18 April 2023: Articles 
Thoracic Epidural as a Rescue Analgesic in a Patient with a Continuous Erector Spinae Plane Block for Rib Fractures: A Case Report
Unusual or unexpected effect of treatment
Ian J. Coblentz1CDEF*, Brian M. Ilfeld1DE, John J. Finneran IV1BCDEFDOI: 10.12659/AJCR.938875
Am J Case Rep 2023; 24:e938875
Abstract
BACKGROUND: Rib fractures are a common traumatic injury with significant morbidity and mortality resulting from respiratory compromise. Regional anesthetic techniques have demonstrated efficacy in reducing morbidity and mortality from rib fractures, but there is limited evidence comparing various techniques, and in complex trauma patients various factors may preclude the use of neuraxial and other techniques.
CASE REPORT: We report the case of a 72-year-old man who presented with left 4th-11th rib fractures. He was initially managed with a continuous erector spinae plane catheter, which resulted in improved pain and incentive spirometry. Unfortunately, he continued to decline and ultimately was rescued from impending respiratory failure by placement of a T6-T7 epidural catheter and epidural infusion of bupivacaine.
CONCLUSIONS: This case report suggests that a continuous erector spinae plane block may be a useful regional anesthesia technique in the management of rib fractures through its potential to improve pain control and increase incentive spirometry volumes. It also suggests that there may be limitations to its utility given the continued decline of the patient, who was eventually rescued from respiratory failure by placement of a thoracic epidural. Unique to erector spinae plane blocks are the ability to be managed in the outpatient setting, improved safety profile, ease of placement, and potential to be placed in patients with coagulopathy and on anticoagulation therapies.
Keywords: Analgesia, Epidural, Anesthesia, Epidural, Rib Fractures, Male, Humans, Aged, Nerve Block, pain management, Pain, Analgesics
Background
Rib fractures are a common injury occurring in about 10% of all trauma patients, and are a source of significant morbidity and mortality [1]. Pain frequently limits the ability of patients with rib fractures to cough and deeply inspire. These impaired respiratory mechanics may cause splinting and hypoventilation, resulting in atelectasis, pneumonia, and other respiratory complications [1]. Additionally, rib fractures are rarely isolated injuries, and underlying injuries such as pulmonary contusion, lacerations, and hemo- and pneumothorax often further impair respiratory mechanics and gas exchange. Increasing age and number of fractures are also associated with a higher mortality, with patients with 7 or more rib fractures having a mortality rate approaching 30% [2,3].
Pain control following rib fractures is, therefore, critical to improve respiratory mechanics, facilitate secretion clearance, and limit complications. Neuraxial anesthetic techniques, such as thoracic epidurals and paravertebral blocks, have been demonstrated to decrease pulmonary complications and mortality in patients with traumatic rib fractures [4,5]. However, in complex trauma patients, various factors frequently preclude the use of epidural or paravertebral analgesia (eg, coagulopathy, hemodynamic instability, spinal trauma). In addition, epidural catheterization – perhaps the “Gold Standard” for providing analgesia following rib fractures – precludes discharge of these patients.
Given the limitations of neuraxial techniques for rib fractures, there has been a recent trend toward using “fascial plane blocks” such as the erector spinae plane (ESP) block to provide post-rib fracture analgesia [6]. Continuous ESP blocks are within the standard of care for management of rib fractures, and have theoretical advantages compared to neuraxial blocks (eg, can be performed in the setting of coagulopathy or systemic anticoagulation, can be provided on an outpatient basis, and have a probable lower risk of pneumothorax or spinal cord trauma) [6,7]. Nevertheless, the relative analgesic potency of fascial plane vs neuraxial local anesthetic deposition remains unknown; without comparative evidence of risk versus benefit, clinicians may be unsure of how to apply the broad standard of care for rib fractures and select the most efficacious technique for the individual patient. The following case report aims to provide insight into how this standard of care and various regional techniques may be applied.
Case Report
A 72-year-old man with a history of atrial fibrillation, type-2 diabetes, and chronic obstructive pulmonary disease with a 55 pack-year smoking history presented after a ground-level fall with left-sided 4th–11th rib fractures and associated hemopneumothorax (Figures 1, 2). A chest tube was placed in the Emergency Department and the patient was admitted to the Intensive Care Unit for continued pain control and monitoring of respiratory status. After admission, the patient rated his pain with incentive spirometry as a 10 on a 0–10 numeric rating scale and was able to achieve a spirometry volume of 750 milliliters (mL). In the setting of the early phase of the COVID-19 pandemic, the patient was very concerned about and wanted to avoid intubation. The Regional Anesthesia and Acute Pain Medicine service was consulted for a possible regional analgesic intervention and proposed a unilateral continuous ESP block.
Using a 5- to 2-Megahertz, 30-centimeter, curvilinear array ultrasound probe (Edge II; SonoSite, Bothell, WA), the left 8th thoracic vertebral transverse process and erector spinae muscle were identified. A 17-gauge (G) Tuohy needle (FlexTip Plus; Teleflex Medical, Research Triangle Park, NC) was inserted using an in-plane, caudal-to-cranial approach. Ropivacaine 0.5% containing 1: 400,000 dilution of epinephrine (20 mL) was injected into the plane deep to the erector spinae muscle. A flexible, 19G catheter was inserted 4 centimeters into this plane and secured at the skin. A continuous basal infusion of 0.2% ropivacaine was initiated at 20 mL/h.
