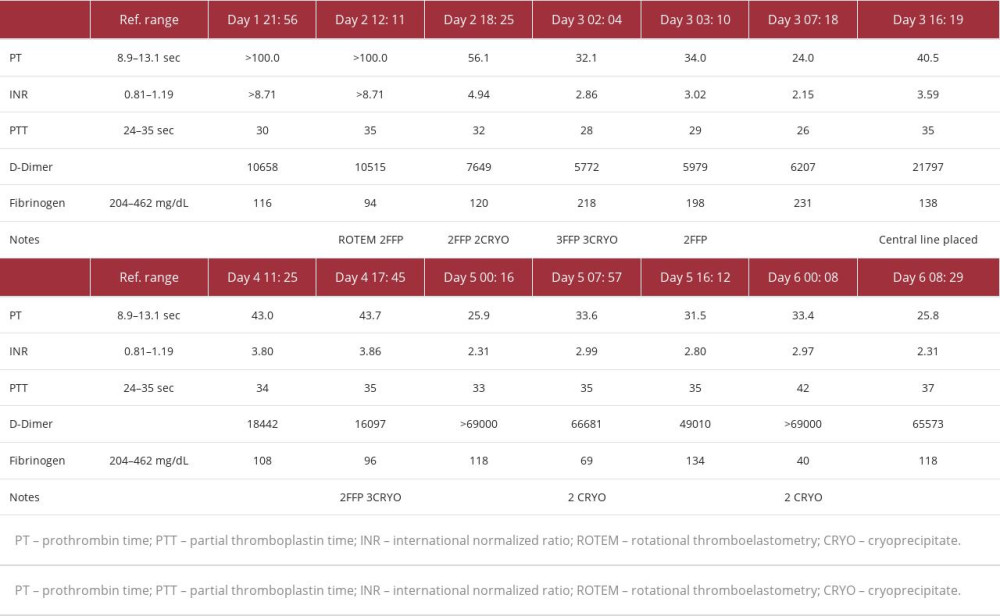
The patient became hypoglycemic and tachypneic with shallow breathing and had developed significant encephalopathy. She became lethargic, minimally responsive, and was intubated within 24 h of admission. On admission day 2, despite the normal ROTEM analysis, the hepatologist was concerned about the patient’s severe coagulopathy, and 9 units of FFP and 5 units of cryoprecipitate were given before a central line placement for molecular adsorbent recirculating system (MARS). No bleeding-related complications or post-procedure hematoma occurred after femoral vein central line insertion. No transfusion reaction was noted. MARS continued for 5 days. During this time, the patient developed acute kidney injury and showed signs of fluid overload and pulmonary edema on a chest X-ray, which was treated with continuous veno-venous hemodialysis (CVVHD). Unfortunately, the patient was not deemed a suitable candidate for liver transplantation due to her history of multiple drug overdosing attempts without obtaining treatment and minimal social support available after transplantation. Despite full medical care, her clinical status deteriorated with worsening neurological exam, abdominal distension, rapid rise in lactate, progressive sinus tachycardia, and acidemia consistent with sepsis. She was started on empiric antibiotics and norepinephrine infusion, without improvement. Her poor prognosis was communicated to the family, and the patient died on hospital admission day 7. During the hospital stay, despite the elevated PT/ INR, no signs of clinical bleeding were observed. The INR trend is shown in Figure 2 and Table 1.
Discussion
The primary finding in this case is that, despite an unmeasur-ably high INR (>8.7), the patient’s whole-blood coagulation was still normal based on ROTEM analysis. The literature reports patients with acetaminophen toxicity and hepatic failure resulting in elevated INR [15,16]. However, the focus in those case reports was not coagulation monitoring, and viscoelastic testing was not performed.
An elevated PT/INR in FHF reflects a dysfunction or decreased production of the coagulation factors but is not necessarily a bleeding risk. This is especially true for factor VII, which has the shortest half-life of all the procoagulant factors (approximately 3-6 h) [17]. A dysfunction of coagulation factors does not translate to a dysfunction of hemostasis since adequate hemostasis does not require 100% of coagulation factors [18]. While FHF patients may have lower coagulation factors, they also have decreased anticoagulant protein C [19]. As a result, FHF patients can have normal clotting potential despite an elevated PT/INR.
Recent evidence has suggested that viscoelastic tests of coagulation, such as ROTEM, offer better clinical utility in assessing hemostatic function in patients with liver disease, including FHF [20]. This is because while PT/INR is analyzed from isolated plasma and its value is generated at the initiation of fibrin polymerization, ROTEM is analyzed from whole-blood samples and evaluates the kinetics and coagulation from clot initiation, propagation, stabilization, and lysis. This reflects a much more comprehensive picture of coagulation status, capturing the importance of plasma, blood cells, and platelets during hemostasis. Secondly, ROTEM considers the levels of pro- and anticoagulants, which are both decreased in FHF, and therefore the coagulation balance is maintained. In contrast, PT/INR only considers procoagulant levels, especially factor VII.
