08 February 2022: Articles 
Case Report: Infective Endocarditis of Mechanical Aortic Valve Due to Bacteremia
Unknown etiology, Unusual setting of medical care, Rare disease
Tatiana J. GetmanDOI: 10.12659/AJCR.933750
Am J Case Rep 2022; 23:e933750
Abstract
BACKGROUND: Neisseria elongata is a infrequent cause of infective endocarditis (IE). Although considered a commensal bacterium of the human nasopharynx, N. elongata has been shown to be the cause of significant disease in humans, namely endocarditis, osteomyelitis, and septicemia.
CASE REPORT: We report the case of a 53-year-old man with a past medical history of mechanical aortic valve who presented to the hospital for evaluation of eleven days of recurrent and relapsing fevers and was admitted for severe sepsis with concern for endocarditis. Blood cultures revealed N. elongata bacteremia, and an echocardiogram did not show any vegetations, although it was limited by mechanical aortic valve shadowing. The patient recovered after six weeks of treatment with intravenous ceftriaxone and oral ciprofloxacin.
CONCLUSIONS: Clinicians should be aware of the possibility of the previously considered non-pathogenic N. elongata as a source of IE caused by gram-negative organisms, as it can potentially cause severe disease and multiple complications. Our case additionally highlights that IE has highly variable clinical presentations. Thus, it is essential to utilize the Duke criteria as only a clinical guide for the diagnosis of IE rather than a substitute for clinical judgment and the decision to treat a patient with suspected IE.
Keywords: infective endocarditis, Bacteremia, Neisseria elongata, Sepsis/Septicemia, Mechanical Heart Valve, Aortic Valve, Endocarditis, Endocarditis, Bacterial, Humans, Male
Background
A literature review revealed only a few reported cases of infective endocarditis due to
Case Report
A 53-year-old man presented to the Emergency Department for eleven days of recurrent, relapsing fevers with night sweats and generalized weakness. His past medical history was significant for an aortic aneurysm, which required repair, and a mechanical aortic valve. Additional pertinent history was obtained and was negative for recent surgeries, recent travel, previous intravenous (i.v.) drug use, and recent dental infection or treatment.
