16 February 2022: Articles 
A 48-Year-Old Man Presenting as an Emergency with Severe Back Pain, a Large Anterior Paravertebral Hematoma, and Spontaneous Rupture of the Right 9 Intercostal Artery Successfully Managed by Transcatheter Arterial Embolization: A Case Report
Challenging differential diagnosis, Management of emergency care, Rare disease
Shintaro Izumoto1ABDEF*, Tomohiro Abe1ACDEF, Takatoshi Koroki1BCEF, Eiji Furukoji2ACD, Rie Masuda2ACD, Hidenobu Ochiai1ACEFDOI: 10.12659/AJCR.934173
Am J Case Rep 2022; 23:e934173
Abstract
BACKGROUND: The rupture of an intercostal artery is rare and is usually associated with trauma, neurofibromatosis type 1, or coarctation of the aorta. Transcatheter arterial embolization is a minimally invasive vascular surgical procedure used to control hemorrhage of an intercostal artery. This report describes a case of a 48-year-old man who presented with severe back pain. This was due to a large anterior paravertebral hematoma following the spontaneous rupture of the right 9th intercostal artery. The rupture was successfully managed by transcatheter arterial embolization.
CASE REPORT: A 48-year-old man suddenly felt severe back pain while walking. He had no previous medical history and he had not experienced any external injury. On arrival, he was tachycardic and hypertensive. He did not have abnormal physical findings. His chest radiograph, 12-lead electrocardiogram, ultrasonography, and blood test findings were unremarkable. A chest computed tomography scan with contrast media was performed, which revealed a 4.3×2.7×7.0 cm mass, enhanced with contrast media, anterior to the 9th vertebral body. The patient was diagnosed with spontaneous rupture of the right ninth intercostal artery. The lesion was embolized with 8 microcoils. The patient was discharged on the 8th hospital day without complications.
CONCLUSIONS: This report presents a rare case of the rupture of an intercostal artery in which no cause was identified. It highlights the role of imaging as an important diagnostic tool. Furthermore, this report shows the benefits of the timely use of emergency transcatheter arterial embolization, which in this instance resulted in a successful outcome.
Keywords: Catheterization, Peripheral, Embolization, Therapeutic, Rupture, Spontaneous, Arteries, Back Pain, Hematoma, Humans, Male, Vascular Surgical Procedures
Background
Spontaneous intercostal arterial rupture is a rare disease that can induce hemorrhagic shock and respiratory failure, caused by a massive hemothorax or retroperitoneal hematoma [1,2].
Intercostal artery rupture is often caused by several external stimuli, such as trauma [3], surgery [4], and severe cough [5]. Spontaneous intercostal arterial rupture was reported to be associated with some underlying conditions (eg, neurofibromatosis [6], Ehlers-Danlos syndrome [7], and tumor [8]), oral antithrombotic medications [9], or aneurysms [1,2].
To the best of our knowledge, only 8 cases of a spontaneous intercostal arterial rupture occurring without any external stimuli or underlying condition have been reported [10–17]. The symptom onset for all patients was pain, and half of the patients later went into shock. This indicates the importance of immediate diagnosis and treatment. The diagnosis of an intercostal artery rupture is usually based on findings of hemothorax and upper mediastinal abnormalities, caused by hemorrhage and blood accumulation. This is confirmed by chest X-ray imaging (CXR) and ultrasound (US) examinations [11,15,17]. The identification of a rupture is missed when these tests exhibit nonspecific findings. Consequently, more severe outcomes may develop [1].
Treatments for intercostal artery rupture include surgical treatments, such as a transcatheter arterial embolization (TAE). These treatments carry a risk of ischemia of the Adamkiewicz artery, which branches from the intercostal artery or lumber artery [18]. The Adamkiewicz artery is the most important feeding artery to the spinal cord, and its ischemia results in paraplegia, sensory impairment, and bladder or rectal disorders [8,18].
