21 July 2020: Articles 
A Rare Case of Non-Prosthetic Aortic Valve Infectious Endocarditis Caused by
Rare disease
Ricardo Lessa de Castro1ABCDEF*, Neiberg de Alcantara Lima1CDEF, Danielli Oliveira da Costa Lino2BCDF, Thomas Austin Melgar1ACDEFDOI: 10.12659/AJCR.923031
Am J Case Rep 2020; 21:e923031
Abstract
BACKGROUND: Achromobacter xylosoxidans is a ubiquitous environmental gram-negative bacterium, very resistant to antibiotics. Endocarditis caused by these bacteria is extremely rare, with only 20 cases described in the literature to our knowledge. Mortality rates are high, and treatment usually involves a combination of antibiotics and surgery. Nosocomial infections predominate with a strong association between bacteremia and immunosuppression.
CASE REPORT: A 19-year-old immunocompetent male presented with endocarditis He had interatrial and interventricular communication corrected at age 11 months and aortic coarctation correction at age 10. Initial echocardiogram showed a possible interventricular patch infection, which was later ruled out. He was treated initially for endocarditis with a combination of antibiotics, but because he remained febrile after appropriate antibiotic treatment, surgery was performed. The patient had a favorable outcome after surgery and was asymptomatic on follow-up.
CONCLUSIONS: Endocarditis caused by A. xylosoxidans is extremely rare. To date, only 20 cases of IT have been reported in the literature, of which only two involved a native valve. Given the scarcity of cases reported, there is no consensus on the best treatment.
Keywords: Achromobacter denitrificans, Endocarditis, Bacterial, Heart Valves, Aortic Valve, Child, Endocarditis, Gram-Negative Bacterial Infections, Infant, young adult
Background
Case Report
A 19-year-old man presented with a history of approximately 1 month of intermittent fevers, chills, dry cough, and pleuritic chest pain. He lost about 10 lb during this period and had progressive fatigue. He had a medical history of interatrial and interventricular communication corrected at 11 months of age and aortic coarctation correction at age 10.
On examination, the patient was febrile, tachycardic, and his blood pressure was 125 over 76 mmHg. Physical exam demonstrated diastolic aortic murmur, grade 3/6, compatible with aortic insufficiency. There was no jugular vein distention, the lung exam was clear, and there were no petechiae or signs of skin lesions. The rest of the patient’s physical exam was normal. Laboratory testing revealed an elevated white blood cell count of 16.45 109/L and microcytic anemia with hemoglobin of 9.1 g/dL and mean corpuscular volume of 78 fL. Creatinine was 0.71 mg/dL with a glomerular filtration rate above 60 mL/min. An HIV test done on our patient was negative. Chest x-ray showed signs of mild pulmonary congestion and an enlarged cardiac silhouette. An echocardiogram revealed a moderate left atrium enlargement and eccentric left ventricular hyper-trophy with an ejection fraction of 47%. A filamentous structure was also seen inside the patient’s left ventricle, adherent to a bicuspid aortic valve, and the ventricular patch in his inter-ventricular septum and severe aortic insufficiency. A diagnosis of endocarditis was given and the patient was placed on gentamicin, oxacillin, and ceftriaxone.
Two sets of blood cultures collected on the patient’s admission were positive for presence of
During the surgery, vegetation was seen on the patient’s aortic valve but not on his ventricular patch. Culture of the vegetation showed
On the fourth day of the patient’s hospitalization, he had a spontaneous right-sided pneumothorax, with no apparent cause, which was drained and resolved after 3 days. He went home 10 days after surgery and completed 28 days of carbapenem. His immediate and 30-day echocardiograms at follow-up did not show any vegetation. He was symptomatic at his 6-month and 1-year follow-up appointments.
Discussion
Endocarditis is dangerous and difficult to treat. Prolonged fevers with weight loss in patients with a previous history of heart disease, especially after cardiac surgeries, should raise suspicion of this diagnosis.
A recent review published by Barragan, et al. showed that in the majority of cases, patients were immunocompromised and almost all had acquired their infections in the hospital [7]. Reviewing our patient’s records, he had no history of recent or recurrent illnesses or hospitalizations. In most patients, infections associated with this pathogen are related to catheters [7,8] but in our report, we do not have a clear source of his infection.
