05 July 2020: Articles 
Coccidioidomycosis and Pulmonary Emboli: A Report of 5 Cases
Challenging differential diagnosis, Management of emergency care, Rare coexistence of disease or pathology
John G. Prichard1BEF*, Michelle B. Azimov23BEF, Karlos Z. Oregel2BEDOI: 10.12659/AJCR.924179
Am J Case Rep 2020; 21:e924179
Abstract
BACKGROUND: Coccidioidomycosis is endemic to the Sonoran life zone, which extends from Latin America to the western United States. The principle manifestation is pneumonia but disseminated disease also occurs. Venous thromboembolism occurring in association with this disease has not been reported. We encountered 5 cases of coccidioidomycosis, each complicated by pulmonary emboli, during a single year. We report these cases with the intent of making those caring for patients with coccidioidomycosis aware of this association.
CASE REPORT: A 35-year-old man developed fever and respiratory symptoms. He was initially treated with antibiotics as an outpatient and during a subsequent hospitalization. He was readmitted because of persistent respiratory symptoms and treated presumptively for coccidioidomycosis pneumonia. Hypoxemia persisted and multiple acute pulmonary emboli were evident on imaging. Serological study and organism identification confirmed a diagnosis of coccidioidomycosis infection. Details of this case and 4 additional cases are described.
CONCLUSIONS: Venous thromboembolism occurred in 5 patients with pulmonary coccidioidomycosis. The etiology of this rare association remains unclear but could be related to regional environmental changes that preceded the appearance of these cases.
Keywords: Coccidioidomycosis, Pulmonary Embolism, venous thromboembolism, California, Dyspnea, Endemic Diseases, Fever, Tomography, X-Ray Computed
Background
Case Reports
A 35-year-old man was well until fever and dyspnea occurred. Two weeks later he was seen by a physician and treated with an oral antibiotic. Symptoms persisted, and he was admitted to a neighboring hospital. A computed tomography (CT) scan of his chest revealed right lower and right upper lobe infiltrates with ipsilateral hilar adenopathy. Intravenous antibiotics were administered, and he was discharged after several days. Symptoms of fever, night sweats, pleuritic chest pain, and dyspnea worsened, and he was admitted to our hospital.
Physical examination disclosed an obese Latino male, awake and alert, in mild respiratory distress. Respiratory rate was 19 breaths per minute and oxygen saturation was 94% on room air. Blood pressure was normal. The temperature was 100.8°F (38.2°C). Breath sounds were diminished over the right hemi thorax, with diffuse crackles. Examination of the heart, abdomen, extremities, and neurological system was unremarkable. He had no adenopathy or rash.
Laboratory studies showed a white blood count of 13 600/μL (normal: 4800–10 800/μL). Hemoglobin was 14.3 gm/dL (normal: 14–18 gm/dL) and the platelet count was 485 000/μL (normal 130 000–400 000/μL). A differential count showed 73% neutrophils, 13% lymphocytes, 9.6% monocytes, 2.8% eosinophils, and 1.3% basophils. Erythrocyte sedimentation rate was 80 mm/hr (normal: 0–15 mm/hr). C reactive protein was 9.74 (normal: 0.05–0.3 mg/dL). Serologic assay for human immuno-deficiency virus was negative, as was a QuantiFERON-TB Gold assay for tuberculosis. PCR assay for influenza A and B was negative. Urinary Legionella antigen was negative by enzyme immunoassay (EIA). Serologic assay for Mycoplasma antibodies was also negative.
Vancomycin and Ceftriaxone were administered but were discontinued after 24 hours once it was determined by review of records that he had received 6 different antibiotics over the preceding 4 weeks. Fluconazole 800 mg was given orally, as coccidioidomycosis was considered the most likely diagnosis. Enoxaparin 40 mg was administered daily by subcutaneous injection during the hospitalization. It was necessary to discontinue the anticoagulant prophylaxis from time to time because of invasive procedures, in which case intermittent pneumatic compression stockings were utilized.