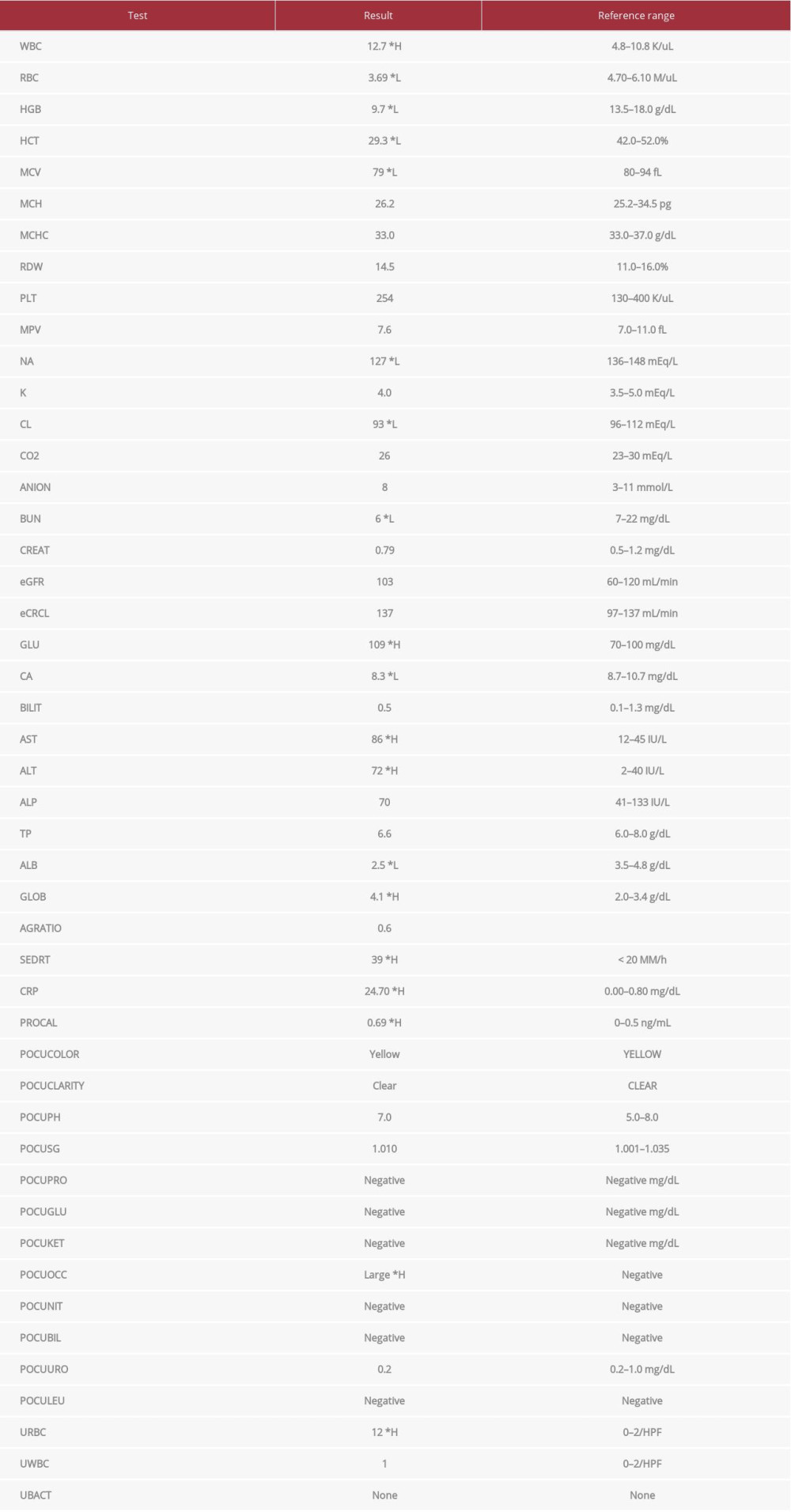
On physical examination, the patient had a temperature of 38.3°C, a heart rate of 105 beats/min, blood pressure of 116/72 mmHg, and a respiratory rate of 22 breaths/min. On cardiovascular examination, a 3/6 blowing systolic murmur with a click was heard best at the right and left upper sternal border. There was no evidence of cardiac failure, and there were no peripheral stigmata of IE. His respiratory, abdominal, musculo-skeletal, and neurologic examinations were normal. Urinalysis revealed large amounts of blood but was otherwise negative. Laboratory tests showed (Table 1) an elevated white blood cell count (12.7×109; reference range 4.8–10.8×109 K/uL), elevated erythrocyte sedimentation rate (ESR) (39; reference range <20 MM/h), elevated C-reactive protein (CRP) (24.7; reference range 0.00–0.80 mg/dL), and elevated procalcitonin (0.69; reference range 0–0.5 ng/mL). He additionally was found to have low hemoglobin of 9.7 g/dL. A chest X-ray performed at that time was unremarkable. A transthoracic echocardiogram (TTE) showed an ejection fraction of 60% to 65% and mild left ventricular hypertrophy with grade II diastolic dysfunction but no obvious severe valvular abnormalities.
The patient was admitted for severe sepsis with concern for possible endocarditis of his mechanical aortic valve. Two blood cultures were drawn on admission, and empiric antibiotic therapy was started with intravenous vancomycin and cefepime. Both blood cultures from admission returned two days later growing gram-negative rods. The results were discussed with the hospital’s laboratory staff, revealing the organism was likely
The patient quickly improved, remaining afebrile throughout his hospital course on antibiotics. Repeat blood cultures from hospital day three onward were negative. Once final identification of the gram-negative rod bacteremia and its sensitivities returned on hospital day seven to confirm
To date, three and a half months after the completion of antibiotics, the patient remains afebrile and is doing well clinically, with no evidence of infection recurrence. A detailed dental examination performed outpatient was negative, as was a CT scan of the neck.