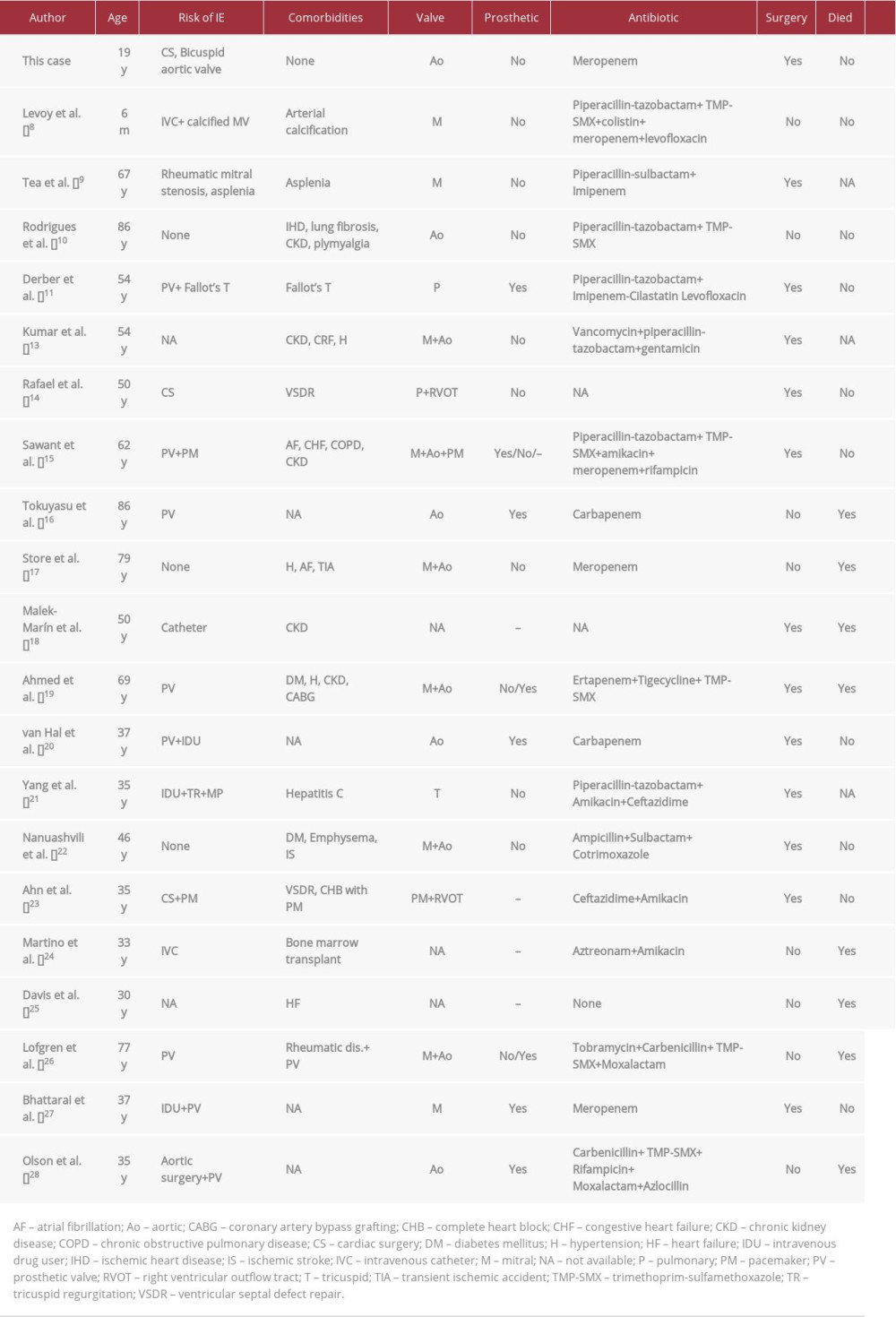
To date, only 20 cases (Table 1) of
Given the scarcity of the cases reported, there is no consensus on the best treatment for
In contrast to use of a percutaneous atrial septal occluder device, surgical patch closure of atrial septal defects is known to represent no risk infective endocarditis [12]. To our knowledge, only two cases of endocarditis on a surgical patch of a ventricular septal defect have been reported [12]. Considering these previous case reports, it would be unlikely for our patient to have an infection in his patch. However, his bicuspid aortic valve increases his risk of developing endocarditis.
