14 June 2021: Articles 
A Young Woman with Excessive Fat in Lower Extremities Develops Disordered Eating and Is Subsequently Diagnosed with Anorexia Nervosa, Lipedema, and Hypermobile Ehlers-Danlos Syndrome
Challenging differential diagnosis, Clinical situation which can not be reproduced for ethical reasons, Rare coexistence of disease or pathology
Thomas F. Wright1BDEF*, Karen L. Herbst2DEFDOI: 10.12659/AJCR.930840
Am J Case Rep 2021; 22:e930840
Abstract
BACKGROUND: Lipedema is a loose connective tissue disease that causes disproportionate subcutaneous fat accumulation on the extremities. As a result of the increased subcutaneous tissue accumulation, lipedema is often confused with obesity by both physicians and patients. Poor awareness and limited diagnosis of lipedema contribute to the confusion of lipedema with obesity and can lead to decreased body image acceptance. Patients with lipedema may have anorexia nervosa, an eating disorder characterized by a distortion of body image, incorrect self-identification of being overweight, restricted eating behavior, and a relentless pursuit of weight loss.
CASE REPORT: A young woman with disproportionate fat accumulation on the lower half of her body self-identified as having obesity. She developed restrictive eating behavior and became obsessed with weight loss, resulting in anorexia nervosa. Her disproportionate subcutaneous tissue persisted despite losing weight to reach a nadir BMI of 15 kg/m². After a decade-long struggle, her eating disorder resolved, and she maintained a healthy weight and BMI of 21.5 kg/m² but disproportionate fat remained in her lower body. She experienced increasing leg tenderness, pain, and easy bruising and was diagnosed with lipedema.
CONCLUSIONS: Lack of recognition of lipedema by medical professionals and the public as a weight loss-resistant disease can affect body image acceptance. Lipedema was mistaken for obesity by the young woman in this case and likely played a role in her development of an eating disorder. Eating disorders, such as anorexia nervosa, are not rare and may be more common in women with lipedema.
Keywords: anorexia nervosa, Body Fat Distribution, Lipedema, Ehlers-Danlos Syndrome, Feeding and Eating Disorders, Lower Extremity
Background
Anorexia nervosa (anorexia) is an eating disorder characterized by a significant and persistent reduction in food intake leading to extremely low body weight and BMI. A distortion of body image and intense fear of gaining weight causes a relentless pursuit of thinness and disturbed eating behavior. Many people with anorexia see themselves as overweight, even when they are starved or malnourished. These characteristics form the basis for the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) diagnostic criteria for Anorexia Nervosa (Table 1. DSM 5) [1]. Anorexia can be disabling; the reported death rate from anorexia is 0.56% per year [2]. The lifetime prevalence of anorexia is estimated at 0.9% in women [3].
Lipedema is a loose connective tissue disease characterized by disproportionate accumulation of fibrotic subcutaneous adipose tissue and extracellular fluid in the limbs of women due to microvascular inflammation [4]. Lipedema is poorly recognized, and it is often mistaken for lifestyle-induced obesity [5]. Often, women with lipedema identify as overweight or obese. Lipedema is also often confused with lymphedema, which causes asymmetric swelling of the limbs and is caused by defects in lymphatic transport [6]. The diagnosis of lipedema is based on the clinical criteria first published by Wold et al and updated most recently with International Consensus
Diagnostic Criteria [7,8] (Table 2). These criteria emphasize heavy, tender, symmetric enlargement of the limbs, sparing the hands and feet, with negative Kaposi-Stemmer’s sign. The prevalence of lipedema is not known; however, the most cited estimate of the prevalence is 11% of the female population [9]. Lipedema is classified as a diffuse painful symmetric lipomatosis and needs to be differentiated from another lipomatosis disease called Dercum’s disease, which is characterized by painful lipomas [10].