Discussion
The primary risk factors for
Delay in diagnosis is common and likely due to the absence of murmur at presentation or difficulty identifying the organism [6]. Non-specific symptoms of IE, as mentioned above, should raise suspicion for IE. Additionally, fever in the context of a new murmur is considered IE until proven otherwise. Work-up should begin with obtaining a detailed history to identify possible predisposing conditions discussed above, performing a comprehensive physical examination to assess the patient’s vital signs and overall toxicity, and identifying any new cardiac murmurs and vascular or immunological phenomena. Frequent cardiac examinations should be performed throughout the hospital stay to evaluate for a changing murmur or signs of congestive heart failure. Basic laboratory tests and imaging studies should be obtained, including a complete blood count with differential, comprehensive metabolic panel, ESR, CRP, lactate, electrocardiogram (EKG), and chest X-ray.
Most importantly, it is imperative on admission to obtain three sets of blood cultures from different sites, ideally spaced more than one hour apart, before the initiation of antibiotics. After appropriate antibiotics have been initiated, at least two blood cultures should be obtained daily until negative to document clearance. A TTE should also be performed on all patients upon admission to identify possible vegetations. If TTE is non-diagnostic, TTE is negative, but clinical suspicion remains high, the patient is high-risk, or a progressive or invasive infection is suspected, a TEE should be obtained. Definitive diagnosis is made according to the modified Duke criteria (Table 2), which is highly sensitive for IE disease detection [8]. Both major, 1 major, and 3 minor, or all 5 minor criteria are necessary for a definite diagnosis.
Treatment involves extended antibiotics, usually of 4 to 6 weeks’ duration, and early surgical evaluation. Studies have shown that
Classifying our patient with IE revealed that extending the modified Duke criteria to the clinical practice can be difficult. Our patient technically met the Duke criteria for possible and rejected IE. He met possible IE by fulfilling at least 3 minor criteria: predisposing heart condition (mechanical valve replacement), fever, microbiological evidence not meeting significant criteria (positive blood cultures for
Conclusions
Clinicians should be aware of the possibility of the previously considered non-pathogenic
References:
1.. Grant PE, Brenner DJ, Steigerwalt AG: J Clin Microbiol, 1990; 28(12); 2591-96
2.. Wong JD, Janda JM: J Clin Microbiol, 1992; 30(3); 719-20
3.. Yoo YP, Kang K-W, Yoon HS: Tex Heart Inst J, 2014; 41(2); 227-30
4.. Andersen BM, Weyant RS, Steigerwalt AG: J Clin Microbiol, 1995; 33; 76-78
5.. Samannodi M, Vakkalanka S, Zhao A, Hocko M: BMJ Case Rep, 2016; 2016; bcr2015213311
6.. Hofstad T, Hope O, Falsen E: Scand J Infect Dis, 1998; 30(2); 200-1
7.. Haddow LJ, Mulgrew C, Ansari A: Clin Microbiol Infect, 2003; 9(5); 426-30
8.. Habib G, Lancellotti P, Antunes MJ, 2015 ESC Guidelines for the management of infective endocarditis: Eur Heart J, 2015; 36(44); 3075-128
9.. Jenkins JM, Fife A, Baghai M, Dworakowski R: BMJ Case Rep, 2015; 2015; bcr2015212415
10.. Herbert DA: Ann Pharmacother, 2014; 48(11); 1529-30
11.. Li JS, Sexton DJ, Mick N, Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis: Clin Infect Dis, 2000; 30(4); 633-38
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250









![Definition of infective endocarditis according to the modified Duke criteria (adapted from Habib et al [8]).](https://jours.isi-science.com/imageXml.php?i=t2-amjcaserep-23-e933750.jpg&idArt=933750&w=1000)