Conclusions
We presented an uncommon and rare case of
References:
1.. Xia R, Otto C, Zeng J, Achromobacter endocarditis in native cardiac valves – an autopsy case report and review of the literature: Cardiovasc Pathol, 2018; 36; 6-10
2.. Manfredi R, Nanetti A, Ferri M, Chiodo F: Eur J Clin Microbiol Infect Dis, 1997; 16(12); 933-38
3.. Baddour LM, Wilson WR, Bayer AS, Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: A scientific statement for healthcare professionals from the American Heart Association: Circulation, 2015; 132; 1435-86
4.. Ohyama A, Yabuuchi O: Jpn J Microbiol, 1971; 15(70028); 477-81
5.. Shigeta S, Yasunaga Y, Honzumi K: J Clin Pathol, 1978; 31(2); 156-61
6.. Igra-Siegman Y, Chmel H, Cobbs C: J Clin Microbiol, 1980; 11(2); 141-45
7.. Barragán EP, Pérez JS, Corbella L: Rev Esp Quimioter, 2018; 31(3); 268-73
8.. Levoy CS, Hall DJ, Berman D: JMM Case Rep, 2015; 2(6); 1-4
9.. Tea I, Caruso M, Gary P: J Am Coll Cardiol, 2019; 73(9 Suppl. 1); 2999
10.. Rodrigues CG, Rays J, Kanegae MY: Autops Case Rep, 2017; 7(3); 50-55
11.. Derber C, Elam K, Forbes BA, Bearman G, Achromobacter species endocarditis: A case report and literature review: Can J Infect Dis Med Microbiol, 2011; 22(3); e17-e20
12.. Honnorat E, Seng P, Riberi A, Late infectious endocarditis of surgical patch closure of atrial septal defects diagnosed by 18F-fluorodeoxyglucose gated cardiac computed tomography (18F-FDG-PET/CT): A case report: BMC Res Notes, 2016; 9(1); 16-19
13.. Kumar S, Khaira J, Penigalapati D, Apurva A: J Glob Infect Dis, 2017; 9(2); 85
14.. Rafael AE, Keshavamurthy S, Sepulveda E, Intracardiac abscess with cutaneous fistula: Secondary to ventricular septal defect repair simulating sternal wound infection: Texas Hear Inst J, 2014; 41(3); 324-26
15.. Sawant AC, Srivatsa SS, Castro LJ: Texas Hear Inst J, 2013; 40(1); 95-98
16.. Tokuyasu H, Fukushima T, Nakazaki H, Shimizu E: Intern Med, 2012; 51(9); 1133-38
17.. Storey A, Wilson A, McWilliams E: BMJ Case Rep, 2010; 2010; bcr0620103104
18.. Malek-Marín T, Arenas MD, Perdiguero M, A case of endocarditis of difficult diagnosis in dialysis: Could “pest” friends be involved?: Clin Nephrol, 2009; 72(5); 405-9
19.. Ahmed MS, Nistal C, Jayan R: Clin Nephrol, 2009; 71(3); 350-54
20.. Van Hal S, Stark D, Marriott D, Harkness J: J Med Microbiol, 2008; 57(4); 525-27
21.. Yang CH, Shih NC, Lu DCT: J Intern Med Taiwan, 2007; 18(4); 212-16
22.. Nanuashvili A, Kacharava G, Jashiashvili N: Euro Surveill, 2007; 12(5); E070524.2
23.. Ahn Y, Kim NH, Shin DH: J Korean Med Sci, 2004; 19(2); 291-93
24.. Martino P, Micozzi A, Venditti M, Catheter-related right-sided endocarditis in bone marrow transplant recipients: Rev Infect Dis, 1990; 12(2); 250-57
25.. Davis M, Gratten M, Ree GH: PNG Med J, 1982; 25(1); 7-11
26.. Lofgren RP, Nelson AE, Crossley KB: Am Heart J, 1981; 101(4); 502
27.. Bhattarai M, Papireddy M, Kulkarni S, A rare case of complicated Achromobacter xylosoxidans endocarditis and its successful management: J Hosp Med, 2016; 11(Suppl 1) http://www.shmabstracts.com/abstract/a-rare-case-of-complicated-achromobacter-xylosoxidans-endocarditis-and-its-successful-management
28.. lson DA, Hoeprich PD: West J Med, 1982; 136(2); 153-57
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250