This report describes the case of a man in his 40s who presented as an emergency with severe back pain due to a large anterior paravertebral hematoma, following the spontaneous rupture of the right 9th intercostal artery. The patient was successfully managed by TAE.
Case Report
A 48-year-old man suddenly felt severe back pain while walking. He had no obvious past medical history such as hypertension, was taking no medications, and had no recent history of trauma. His family’s medical history was also unremarkable. He called an ambulance because his back pain persisted, and he was transported to our hospital.
On arrival, he was tachycardic with a heart rate of 108 beats/minute and hypertensive at 147/106 mmHg. No respiratory failure was observed. Physical examination revealed no abnormal breath or heart sounds. The patient had no peripheral coldness or dampness, and the rest of his physical findings were unremarkable. A blood test showed no anemia or coagulopathy (hemoglobin 13.2 g/dL, PT-INR 1.03, APTT 25.8 s). The D-dimer levels were normal at 0.41 μg/mL (Table 1). His CXR, 12-lead electrocardiogram, US examination, and blood tests were normal and did not suggest acute coronary syndrome, aortic dissection, or pulmonary embolism. However, the symptoms persisted, so a chest CT scan was performed. Non-enhanced CT showed thickening of the space between the aorta and 9th vertebral body. Contrast-enhanced CT showed a 4.3×2.7×7.0-cm mass enhanced with a contrast media (Figure 1). No other underlying diseases associated with pseudoaneurysm, such as neurofibromatosis and Ehlers-Danlos syndrome, were detected by the enhanced CT.
The patient was diagnosed with spontaneous rupture of an intercostal artery. Transcatheter angiography was performed because of prolonged bleeding. A right femoral artery puncture was performed using a 5-Fr sheath (Medikit, Tokyo, Japan), 5-Fr shepherd hook-type catheter (Hanako Medical, Saitama, Japan), and a 0.035-inch×150-cm guidewire (SURF®, PIOLAX MEDICAL DEVICES, Kanagawa, Japan) for angiography of the
intercostal artery. Angiography revealed a leak of contrast medium in the right 9th intercostal artery (Figure 2). No apparent pseudoaneurysm was found. The Adamkiewicz artery was not visualized. The balloon occlusion test was performed at the proximal site with a 2.7/2.8-Fr×130-cm balloon catheter (Attendant Nexus®, Terumo Corporation, Tokyo, Japan) and 0.016-inch×180-cm guidewire (Fathom-16, Boston Scientific, Marlborough, MT, USA) to avoid accidental embolization of the Adamkiewicz artery, which showed no paralysis or sensory disturbances on the patient’s lower limbs.
We therefore decided to embolize the lesion. Isolation embolization was performed on the right 9th intercostal artery from the distal to proximal site with pushable coils through the deflated balloon catheter which was used in the balloon occlusion test. Because the injury site was long, 8 microcoils were used until the extravasation was stopped (two 2-mm×2-cm Microcoilspiral® [Cook Medical Japan, Tokyo, Japan], three 2-mm×3-mm, and two 2-mm×4-mm VortXTM Diamond Shape Fibered Platinum Coils® [Boston scientific Corporation, Marlborough, MA, USA], and one 0.014-inch×15-mm C-STOPPER COIL® [PIOLAX MEDICAL DEVICES, Kanagawa, Japan]). After embolization, there was no evidence of spinal cord infarction such as lower-limb paralysis and bladder or rectal disorders. During and after the embolization, the patient’s blood pressure remained stable. His systolic blood pressure stayed within the range of 120–130 mmHg and he never went into shock. During hospitalization, he had no findings suggestive of re-rupture, coagulopathy, or anemia. He was discharged on the 8th hospital day because he was in good general condition. Contrast-enhanced CT examination on the 37th day showed that the hematoma had almost disappeared, with no evidence of a neoplastic lesion (Figure 3).
Discussion
We report the case of a spontaneous rupture of the intercostal artery in a patient without any underlying diseases. In this case, the patient did not show any findings of hemothorax on CXR or US examination, whereas a contrast-enhanced CT scan revealed a hematoma in front of the 9th vertebrae. Finally, we successfully treated him using TAE without any complications.