Lipedema progression is graded by stages [6,8,10]. Stage 1 lipedema is characterized by a thickening and disproportionate accumulation of loose connective tissue (LCT) in the extremities. The skin remains smooth, but there are small palpable nodules in the LCT; the tissue is generally not heavy or swollen, but there is often pain, and there is resistance to weight loss by diet or exercise. Stage 2 lipedema is characterized by increased fibrous tissue, leading to larger palpable nodules in the LCT and increased swelling and tenderness of affected areas. Stage 3 lipedema is characterized by formation of lobules of skin and LCT, and larger and more extensive masses in the tissue [11]. Increased tissue sodium and extracellular water are seen in Stage 2 and 3 lipedema [12,13]. Delayed lymphatic transport in lipedema may be present before overt clinical secondary lymphedema or lipo-lymphedema is seen [14,15]. A percentage of women in Stages 2 and 3 lipedema develop overt secondary lymphedema with pitting edema in the legs and feet, called lipo-lymphedema [16]. Lipedema is also classified by types according to the anatomic location of the disease. Type I affects the area of the buttocks and hips; Type II affects the buttocks to knees, with formations of folds of fat around the inner side of the knee; Type III affects the buttocks to ankles; Type IV affects the arms; and Type V affects the lower legs (see Figure 1) [8].
Case Report
At approximately 12 years of age, an adolescent female began developing excess subcutaneous fat on the hips, thighs, calves, and ankles out of proportion to her upper body. Her thighs, calves, and ankles were disproportionately large and increased in size as she physically matured, although she was technically underweight, with a BMI of 17 kg/m2. Her uneven body shape became a source of poor self-esteem, progressing to emotional distress. She felt ashamed of her legs, calling them her “vanilla shame,” and “wore loose fitting clothing like long dresses that would hide” her legs. During her teens, her relationship with food became progressively unhealthier. She would restrict her eating, was persistently afraid of gaining weight, and self-identified as overweight. She also would purge meals and abuse laxatives. At the age of 17, she met the DSM-5 criteria of anorexia nervosa [1]. At the height of her anorexia struggle, she was 5’10” and 50 kilograms, with a BMI of 15 kg/m2. She was prescribed antidepressant medication and participated in individual counseling. After a nearly decade-long struggle, her body image and thoughts about food and eating behavior became consistently healthy. She recovered from her anorexia and returned to a healthy weight of 68 kg, BMI 21.8 kg/m2, with the bulk of her fat tissue on the lower half of her body. Over the last 4–5 years, she noticed an increase in easy bruising and increasing heaviness, tenderness, and pain in her thighs and calves. At age 33 years, she presented to an outpatient medical office with disproportionately large, heavy, tender legs (Figure 2).
Her past medical history was significant for urinary tract infections, migraine headaches, and pneumonia. Her social history was positive for the rare consumption of alcohol. Her family history was significant for her mother and sister with disproportionately shaped and larger lower half of their bodies.
Her physical exam demonstrated a healthy weight of 68 Kg, height of 177.8 cm (5 feet 10 inches) with BMI 21.8 kg/m2. Her blood pressure was 118.0/82.0 mm Hg, with heart rate of 92 beats per minute. The patient presented an overall appearance of a healthy young woman with small waist and visible ribs with increased fat tissue on the hips, thighs, and calves. Her heart, lungs, and abdominal exam were normal. An extremity exam found 1+ non-pitting edema present in the bilateral hips, thighs, and pretibial area. Trace non-pitting edema was detected on the arms. On the dorsal aspect of her feet, her skin was able to be pinched into a tent, a negative Kaposi-Stemmer Sign. The skin was soft with pea-to-walnut sized subcutaneous nodules palpable on the thighs and hips. There was symmetrical disproportionate excess fatty tissue on the front of the thighs, overhanging the knees, and on the inner and lateral thighs. There was symmetrical disproportionate excess fatty tissue on the calves. Both ankles had subcutaneous fatty tissue cuffs. There was faint erythema on the lower legs, which blanched on palpation. There was normal hair distribution for sex. Silver striae were present on both thighs. A joint exam was consistent with generalized joint hypermobility of the fingers, wrists, elbows, and knees by the Beighton Criteria with a score of 8 out of 9 (Table 3) [17].
She was diagnosed with Stage 1, Type 3, buttocks to ankles, lipedema following the International Consensus Diagnostic Criteria (Table 1) [8]. She was also diagnosed with Ehlers-Danlos hypermobility syndrome (JHS/hEDS) [18].
Discussion
This clinical case shows how poor understanding and recognition of lipedema can play a role in the self-identification of being overweight or obese. Lipedema is often associated with higher body weights and BMI, but this case shows lipedema can be present in underweight women. Lipedema is a loose connective tissue disease characterized by growth of painful loose connective tissue on the limbs, primarily of women, that is relatively resistant to diet and exercise, as in this case [8]. As it progresses, interstitial edema, inflammation, and tissue fibrosis develop, resulting in nodularity and swelling of the subcutaneous tissue [4]. The lack of a proper diagnosis of lipedema when present can affect body acceptance and play a role in distorted body perception of eating disorders. Anorexia nervosa is a psychiatric disorder that is characterized by body dysmorphia, chronic undernourishment, and low BMI. The body weight cut-off for anorexia is 15% below expected, or BMI less than 17.5 Kg/m2 [19].