Repeat chest CT showed right upper lobe, right middle lobe, left mid-lung infiltrates, and multiple cavitary lesions. Blood and sputum cultures remained negative. Fever persisted up to 103°F (39.4°C). A bronchoscopy was performed on the sixth hospital day. On the eighth hospital day, fever and increasing oxygen requirement prompted another chest CT, which showed extensive emboli in the left lower lobe pulmonary artery (Figure 1). Mediastinal adenopathy was more prominent; pulmonary infiltrates and cavities were unchanged. A venous ultrasound showed bilateral posterior tibial and left peroneal vein thrombi. Factor V Leiden and prothrombin gene mutations by PCR assay were negative. He was placed on rivaroxaban 20 mg. Immunodiffusion assay for coccidioidomycosis returned as positive, and the complement fixation assay was reported at 1: 32. Bronchial alveolar lavage fluid grew
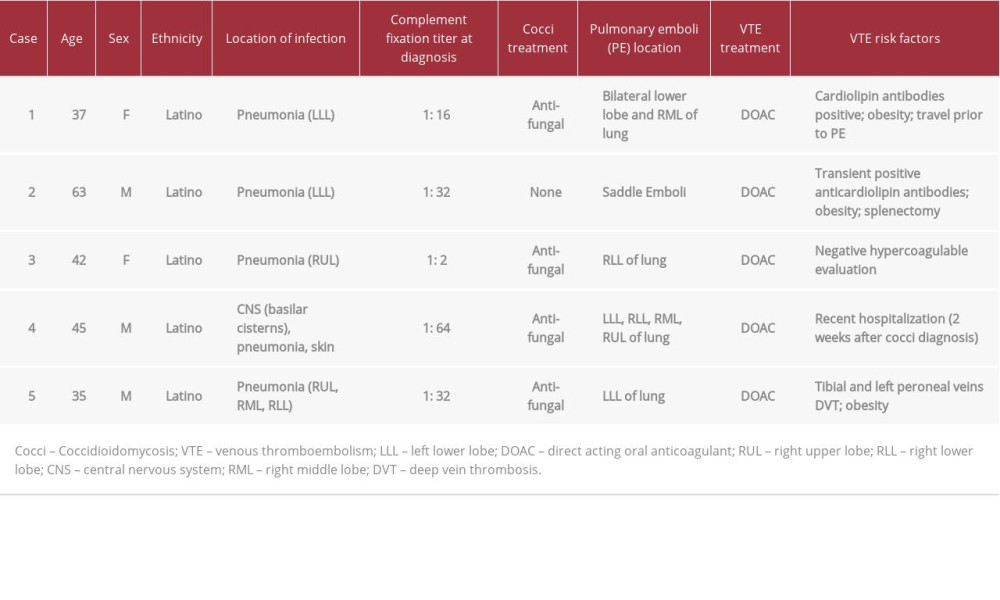
A summary of all 5 cases is shown in Table 1. All patients were treated with rivaroxaban because of lesser drug–drug interactions with fluconazole.
Discussion
Infection is associated with a thrombophilic state through a variety of mechanisms, resulting in activation of the coagulation cascade and decreased fibrinolysis [3]. Such activation can occur regardless of the infecting organism [4] or its chronicity [5]. Despite the relatively large number of cases diagnosed in our area [6], we had not, in our collective memory, seen VTE complicate the course of coccidioidomycosis, even in those with severe disease and prolonged hospitalization. We searched the medical literature using medical subject headings (MeSH) generated by the National Library of Medicine for MEDLINE/PubMed alone and in combination, without finding any report of pulmonary emboli associated with a diagnosis of coccidioidomycosis. Discussion with other clinicians with extensive experience diagnosing and treating coccidioidomycosis in highly endemic areas failed to yield similar cases. We queried other regional expert clinicians with the thought that they may have also treated such cases but did not report them. We encountered 3 cases of VTE in ambulatory patients who initially presented with a clinical syndrome consistent with pneumonia. Dyspnea prompted an emergency room visit, and in each case both pulmonary infiltrates and pulmonary embolism were defined at that initial visit. Two of these patients were diagnosed with pneumonia and VTE at other hospitals and were later referred for ongoing treatment. The fourth patient presented with VTE during a clinic visit 1 week after hospital discharge following treatment for coccidioidomycosis meningitis. The fifth patient, described in the case report, developed pulmonary emboli while hospitalized for pneumonia. Review of the records and images of each patient confirmed the presence of multiple emboli (Figure 2), and each was prescribed anticoagulant therapy with rivaroxaban [7].
Conclusions
One could speculate that discovery of pulmonary emboli in these cases reflects the now common practice of ordering a computerized tomography angiogram (CTA) when encountering patients with respiratory complaints, and the relative ease with which such a study can be performed and interpreted [8]. CTA has been available in our local hospitals for many years, and each of the cases reviewed were encountered only in the past year (2019). Risk factors for VTE, such as immobility, can also be seen in significant pulmonary infections, such as those caused by coccidiomycosis. Yet, with the exception of 2 patients, immobility at home or in hospital was not a feature of their illness. Three of the patients with pneumonia, though fatigued and feeling ill, remained ambulatory throughout their pre-hospital course. Another possibility might be environmental changes. The region, Ventura County, where all 5 patients were likely infected experienced major fires (155 193 hectares or 591.5 square miles burned) during the preceding 2 years, followed by rainfall that ended a 6-year drought. These environmental changes may have favored
Figures
References:
1.. Kirkland TN, Fierer J: Virulence, 2018; 9(1); 1426-35
2.. Parish JM, Blair JE, Coccidioidomycosis: Mayo Clin Proc, 2008; 83(3); 343-49
3.. Levi M, van der Poll T, Schultz M, New insights into pathways that determine the link between infection and thrombosis: Neth J Med, 2012; 70(3); 114-20
4.. Levi M, van de Poll T, Coagulation in sepsis: All bugs bite equally: Crit Care, 2004(8); 99-100
5.. Epaulard O, Foote A, Bosson JL, Chronic infection and venous thromboembolic disease: Semin Thromb Hemost, 2015(41); 644-49
6.. , Coccidioidomycosis in California provisional monthly report January–October 2019 https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/CocciinCAProvisionalMonthlyReport.pdf
7.. Dobler CC, Overdiagnosis of pulmonary embolism: Definition, causes and implications: Breathe, 2019(15); 46-53
8.. Ruggiero A, Screaton NJ, Imaging of acute and chronic thromboembolic disease: State of the art: Clin Radiol, 2017(5); 375-88
9.. Jain N, Fries BC, Antigenic and phenotypic variations in fungi: Cell Microbiol, 2009(12); 1716-23
10.. Abdel-Wahab N, Lopez-Olivo MA, Pinto-Patarroyo GP, Suarez-Almazor ME, Systematic review of case reports of antiphospholipid syndrome following infection: Lupus, 2016(25); 1520-31
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250