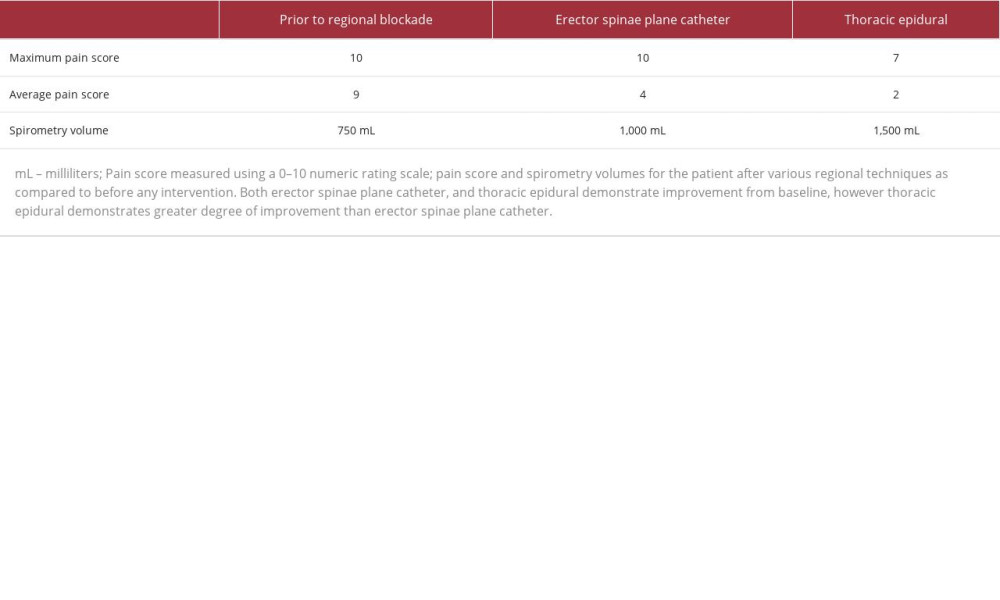
Following this intervention, the patient’s reported average pain score improved from 9 to 4 on the 0–10 NRS and spirometry volumes increased from 750 mL to 1000 mL, although maximum pain score during spirometry and coughing remained unchanged at 10 (Table 1). Despite this intervention and improvement in incentive spirometry and pain, the patient’s respiratory status deteriorated over the subsequent 12 hours and the oxygen requirements delivered by facemask increased. In the early morning following the block, arterial blood gas demonstrated hypercarbic respiratory acidosis (pH 7.27, PaCO2 75, PaO2 79, on 15 liters/minute oxygen by facemask). The patient continued to refuse intubation as recommended by the critical care team.
The regional anesthesia team re-evaluated the patient approximately 15 hours following the ESP block and proposed thoracic epidural placement. The ESP catheter was removed without difficulty and an epidural catheter was inserted between the 6th and 7th thoracic levels using a conventional loss of resistance technique with air and a negative 3 mL test dose (1.5% lidocaine with 1: 200 000 epinephrine). After securing the catheter, an infusion of 0.1% bupivacaine was initiated (10 mL/hour basal, 5 mL patient-controlled bolus, 30-minute lockout). Following placement of the thoracic epidural, the patient’s average pain was reduced to a 2 on a 0–10 numeric rating scale, and pain during spirometry and coughing reduced from 10 to 7. Incentive spirometry further increased from 1000 mL to 1500 mL (Table 1). Arterial blood gas 6 hours following epidural placement revealed a marked improvement in his respiratory acidosis (pH 7.39, PaCO2 49, PaO2 70, on 2 L/min oxygen by nasal cannula). Eight days following placement, the epidural catheter was removed. The patient was discharged from the hospital 15 days after the initial injury.
Discussion
While this patient continued to decline clinically after initial treatment with a continuous ESP block and was ultimately rescued from impending intubation by a thoracic epidural, we suggest that this is not evidence against the use of a continuous ESP catheter in rib fracture patients. This report supports the use of a continuous ESP catheter in the management of rib fractures because average pain scores at rest were improved after placement of the initial ESP block, and incentive spirometry values were increased, indicating the aims of therapy were met. Further, the improvement in analgesia and incentive spirometry persisted with the continuous infusion of ropivacaine via the catheter after the likely resolution of the single-injection ESP block. Despite these improvements, the patient continued to deteriorate clinically. This supports the notion that there is not a single best regional anesthetic for all rib fractures. Overall, rib fracture severity and clinical context requires evaluation of the merits and harms of various regional anesthesia techniques in the hopes of selecting the most effective technique at the onset of patient care.