Individuals with anorexia overly restrict food intake to correct a distorted body image [19]. The disproportionate increase in fat accumulation on the legs in lipedema is relatively resistant to diet and exercise, which, paired with lack of awareness of this medical disorder, leads to increasing frustration [6,20,21]. The lipedema tissue on the young woman’s legs in this case did not respond to weight loss, which resulted in more unhealthy eating thoughts and behavior. The unhealthy behavior included food restriction, meal purging, and laxative use. In our review of PubMed index studies, there are no published case reports or case series of anorexia nervosa and lipedema. There is, however, a report by Kraus of a single-site study which showed an increased proportion of eating disorders in patients with lipedema [22]. The study consisted of 100 consecutive patients with lipedema; 74% had a history of eating disorders, 12% with periodic binge eating attacks, 8% with bulimia, and 16% with anorexia nervosa [22].
Anorexia nervosa has the highest mortality rate of any psychiatric disorder [23]. It has a prevalence of about 0.3% in young women. It is more than twice as common in teenage girls [23]. In our case, the onset was 17 years of age, which is in line with an average age of onset of 15 years. In addition, 80–90% of patients with anorexia are female [19].
Awareness of lipedema is very low among medical professionals and the general population [20]. A United Kingdom study showed 93% of patients who presented with lipedema signs and symptoms were not recognized by their physicians [20]. It is possible that awareness of lipedema could have helped the patient with body acceptance and prevented the development of anorexia. More study is needed to better understand if the disproportionate fat accumulation in lipedema or its relative resistance to diet is commonly responsible for eating disorders in patient with this disease. In this case, the young woman had Type 3 lipedema, which is lipedema from the ankles to buttocks. While up to 80% of women with lipedema have a combination lipedema of Type IV in the arms and Type II or III in the legs, this individual only had lipedema in her legs [8].
The patient was diagnosed with Ehlers-Danlos hypermobility syndrome (JHS/hEDS), which is thought to be the most common subtype of JHS/EDS, most cases of which are caused by genetic defects in collagen production. Joint hypermobility diseases are common connective tissue diseases. In one study, hypermobile joints were found in up to 60% of individuals with lipedema [10]. In support of lipedema as a connective tissue disease, the aorta was dilated during systole and diastole in women with lipedema [24] and there was a loss of elasticity in the tissue of the calf [25]. These studies suggest that increased connective tissue compliance may have a role in the development or progression of lipedema.
Anorexia has been reported in the literature to be associated with JHS/EDS [26]. It is thought that the extra-articular features such as gastrointestinal problems, temporomandibular disorders, and food intolerances contribute to developing and maintaining disturbed eating behaviors and significant weight loss in JHS/hEDS [27]. Our patient did not have somatic problems associated with disturbed eating in JHS/hEDS; therefore, her anorexia was more likely to be associated with her feelings of being overweight due to her lipedema.
Conclusions
Lipedema is a loose connective tissue disease of the limbs, primarily in women, that results in a fibrotic fat tissue that resists loss by even severely restricted calorie intake, as was seen in this case. The poor recognition of lipedema by medical professionals and the public can affect body image acceptance. The disproportionate subcutaneous adipose tissue of lipedema was confused with obesity by the young woman in this case and likely played a role in her development of an eating disorder. Eating disorders, such as anorexia nervosa, are not rare and may occur with increased frequency in women with lipedema, and also for somatic reasons in people with JHS/ hEDS. More study of the prevalence of anorexia nervosa and other eating disorders in the lipedema population is needed. Increased awareness of lipedema in the medical community can result in better education of patients, which may reduce the incidence of eating disorders in this population.