In the present case, the patient was diagnosed with idiopathic intercostal rupture. He had no underlying illness, oral medication, or prior history of external forces such as trauma or chest surgery. Furthermore, there were no conclusive findings from physical and angiographical examinations suggestive of pre-existing diseases such as neurofibromatosis, Ehlers-Danlos syndrome, systemic lupus erythematosus, or aneurysms [2,6,19,20].
We searched for similar previous cases in PubMed using the terms ‘intercostal artery rupture’, ‘spontaneous rupture of intercostal artery’, and ‘intercostal artery pseudoaneurysm’, and manually picked the cases without any underlying diseases or any triggering stimuli, resulting in only 8 cases (Table 2) [10–17]. The patients were middle-aged (median: 52.5 years), 6 were male, and symptom onsets were sudden pain for all patients. As is the present case, a middle-aged person reporting sudden-onset pain, typically male, should be suspected to have a spontaneous intercostal artery rupture, even if they have no risk factors for vascular vulnerability or a history of trauma injuries.
A contrast-enhanced CT scan was critical to the early diagnosis in our case. In the emergency department, excluding pulmonary embolism and acute aortic dissection for patients complaining of acute chest or back pain is necessary. The D-dimer value and Aortic Dissection Detection Risk score were useful for excluding pulmonary embolism and acute aortic dissection [21]. In our case, these tools indicated the low likelihood of pulmonary embolism or acute aortic dissection, suggesting that additional CT examinations were unnecessary. As in the present case, bleeding at the posterior mediastinum would not be recognized by CXR, AXR, or US examinations [14,16]. If the CT scan had not been performed, the spontaneous rupture of the intercostal artery would not have been diagnosed. It may result in massive hemothorax or circulatory insufficiency because a Moreira non-enhanced CT scan showed a small hemothorax in this case. From the previous cases summarized in Table 2, the bleeding site was the thorax and/or abdominal wall in 5 out of 8 cases, and most of these cases went into shock [11–14,17]. Therefore, in patients with sudden-onset and persistent back pain, performing a non-enhanced CT scan should be considered, even when the likelihood of a pulmonary embolism and acute aortic dissection is low and the CXR, AXR, or US findings are unremarkable.
Our patient underwent TAE and had good outcomes in terms of length of stay, complications, and rehabilitation. Table 2 shows that 1 case received surgical treatment, 5 cases received TAE for hemostasis, and 2 cases received conservative management. TAE reportedly had an equal or better survival rate than surgical treatment and is the preferred first-line treatment, especially in cases with stable hemodynamics [22]. This is because it is minimally invasive and can be performed immediately [1,2]. Therefore, TAE is widely used for traumatized patients [23]. TAE would also be effective as a treatment for spontaneous intercostal artery rupture.
The complications of TAE include lower-limb paralysis, sensory impairment, vascular injury due to the catheter procedure itself, impaired blood flow in peripheral tissues, pulmonary embolization, and cerebral infarction. Similar complications of TAE for the spontaneous rupture of the intercostal artery are possible. When the embolic site is on the central side of the intercostal artery, spinal infarction due to embolization to the Adamkiewicz artery should be avoided. The Adamkiewicz artery usually branches from the left intercostal artery or lumbar artery to approximately 70% at the level of Th 8-L1 [24]. Table 2 reveals that spontaneous intercostal artery ruptures occurred equally on right and left sides. Although the present case had right-sided intercostal artery rupture and the angiography did not show the Adamkiewicz artery, we performed the balloon occlusion test before embolization to avoid accidental ischemia of the Adamkiewicz artery. This test would make embolization to the intercostal artery safer.