Most liver transplantation anesthesiologists understand that PT/INR is not reflective of the patient’s whole-blood coagulation status and is not an indication to transfuse FFP. However, an INR of >8.71 is rarely seen and would generally lead physicians to transfuse FFP prior to an invasive procedure, mainly due to a fear of spontaneous bleeding or continuous bleeding from the procedure site. However, in FHF, the risk of spontaneous bleeding related to coagulation defects is unlikely. Munoz et al analyzed more than 1000 FHF cases and found minor gastrointestinal bleeding in only 6.6% of cases, with no significant difference in PT/INR between patients who bled versus those who did not [21]. Stravitz et al studied 1770 FHF cases and reported bleeding complications in 11% of cases, with no difference in PT/INR between FHF patients who bled versus those who did not [22]. Further, Fisher and Mutimer found no major vascular complications attributed to an elevated INR in a prospective audit of 580 central line placements in liver disease patients with an INR >1.5 [23].
According to the 2015 Practice Guidelines for Perioperative Blood Management from the American Society of Anesthesiologists, prophylactic blood products are not indicated if there is no bleeding, regardless of laboratory results [24]. There is also no clear evidence that prophylactic administration of FFP and cryoprecipitate improves outcomes when used solely to correct PT/INR in FHF patients based on conventional coagulation testing. One small randomized trial showed that prophylactic administration of FFP had no influence on mortality in patients with FHF with abnormal PT/INR and no active bleeding [25]. FFP used to correct coagulopathy in FHF has a high potential to cause volume-overload acute lung injury, hypersensitivity reactions, and nosocomial infections [26,27]. The main cause is the large volume needed, which is about 15 to 20 mL of FFP per kilogram of body weight to achieve any hemostatic effect [28]. To avoid large-volume transfusion, PCC has been studied as an alternative in liver transplantation. A retrospective review from Kirchner et al found that ROTEM-guided first line hemostatic therapy with fibrinogen concentrate and PCC did not appear to increase the risk of thrombotic, thromboembolic, or ischemic events in liver transplant patients [29].
In this case, the patient received FFP and cryoprecipitate based on conventional coagulation tests and under the assumption that it would correct whole-blood coagulation abnormalities. However, physicians should be encouraged to utilize viscoelastic testing over conventional coagulation testing to assess bleeding risk and guide FFP transfusions. Dotsch et al reported that ROTEM was a better predictor of postoperative bleeding than plasma fibrinogen concentration [30]. Multiple studies found that thromboelastography-guided transfusion decreased FFP transfusions and intraoperative blood loss and was superior to conventional coagulation tests [31–34]. The International Liver Transplantation Society (ILTS) ERAS4OLT.org Consensus
Conference on Enhanced Recovery for Liver Transplantation recommends viscoelastic tests over conventional coagulation tests to guide transfusion management [35].
Conclusions
Patients with FHF can have normal whole-blood coagulation based on ROTEM, even if INR levels are unmeasurably high. Viscoelastic tests such as ROTEM, which assesses whole-blood coagulation properties, are preferable for coagulation monitoring in these patients. Transfusion with blood products like FFP and cryoprecipitate can be used based on the result of visco-elastic testing over conventional coagulation testing.
References:
1.. Yoon E, Babar A, Choudhary M, Acetaminophen-induced hepatotoxicity: A comprehensive update: J Clin Transl Hepatol, 2016; 28; 131-42
2.. Guengerich FP, Cytochrome P450 2E1 and its roles in disease: Chem Biol Interact, 2020; 1; 322 :109056
3.. More SS, Nugent J, Vartak AP, Hepatoprotective effect of γ-glutathione in a murine model of acetaminophen-induced liver toxicity: Chem Res Toxicol, 2017; 30; 777-84
4.. Chiew AL, Gluud C, Brok J, Buckley NA, Interventions for paracetamol (acetaminophen) overdose: Cochrane Database Syst Rev, 2018; 23(2); CD003328
5.. Gish RG, Brothers JM, Current observations in the management of hypoand hypercoagulability in patients with acute or chronic liver failure: Gastroenterol Hepatol, 2021; 17; 23-26
6.. Shikdar S, Vashisht R, Bhattacharya PT, International normalized ratio (INR): StatPearls [Internet], 2022, Treasure Island (FL), StatPearls Publishing
7.. Hartert H, [Blood clotting studies with Thrombus stressography; A new Investigation procedure.]: Klin Wochenschr, 1948; 26; 577-83
8.. Kang YG, Martin DJ, Marquez J, Intraoperative changes in blood coagulation and thrombelastographic monitoring in liver transplantation: Anesth Analg, 1985; 64; 888-96
