10 November 2021: Articles 
Prednisolone Treatment Is Effective for an Idiopathic Penile Abscess: A Case Report and Review
Rare disease
Atsushi Yamagishi1AEF*, Masayuki KurokawaDOI: 10.12659/AJCR.933618
Am J Case Rep 2021; 22:e933618
Abstract
BACKGROUND: Penile abscesses were traditionally regarded as an infectious disease; however, idiopathic cases in which prednisolone was effective have been reported.
CASE REPORT: A 64-year-old man was admitted to the hospital with symptoms of penile induration and dysuria. He was diagnosed with a penile abscess, which was punctured and then relapsed. An incision and drainage were performed on the abscess, and the pus and tissue samples were cultured and examined histologically. There was no evidence of malignancy or bacterial infection, and he was diagnosed with an idiopathic penile abscess. As pus continuously drained from the incision, prednisolone 40 mg was initiated, which resulted in a decreased amount of pus and eventual wound closure. Over 15 months, prednisolone was gradually tapered to 5 mg, and the abscess continued to decrease in size.
CONCLUSIONS: Idiopathic penile abscesses are rare but often lead to penectomy. Prednisolone is a new treatment method for such patients. This is the third case of an idiopathic penile abscess that was successfully treated with prednisolone. The causative agent of the idiopathic penile abscess was suggested to be pyoderma gangrenosum; however, this case did not exhibit the typical characteristics of pyoderma gangrenosum. Therefore, further investigation was needed. A differential diagnosis of an infectious abscess is required before initiating steroid treatment. Open drainage is useful, but the size of the incision should be minimized for the purpose of preserving penile function. The prednisolone dose should be started at 20 to 40 mg and reduced gradually to avoid relapse.
Keywords: Penile Diseases, Prednisolone, Pyoderma Gangrenosum, Abscess, Diagnosis, Differential, Drainage, Humans, Male
Background
Penile abscess is a rare disease, which has traditionally been considered as an infectious disease and usually occurs secondary to trauma or in patients with immunocompromising conditions such as diabetes [1]. However, in a report summarizing 29 cases of penile abscess, 20 of these were of idiopathic origin [2]. The disease prognosis is very poor; in particular, recurrent cases and idiopathic cases that are negative for any causative bacteria tend to undergo penectomy. In Japan, 2 cases that were successfully treated with prednisolone and avoided penectomy have been reported [2,3]. The discovery of this treatment strategy is invaluable in improving the negative outcomes of this disease and in suggesting immunologic etiology.
We report a case of an idiopathic penile abscess in which prednisolone treatment was successful and provide a review of the past cases. This report represents the third case of such a condition.
Case Report
A 64-year-old man was referred to the urology department of a general hospital for induration of the penis and dysuria which had persisted for 1 month. He had a history of renal stones and gallstones and had undergone surgery for gouty arthritis of the left ankle. The patient had a membranous urethral stricture and underwent urethral dilatation and catheter placement. The measured level of the prostate-specific antigen (PSA) was 13.4 ng/mL. Magnetic resonance imaging (MRI) of the induration revealed a penile abscess (Figure 1A). A month after the referral, the patient underwent an abscess puncture, urethral biopsy, and prostate biopsy. The pus that drained from the abscess was analyzed, and the culture results were negative for any etiologic agent. The urethral biopsy showed inflammatory changes, while the prostate biopsy detected an adenocarcinoma with a Gleason score of 3+4 in 3 of the 14 specimens. The patient was then referred to our hospital for robot-assisted radical prostatectomy.
While considering surgical options, he expressed concern of a potential recurrence of penile induration. The patient’s overall condition was favorable, and his vital signs did not show abnormalities. However, an induration of 1 to 2 cm in diameter was noted at the base of the penis and the shaft (Figure 2A). The urinalysis results were unremarkable, the urine culture was negative for any etiologic agent, and the blood tests did not show any inflammatory reaction. The MRI results confirmed a recurrence of the penile abscess (Figure 1B). The cystoscopy results suggested severe inflammatory stenosis in the membranous urethra.
Two months after the recurrence, an internal urethral incision and a penile abscess incision and drainage were performed. The incision was on the tunica albuginea, and the excreted pus was drained. Since the abscess had no capsule and destructively infiltrated the inside of the corpus cavernosum, minimal debridement was performed (Figure 2B). The pus and abscess tissue were collected prior to the initiation of antibiotics, examined, and cultured for bacteria and myco-bacteria, which turned out negative. The histological examination revealed inflammation and granulation tissue accompanied by an infiltration of inflammatory cells. The inflammatory cells mainly comprised lymphocytes, plasma cells, and macrophages; very few neutrophils were identified. No cells indicative of a malignancy were observed (Figure 3). Based on the above findings, he was diagnosed with a non-bacterial idiopathic penile abscess. The possibility of pyoderma gangrenosum being the etiologic agent in this case was also considered, based on previous reports [2,3]. However, the dermatologist could not find any indication that the condition was caused by pyoderma gangrenosum. Although the patient had a history of gouty arthritis surgery on his ankle, he did not have symptoms or autoantibodies that were indicative of rheumatic disease. Additionally, he had no gastrointestinal symptoms.