Surgical treatment is considered when hemostasis is difficult to achieve with TAE, when hemothorax causes circulatory or respiratory failure [13], or when hematoma infection is suspected [3]. Only a few cases, in which the patients were hemodynamically stable, were treated conservatively [14,15,25]. Conservative management should be selected for hemodynamically stable patients whose ruptured artery is related to the Adamkiewicz artery. Treatments therefore should be selected according to the patient’s hemodynamic status and relationship with the Adamkiewicz artery.
We could not exclude the possibility that this case had some underlying disease, because we did not perform genetic tests. Additionally, we might have missed previous similar reports not summarized in Table 2. Because a spontaneous intercostal artery rupture is very rare, further case accumulation is needed.
Conclusions
We report a case of spontaneous rupture of the intercostal artery in a patient without any underlying diseases or triggers. We achieved early diagnosis with a contrast-enhanced CT and successfully treated him by TAE. Spontaneous rupture of the intercostal artery is rare but can be fatal. However, early detection with CT scanning and timely TAE can result in successful outcomes.
Figures
References:
1.. Dominguez J, Sancho C, Escalante E, Percutaneous treatment of a ruptured intercostal aneurysm presenting as massive hemothorax in a patient with type I neurofibromatosis: J Thorac Cardiovasc Surg, 2002; 124; 1230-32
2.. Jang J, Lim Y, Woo J, Jang J, Spontaneous rupture of intercostal artery after severe cough: Am J Emerg Med, 2015; 33; 131.e1-e3
3.. Sekino S, Takagi H, Kubota H, Intercostal artery pseudoaneurysm due to stab wound: J Vasc Surg, 2005; 42; 352-56
4.. Bluebond-Langner R, Pinto P, Recurrent bleeding from intercostal arterial pseudoaneurysm after retroperitoneal laparoscopic radical nephrectomy: Urology, 2002; 60; 1111
5.. Yu W, Wang C, Ng K, Chen W, Tzeng I, Successful embolization of a ruptured intercostal artery after violent coughing: Am J Emerg Med, 2006; 24; 247-49
6.. Misao T, Yoshikawa T, Aoe M, Recurrent rupture of intercostal artery aneurysms in neurofibromatosis type 1: Gen Thorac Cardiovasc Surg, 2012; 60; 179-82
7.. Beighton P, De Paepe A, Steinmann B, Ehlers-Danlos syndromes: Revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK): Am J Med Genet, 1998; 77(1); 31-37
8.. Finstein J, Chin K, Alvandi F, Lackman R, Case report: Postembolization paralysis in a man with a thoracolumbar giant cell tumor: Clin Orthop Relat Re, 2006; 453; 335-40