Figures
References:
1.. : DSM-5 Changes: Implications for Child Serious Emotional Disturbance [Internet] Jun, 2016, Rockville (MD), Substance Abuse and Mental Health Services Administration (US) 2016
2.. Sullivan PF, Mortality in anorexia nervosa: Am J Psychiatry, 1995; 152(7); 1073-74
3.. Hudson JI, Hiripi E, Pope HG, Kessler RC, The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication: Biol Psychiatry, 2007; 61(3); 348-58
4.. Al-Ghadban S, Cromer W, Allen M, Dilated blood and lymphatic microvessels, angiogenesis, increased macrophages, and adipocyte hypertrophy in lipedema thigh skin and fat tissue: J Obes, 2019; 2019; 8747461
5.. Herbst KL, Rare adipose disorders (RADs) masquerading as obesity: Acta Pharmacol Sin, 2012; 33(2); 155-72
6.. Buck DW, Herbst KL, Lipedema: A relatively common disease with extremely common misconceptions: Plast Reconstr Surg Glob Open, 2016; 4(9); e1043
7.. Wold LE, Hines EA, Allen EV, Lipedema of the legs; A syndrome characterized by fat legs and edema: Ann Intern Med, 1951; 34(5); 1243-50
8.. Sandhofer M, Hanke CW, Habbema L, Prevention of progression of lipedema with liposuction using tumescent local anesthesia: Results of an International Consensus Conference: Dermatol Surg, 2020; 46(2); 220-28
9.. Foldi E, Foldi M, Lipedema: Foldi’s Textbook of Lymphology, 2006; 551, M¨nchen, Germany, Elsevier, Urban & Fischer Verlag
10.. Beltran K, Herbst KL, Differentiating lipedema and Dercum’s disease: Int J Obes (Lond), 2017; 41(2); 240-45
11.. Wollina U, Lipedema – an update: Dermatol Ther, 2019; 32(2); e12805
12.. Crescenzi R, Marton A, Donahue PMC, Tissue sodium content is elevated in the skin and subcutaneous adipose tissue in women with lipedema: Obesity (Silver Spring), 2018; 26(2); 310-17
13.. Crescenzi R, Donahue PMC, Weakley S, Lipedema and Dercum’s disease: A new application of bioimpedance: Lymphat Res Biol, 2019; 17(6); 671-79
14.. Forner-Cordero I, Olivan-Sasot P, Ruiz-Llorca C, Munoz-Langa J, Lymphoscintigraphic findings in patients with lipedema: Rev Esp Med Nucl Imagen Mol, 2018; 37(6); 341-48
15.. Gould DJ, El-Sabawi B, Goel P, Uncovering lymphatic transport abnormalities in patients with primary lipedema: J Reconstr Microsurg, 2019; 23(10); 136-41