The wound was rinsed with water and covered with gentamicin ointment and gauze each day. The postoperative wound pain was tolerable without painkillers. Since there was continuous discharge of pus, prednisolone treatment was suggested. After obtaining informed consent from the patient and his family, treatment was initiated.
One month after incision and drainage, prednisolone treatment was initiated with a dose of 40 mg/day. One week after treatment initiation, the amount of pus draining was minimal, and the wound was observed to be healing. The dose of prednisolone was gradually reduced as follows: 40 mg for 2 weeks, 30 mg for 3.5 weeks, 25 mg for 4 weeks, 20 mg for 6 weeks, 15 mg for 8 weeks, and 10 mg for 10 weeks, which was further reduced to 5 mg by 1-mg increments every 8 weeks. The wound was completely healed 10 weeks after initiating prednisolone treatment (Figure 2C). Subsequently, 15 months after the start of the administration, the prednisolone dose was reduced to 5 mg, and the MRI showed sustained remission of the abscess (Figure 1C). Insomnia appeared as an adverse effect of the prednisolone in the early stage of administration, but no medication was required, and no other notable adverse effects were observed. As a postoperative complication, the right dorsolateral area of the penis, distal to the incision site, lost tumescence. That portion had restricted blood flow by the wound scar and remained flaccid even when other portion became tumescent. For the urethral stricture, a bougie was performed several times after the operation and ended without signs of restenosis, and no recurrence was observed. For the prostate cancer, active surveillance was preferred over any type of treatment until the penile abscess stabilized. The PSA level did not increase, and the cancer lesion was not clear on MRI. A follow-up analysis is still ongoing.
Discussion
Although several cases of idiopathic penile abscess have been reported, their causes were usually infection and were not further discussed. Two previous reports on prednisolone treatment for this disease suggested that the underlying etiology was pyoderma gangrenosum [2,3]. Interestingly, some cases of urethral stricture have also been reported, similar to the present case [2,4,5]. There are several case reports of pyoderma gangrenosum on the vulvar skin, but none exist regarding abscesses in the corpus cavernosum. Pyoderma gangrenosum is a disease in which chronic and progressive neutrophilic skin necrosis occurs. The cause has yet to been identified, but an immunological mechanism specifically associated with neutrophils is suspected to play a role. Pyoderma gangrenosum promotes the formation of abscesses and ulcers and is exacerbated by mechanical irritation and debridement. It is often associated with inflammatory bowel disease and rheumatoid arthritis [6].
Based on these viewpoints, a detailed examination of pyoderma gangrenosum was performed in our patient before prednisolone treatment was initiated. However, no dermatological findings of pyoderma gangrenosum were identified. Moreover, rheumatoid arthritis and inflammatory bowel disease, which are frequently seen with pyoderma gangrenosum, were also absent. The histological findings were also inconclusive because the infiltrating cells were mostly macrophages and not neutrophils. These results do not point to pyoderma gangrenosum as the diagnosis. In the first reported case, the diagnosis had been based on the fact that neutrophil infiltration was found in the dermis by skin biopsy [2]. However, the diagnosis of pyoderma gangrenosum could not be confirmed by this histological finding alone. In the second case, the non-bacterial penile abscess had been directly diagnosed as pyoderma gangrenosum based on the report of the first case, and there was no description of the findings that were typical of pyoderma gangrenosum [3]. For these reasons, we cannot conclude that an idiopathic penile abscess is caused by pyoderma gangrenosum, although we agree that diagnosis should be based on immunogenic mechanisms and it was effectively treated by prednisolone. In the future, it will be necessary to evaluate more cases and examine them in detail to identify the underlying mechanisms of the condition.
When opting for prednisolone treatment, ruling out infectious abscesses is crucial. Signs such as the absence of fever, mild local symptoms, mild inflammatory reactions, non-response to antibiotics, and negative culture tests are all considered important factors. In particular, the culture tests should be performed before the administration of antibiotics to avoid false negatives. In patients with initial symptoms of induration, penile tuberculosis should be ruled out since it often forms nodules and ulcers rather than abscesses [7]. Periurethral abscesses caused by
Open drainage is useful as it promotes the continuous drainage of pus and facilitates the observation of the therapeutic effect of prednisolone via the reduction in the amount of drainage. However, in our case, partial erectile dysfunction occurred on the right dorsolateral area of the penis and distal to the incision site. In another case, a urethral fistula had also been reported [3]. If an idiopathic penile abscess is suspected and prednisolone treatment is considered, the necessity for an invasive treatment of the penis should be minimized, and options such as a puncture or small incision are warranted to preserve penile function.