9.. Yoon U, Lai M, Nguyen T, Elia E, Perioperative viscoelastic assay use for monitoring coagulation among US Liver Transplantation Centers: Transplant Proc, 2021; 53; 2312-17
10.. Veigas PV, Callum J, Rizoli S, A systematic review on the rotational thrombelastometry (ROTEM®) values for the diagnosis of coagulopathy, prediction and guidance of blood transfusion and prediction of mortality in trauma patients: Scand J Trauma Resusc Emerg Med, 2016; 24; 114
11.. Li C, Zhao Q, Yang K, Thromboelastography or rotational thromboelastometry for bleeding management in adults undergoing cardiac surgery: A systematic review with meta-analysis and trial sequential analysis: J Thorac Dis, 2019; 11; 1170-81
12.. Theusinger OM, Nürnberg J, Asmis LM, Rotation thromboelastometry (ROTEM) stability and reproducibility over time: Eur J Cardiothorac Surg, 2010; 37; 677-83
13.. Munoz SJ, Stravitz RT, Gabriel DA, Coagulopathy of acute liver failure: Clin Liver Dis, 2009; 13; 95-107
14.. Mallett S, clinical utility of viscoelastic tests of coagulation (TEG/ROTEM) in patients with liver disease and during liver transplantation: Semin Thromb Hemost, 2015; 41; 527-37
15.. Austin EB, Hobbs H, Crouse BA, Lobos AT, A case report of full recovery from severe cerebral edema secondary to acetaminophen-induced hepatotoxicity in a 13 year old girl: BMC Pediatr, 2018; 18; 247
16.. Epperson LC, Weiss ST, Cao DJ, A case report of a severe, unusually delayed anaphylactoid reaction to intravenous n-acetylcysteine during treatment of acute acetaminophen toxicity in an adolescent: J Med Toxicol, 2021; 17; 75-79
17.. Lichtman MA, Molecular biology and biochemistry of the coagulation factors and pathways of hemostasis: Williams Hematology, 2010, New York, NY, The McGraw-Hill Companies chapter 113
18.. Mintz PD, Transfusion therapy: Clinical principles and practice: AABB Press, 2011; 931
19.. Yamaguchi M, Gabazza EC, Taguchi O, Decreased protein C activation in patients with fulminant hepatic failure: Scand J Gastroenterol, 2006; 41; 331-37
20.. Mallett S, Clinical utility of viscoelastic tests of coagulation (TEG/ROTEM) in patients with liver disease and during liver transplantation: Semin Thromb Hemost, 2015; 41; 527-37
21.. Munoz SJ, Rajender Reddy K, Lee W, The coagulopathy of acute liver failure and implications for intracranial pressure monitoring: Neurocrit Care, 2008; 9; 103-7
22.. Stravitz RT, Ellerbe C, Durkalski V, Bleeding complications in acute liver failure: Hepatology, 2018; 67; 1931-42
23.. Fisher NC, Mutimer DJ, Central venous cannulation in patients with liver disease and coagulopathy – a prospective audit: Intensive Care Med, 1999; 25; 481-85
24.. , Practice guidelines for perioperative blood management: Anesthesiology, 2015; 122; 241-75
25.. Gazzard BG, Henderson JM, Williams R, Early changes in coagulation following a paracetamol overdose and a controlled trial of fresh frozen plasma therapy: Gut, 1975; 16; 617-20
26.. Toy P, Gajic O, Bacchetti P, Transfusion-related acute lung injury: Incidence and risk factors: Blood, 2012; 119; 1757-67
27.. Khan H, Belsher J, Yilmaz M, Fresh-frozen plasma and platelet transfusions are associated with development of acute lung injury in critically ill medical patients: Chest, 2007; 131; 1308-14
28.. Rossaint R, Bouillon B, Cerny V, The European guideline on management of major bleeding and coagulopathy following trauma: Fourth edition: Crit Care, 2016; 12; 100
29.. Kirchner C, Dirkmann D, Treckmann JW, Coagulation management with factor concentrates in liver transplantation: A single-center experience: Transfusion, 2014; 54; 2760-68
30.. Dötsch TM, Dirkmann D, Bezinover D, Assessment of standard laboratory tests and rotational thromboelastometry for the prediction of postoperative bleeding in liver transplantation: Br J Anaesth, 2017; 119; 402-10
31.. Wang S-C, Shieh J-F, Chang K-Y, Thromboelastography-guided trans-fusion decreases intraoperative blood transfusion during orthotopic liver transplantation: Randomized clinical trial: Transplant Proc, 2010; 42; 2590-93
32.. Smart L, Mumtaz K, Scharpf D, Rotational thromboelastometry or conventional coagulation tests in liver transplantation: Comparing blood loss, transfusions, and cost: Ann Hepatol, 2017; 16; 916-23
33.. Wikkelsø A, Wetterslev J, Møller AM, Afshari A, Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding: Cochrane Database Syst Rev, 2016; 2016(8); CD007871
34.. Yeom RS, Wang XA, Elia E, Yoon U, Severe congenital factor VII deficiency with normal perioperative coagulation profile based on ROTEM analysis in a hepatectomy: Am J Case Rep, 2021; 22; e930245
35.. Yoon U, Bartoszko J, Bezinover D, org Working Group. Intraoperative transfusion management, antifibrinolytic therapy, coagulation monitoring and the impact on short-term outcomes after liver transplantation – a systematic review of the literature and expert panel recommendations: Clin Transplant, 2022; 6; 14637
Figures
In Press
04 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.941835
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250