16.. Herbst K, Mirkovskaya L, Bharhagava A, Lipedema fat and signs and symptoms of illness, increase with advancing stage: Archives of Medicine, 2015; 7(4: 10); 1-8
17.. Beighton P, Horan F, Orthopaedic aspects of the Ehlers-Danlos syndrome: J Bone Joint Surg Br, 1969; 51(3); 444-53
18.. Malfait F, Francomano C, Byers P, The 2017 international classification of the Ehlers-Danlos syndromes: Am J Med Genet C Semin Med Genet, 2017; 175(1); 8-26
19.. Morris J, Twaddle S, Anorexia nervosa: BMJ, 2007; 334(7599); 894-98
20.. Fetzer A, Fetzer S: Lipoedema UK Big Survey 2014 Research Report, 2016, Chichester, Lipoedema UK http://www.lipoedema.co.uk/wp-content/uploads/2016/04/UK-Big-Surey-version-web.pdf
21.. Di Renzo L, Cinelli G, Romano L, Potential effects of a modified mediterranean diet on body composition in lipoedema: Nutrients, 2021; 13(2); 358
22.. Kraus RH, [All about lipedema]: Lymphe Gesundheit, 2015; 2015(1); 1-9 [in German]
23.. Hoek HW, Incidence, prevalence and mortality of anorexia nervosa and other eating disorders: Curr Opin Psychiatry, 2006; 19(4); 389-94
24.. Szolnoky G, Nemes A, Gavaller H, Lipedema is associated with increased aortic stiffness: Lymphology, 2012; 45(2); 71-79
25.. Jagtman BA, Kuiper JP, Brakkee AJ, [Measurements of skin elasticity in patients with lipedema of the Moncorps “rusticanus” type]: Phlebologie, 1984; 37(3); 315-19 [in French]
26.. Lee M, Strand M, Ehlers-Danlos syndrome in a young woman with anorexia nervosa and complex somatic symptoms: Int J Eat Disord, 2018; 51(3); 281-84
27.. Bulbena A, Baeza-Velasco C, Bulbena-Cabre A, Psychiatric and psychological aspects in the Ehlers-Danlos syndromes: Am J Med Genet C Semin Med Genet, 2017; 175(1); 237-45
28.. Herbst KL, Subcutaneous adipose tissue diseases: Dercum disease, lipedema, familial multiple lipomatosis, and madelung disease. [Updated 2019 Dec 14]: Endotext [Internet], 2000, South Dartmouth (MA), MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK552156/
Figures
Tables
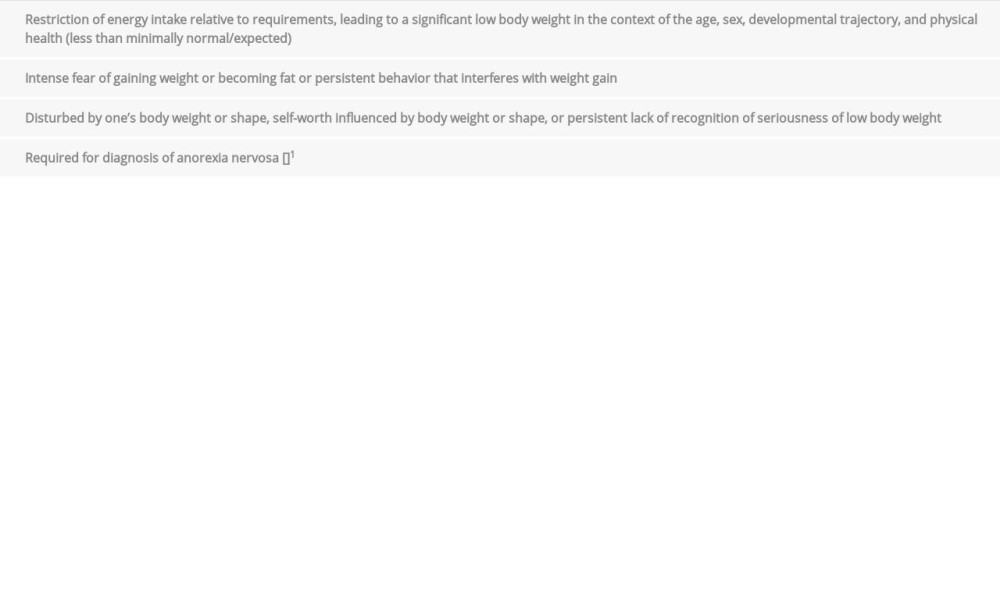 Table 1.. DSM-IV to DSM-5 anorexia nervosa.
Table 1.. DSM-IV to DSM-5 anorexia nervosa.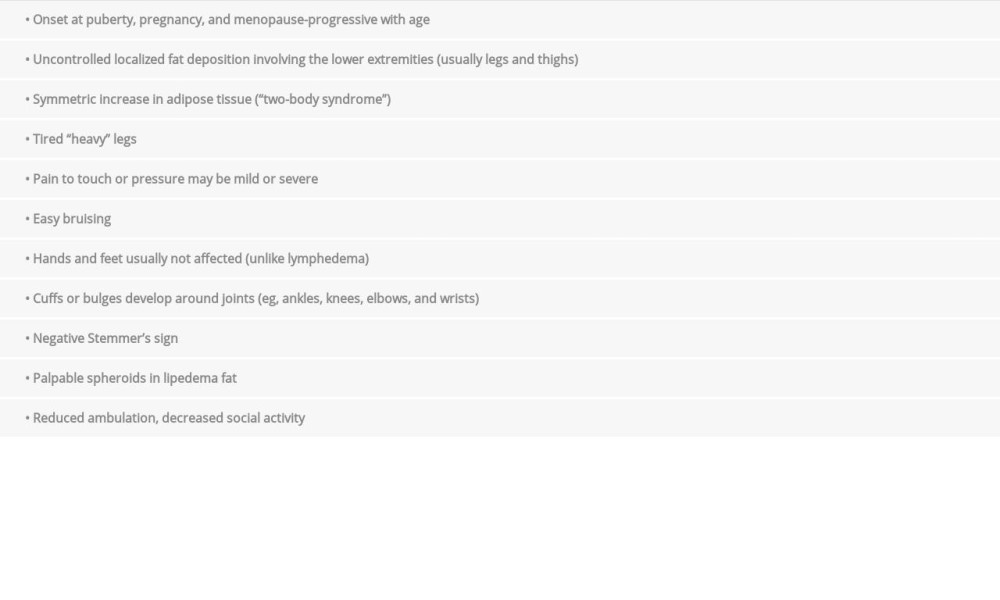 Table 2.. Diagnostic criteria of lipedema: International consensus [8].