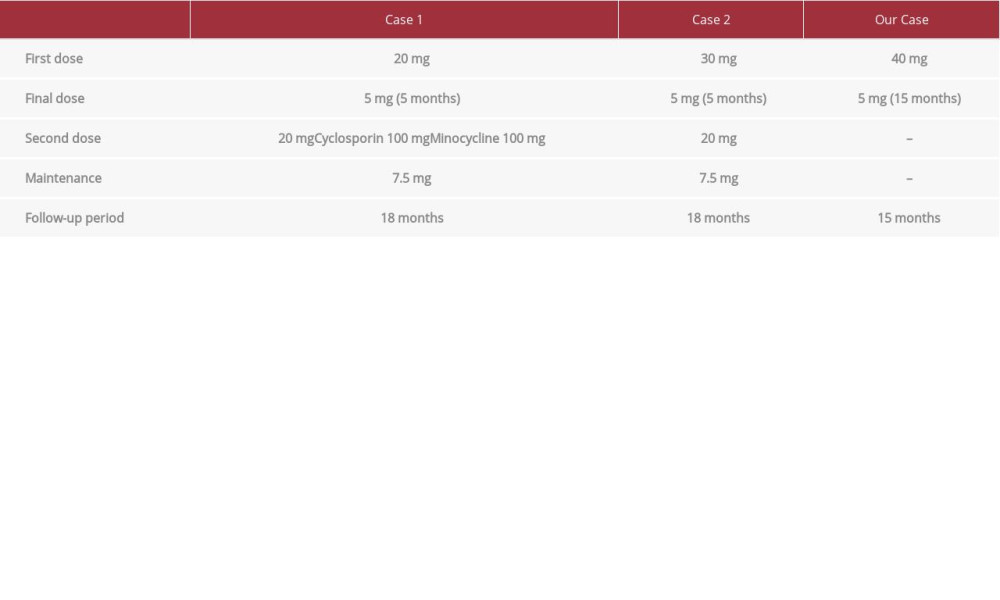
Table 1 summarizes the progress of past reports based on the prednisolone doses. In a previous report, the initial dosage was 20 to 30 mg, which was gradually tapered, but a relapse occurred. A dosage of 0.5 to 2 mg/kg of corticosteroid was most commonly used for pyoderma gangrenosum [9]. For those reasons, in our case, prednisolone treatment was initiated at 40 mg and gradually tapered to 5 mg over 15 months. No severe adverse effect and no recurrence has been observed to date. The optimal dose and duration should be verified by repeating the procedure used in these cases.
Conclusions
An idiopathic penile abscess can be treated successfully by prednisolone. When considering this treatment, other infectious diseases need to be rigorously ruled out. Open drainage is useful, but a small incision is better to preserve penile function. Further case reports and studies are needed to determine the mechanisms and optimal treatment of penile abscesses.
Figures
References:
1.. Moussa M, Abou Chakra M, Spontaneous cavernosal abscess: A case report and review of literature: J Surg Case Rep, 2019; 2019; rjz108
2.. Iida K, Mizuno K, Kawai N, [A case of abscess of corpus cavernosum as an early symptom of penile pyodermal gangrenosum: We propose the possibility of a new pathogenic finding.]: Hinyoukika Kiyo, 2015; 61; 115-19 [in Japanese]
3.. Takahashi S, Numakura K, Kubo K, [A case of penile pyoderma gangrenosum treated with steroid administration without penectomy.]: Hinyoukika Kiyo, 2019; 65; 219-22 [in Japanese]
4.. Ranjan P, Chipde SS, Prabhakaran S, Endoscopic management of emphysematous periurethral and corporal abscess: Niger Med J, 2013; 54; 209-10
5.. Koyama J, Namiki S, Kamiyama Y, [Total penectomy for corpus cavernosum abscess: A case report.]: Acta Urol Jpn, 2015; 61; 109-14 [in Japanese]
6.. Maverakis E, Ma C, Shinkai K, Diagnostic criteria of ulcerative pyoderma gangrenosum a Delphi consensus of international experts: JAMA Dermatol, 2018; 154; 461-66
7.. Singal A, Pandhi D, Kataria V, Arora VK, Tuberculosis of the glans penis: An important differential diagnosis of genital ulcer disease: Int J STD AIDS, 2017; 28; 1453-55
8.. Kenfak-Foguena A, Zarkik Y, Wisard M, Periurethral abscess complicating gonococcal urethritis: Case report and literature review: Infection, 2010; 38; 497-500
9.. Quist SR, Kraas L, Treatment options for pyoderma gangrenosum: J Dtsch Dermatol Ges, 2017; 15; 34-40
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250