Thoracic epidurals have previously been viewed as the ‘gold standard’ in analgesic management of rib fractures and have been demonstrated to provide superior analgesia compared to intercostal blocks and intravenous analgesia [4]. However, growing evidence demonstrates analgesia can be provided by less invasive, more portable, and lower-risk alternatives such as paravertebral blocks, erector spinae plane blocks, and serratus anterior plane blocks [8,9]. One of the notable benefits of thoracic epidural analgesia is an ability to provide analgesia for bilateral rib fractures with a single procedure as opposed to the unilateral analgesia of other regional techniques.
Despite the effectiveness of thoracic epidurals, there are significant contraindications and limitations to utilization.
Anticoagulation, which is often necessary in trauma patients and other medical conditions, may limit candidacy for epidural placement [10]. Spinal and head trauma may also preclude use of epidural analgesia [5]. Additionally, epidurals require technical skill for successful placement, and are recommended to have close monitoring for the development of complications, necessitating hospital admission and nursing resources, and thereby limiting availability [11]. In contrast, continuous erector spinae plane blocks are not limited by anticoagulation or coagulopathy. The skill level necessary for thoracic epidurals and paravertebral blocks essentially limits utilization to anesthesiologists, but erector spinae plane blocks may be easier to insert for a variety of providers, which can help to increase utilization in areas such as Emergency Departments and Urgent Care centers. Thoracic epidurals physically tether a patient to the hospital environment, but continuous erector spinae plane catheters have demonstrated safety and efficacy in outpatient use, which can limit the burden on hospital resources [7]. Lastly, the risk of complications with continuous ESP catheters is low, and may be more favorable in trauma patients who may otherwise be unable to tolerate complications such as pneumothorax, epidural hematomas, and spinal cord injuries [5,6,9,12].
Further research is indicated in the form of randomized, controlled trials to further compare and quantify the benefits of continuous ESP block in providing analgesia for rib fractures in comparison with other regional anesthetics. In patients with significant chest wall trauma (eg, numerous or bilateral fractured ribs, chest tube requirement, flail chest) such as our patient, thoracic epidural analgesia may continue to be the “Gold Standard” for chest wall analgesia; however, the limited contraindications, decreased technical skill, and applicability to outpatient management without significant compromise in effective analgesia make continuous ESP blocks an alternative worthy of consideration in select patients.
Conclusions
Given the significant morbidity and mortality associated with rib fractures, it is important to utilize effective and safe methods of analgesia and improve pulmonary function. A variety of regional anesthesia techniques have been reported in the literature for providing analgesia and supporting pulmonary function in this patient population. In this patient with extensive left-sided fractures of the 4th–11th ribs, an initial continuous ESP catheter did provide some improvement, but ultimately did not stop further clinical decline. The patient was rescued from further decline by placement of a thoracic epidural. While further studies are necessary to better compare these techniques and develop selection criteria, there are certain advantages to the use of ESP blocks in rib fractures, including potential for outpatient management, improved safety profile, ease of placement, and a lack of contraindications associated with coagulopathy/anticoagulation as compared to neuraxial techniques.
Figures
References:
1.. Ziegler DW, Agarwal NN, The morbidity and mortality of rib fractures: J Trauma Inj Infect Crit Care, 1994; 37(6); 975-79
2.. Flagel BT, Luchette FA, Reed RL, Half-a-dozen ribs: The breakpoint for mortality: Surgery, 2005; 138(4); 717-25
3.. Holcomb JB, McMullin NR, Kozar RA, Morbidity from rib fractures increases after age 45: J Am Coll Surg, 2003; 196(4); 549-55
4.. Bulger EM, Edwards T, Klotz P, Jurkovich GJ, Epidural analgesia improves outcome after multiple rib fractures: Surgery, 2004; 136(2); 426-30
5.. Malekpour M, Hashmi A, Dove J, Analgesic choice in management of rib fractures: Paravertebral block or epidural analgesia?: Anesth Analg, 2017; 124(6); 1906-11
6.. Adhikary SD, Liu WM, Fuller E, The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: A retrospective cohort study: Anaesthesia, 2019; 74(5); 585-93
7.. Finneran JJ, Alexander B, Bechis SK, Continuous erector spinae plane blocks with automated boluses for analgesia following percutaneous nephrolithotomy: Korean J Anesthesiol, 2021; 74(2); 178-80
8.. Peek J, Smeeing DPJ, Hietbrink F, Comparison of analgesic interventions for traumatic rib fractures: A systematic review and meta-analysis: Eur J Trauma Emerg Surg, 2019; 45(4); 597-622
9.. Williams A, Bigham C, Marchbank A, Anaesthetic and surgical management of rib fractures: BJA Educ, 2020; 20(10); 332-40
10.. Horlocker TT, Vandermeuelen E, Kopp SL, Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (fourth edition): Reg Anesth Pain Med, 2018; 43(3); 263-309
11.. Tran DQH, Van Zundert TCRV, Aliste J, Engsusophon P, Finlayson RJ, Primary failure of thoracic epidural analgesia in training centers: The invisible elephant?: Reg Anesth Pain Med, 2016; 41(3); 309-13
12.. Forero M, Adhikary SD, Lopez H, The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain: Reg Anesth Pain Med, 2016; 41(5); 621-27
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250