Table 2.. Diagnostic criteria of lipedema: International consensus [8].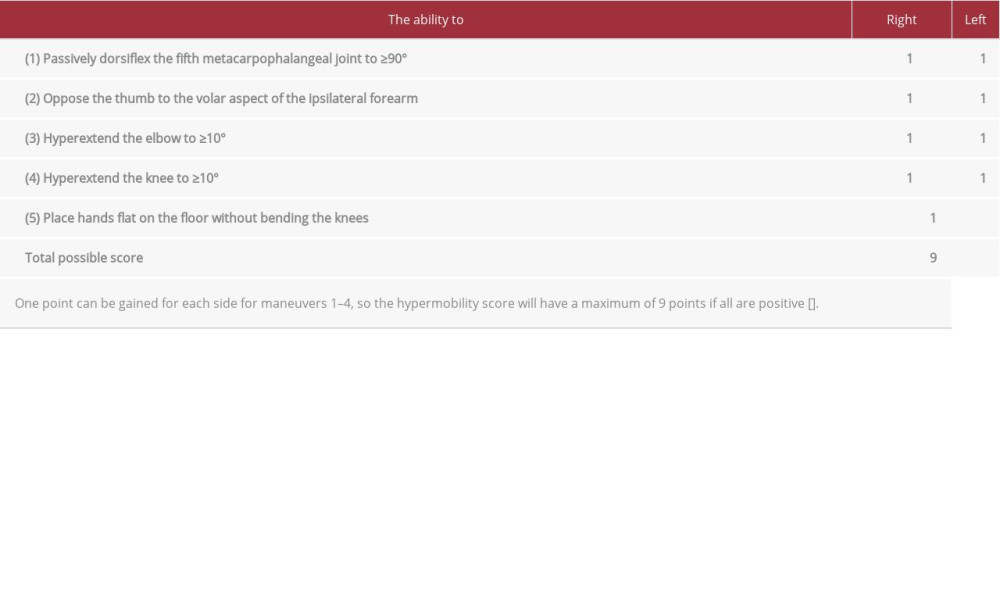 Table 3.. Beighton’s joint hypermobility score.
Table 3.. Beighton’s joint hypermobility score.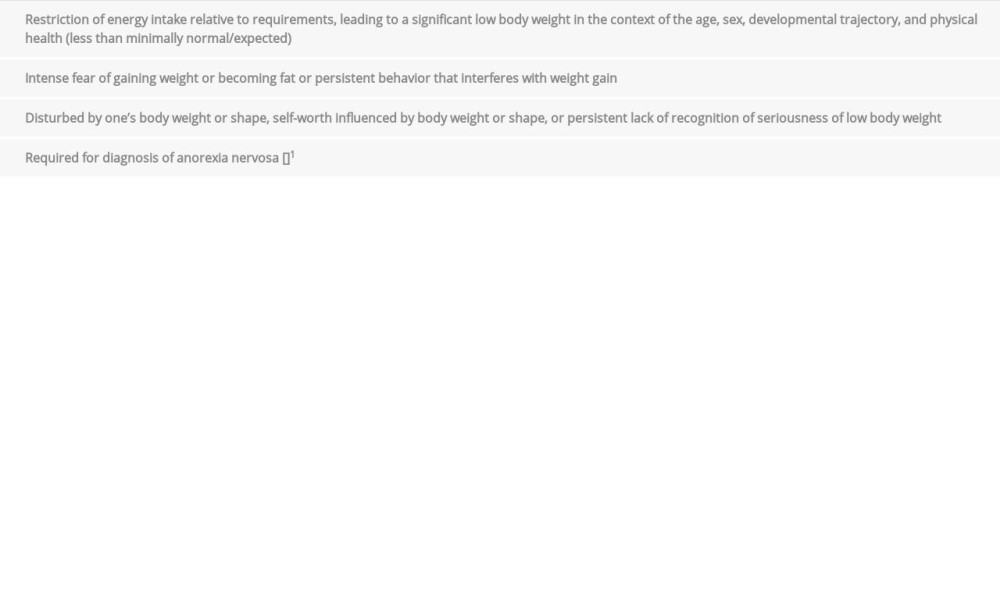 Table 1.. DSM-IV to DSM-5 anorexia nervosa.