9.. Salmi R, Gaudenzi P, Ricci F, Sudden acute thoracic pain and hypovolemic shock as a presentation of spontaneous rupture of intercostal artery: A case report: J Am Geriatr Soc, 2012; 60; 371-73
10.. Moon J, Lee S, Chun B, Spontaneous intercostal artery bleeding: Emerg Med J, 2008; 25; 53-54
11.. Mathew R, Abdullah S, Renfrew I, Massive abdominal wall haematoma and haemothorax due to spontaneous rupture of an intercostal artery: Emerg Med J, 2008; 25; 608
12.. Dobrilovic N, Sadiq I, Vognar L, Fingleton J, Magnetic resonance angiography demonstrating active spontaneous intercostal bleeding: J Emerg Med, 2013; 44; 171-72
13.. Dua A, Dua A, Jechow S, Idiopathic spontaneous rupture of an inter-costal artery: WMJ, 2014; 113; 116-18
14.. Ishida A, Hiraoka A, Chikazawa G, Spontaneous intercostals arterial rupture restrained by conservative management: Ann Vasc Dis, 2014; 7; 430-32
15.. Jang J, Lim Y, Woo J, Jang J, Spontaneous rupture of intercostal artery after severe cough: Am J Emerg Med, 2015; 33; 131.e1-3
16.. Junck E, Utarnachitt R, Ruptured intercostal artery pseudoaneurysm: A rare cause of acute back pain: BMJ Case Rep, 2015; 2015; bcr2015209788
17.. Tanaka Y, Haratake N, Kinoshita F, Spontaneous hemopneumothorax with a ruptured aneurysm in the second intercostal artery: Report of a case: Gen Thorac Cardiovasc Surg, 2021; 69; 1133-36
18.. Alleyne C, Cawley C, Shengelaia G, Barrow D, Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery: J Neurosurg, 1998; 89; 791-95
19.. Lu C, Chen C, Yeh S, A spontaneous intercostal artery hemorrhage in systemic lupus erythematosus: Rheumatol Int, 2012; 32; 829-31
20.. Afonso C, Pereira J, Gil-Agostinho A, Casimiro C, Spontaneous rupture of an intercostal artery: BMJ Case Rep, 2020; 13; e233242
21.. Nazerian P, Mueller C, De Matos Soeiro A, Diagnostic accuracy of the aortic dissection detection risk score plus D-dimer for acute aortic syndromes the ADvISED prospective multicenter study: Circulation, 2018; 137; 250-58
22.. Degbelo F, Cito G, Guendil B, A case report and review of the literature: Am J Case Rep, 2019; 20; 674-78
23.. Bauer J, Ray C, Transcatheter arterial embolization in the trauma patient: A review: Semin Intervent Radiol, 2004; 21; 11-22
24.. Koshino T, Murakami G, Morishita K, Does the Adamkiewicz artery originate from the larger segmental arteries?: J Thorac Cardiovasc Surg, 1999; 117; 898-905
25.. Miura T, Kawano Y, Chujo M, Spontaneous hemothorax in patients with von Recklinghausen’s disease: Jpn J Thorac Cardiovasc Surg, 2005; 53; 649-52
Figures
Tables
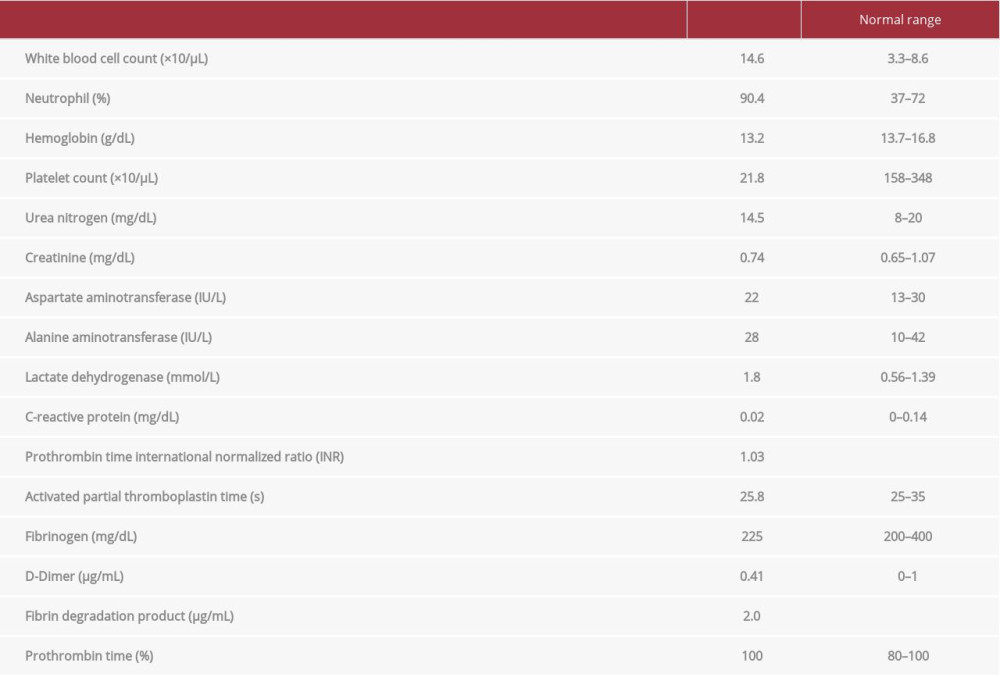 Table 1.. Laboratory findings on admission.