Table 1.. DSM-IV to DSM-5 anorexia nervosa.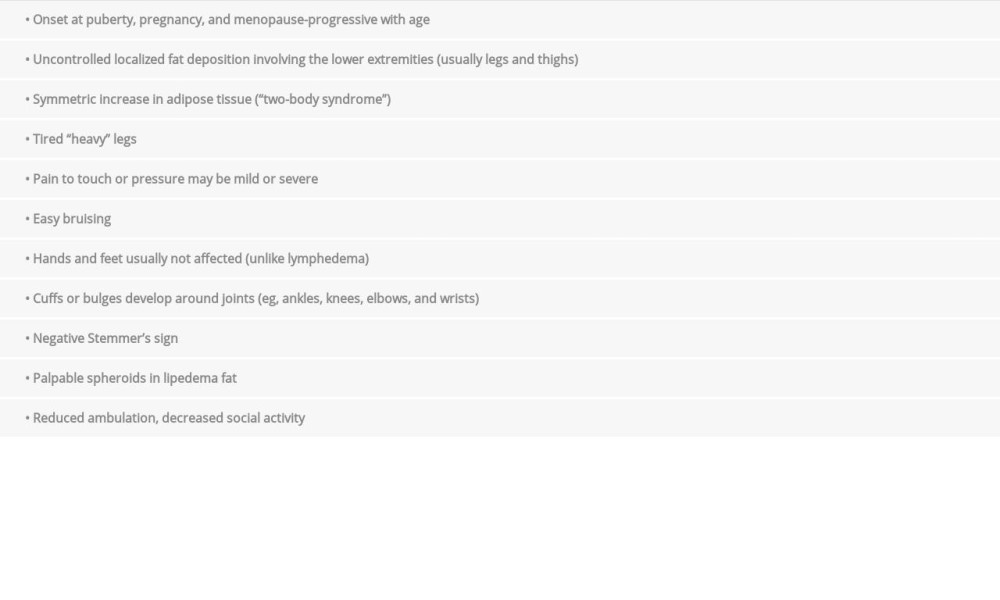 Table 2.. Diagnostic criteria of lipedema: International consensus [8].
Table 2.. Diagnostic criteria of lipedema: International consensus [8].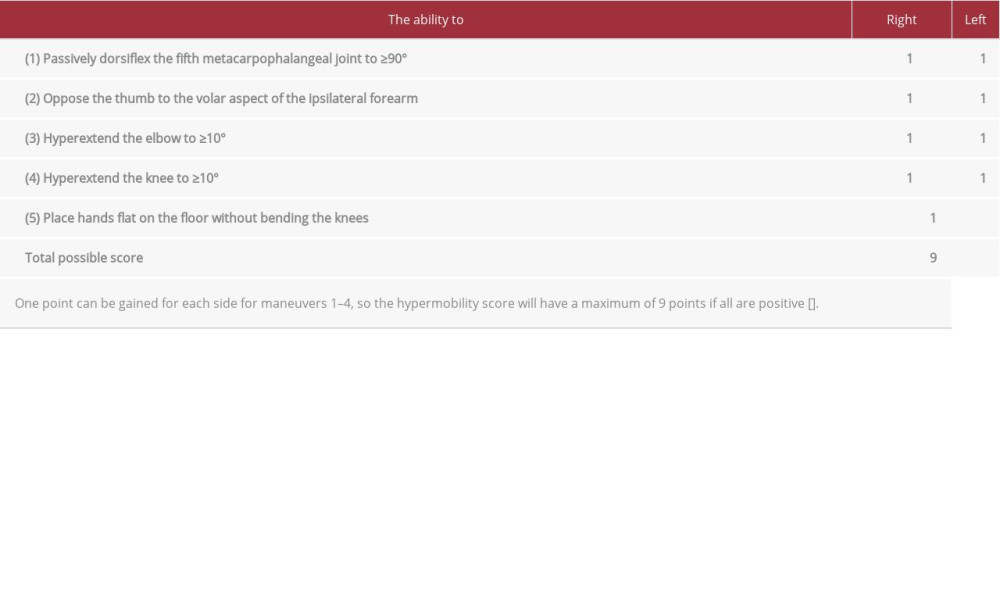 Table 3.. Beighton’s joint hypermobility score.
Table 3.. Beighton’s joint hypermobility score. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