Table 1.. Laboratory findings on admission.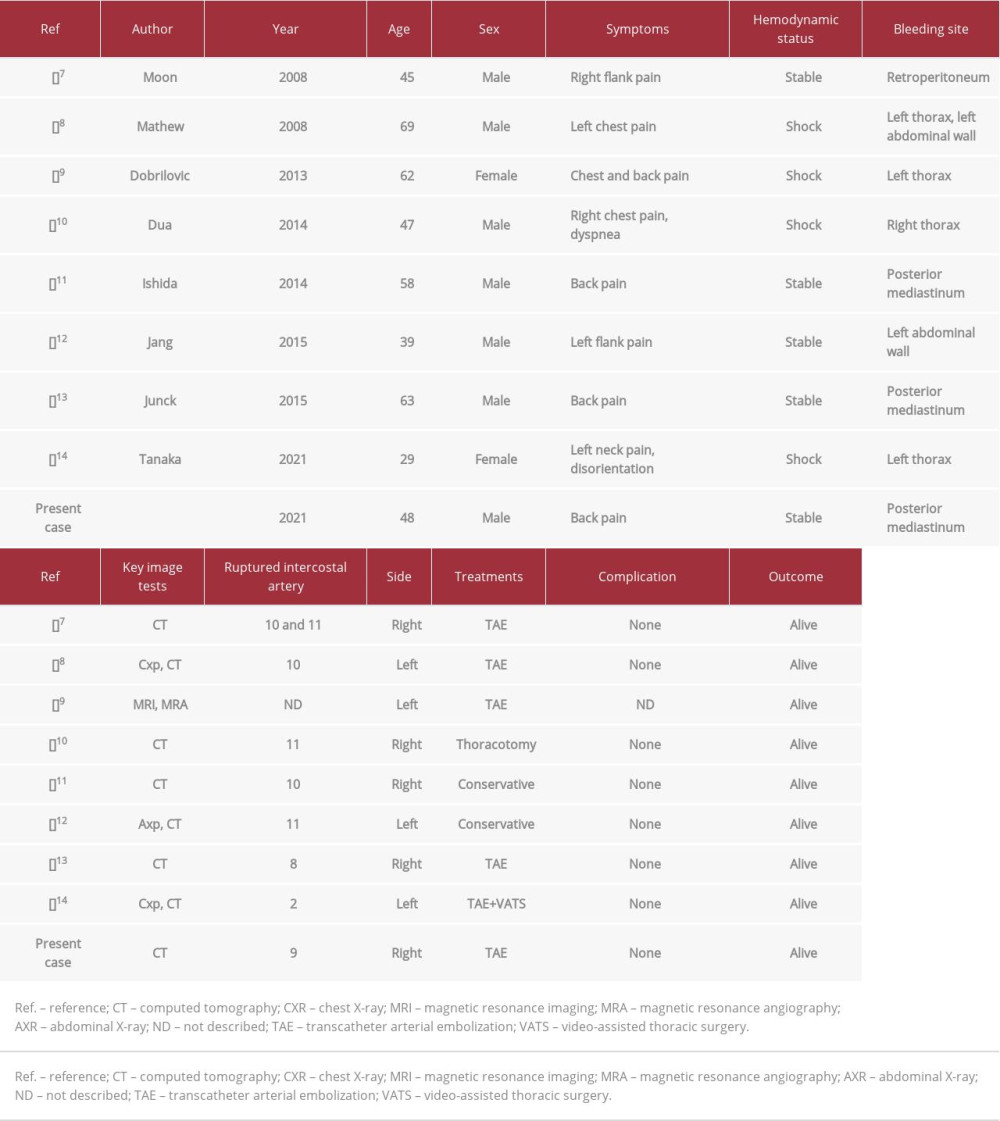 Table 2.. Summary of previous cases and the present case with spontaneous intercostal artery rupture without known underlying disease.
Table 2.. Summary of previous cases and the present case with spontaneous intercostal artery rupture without known underlying disease.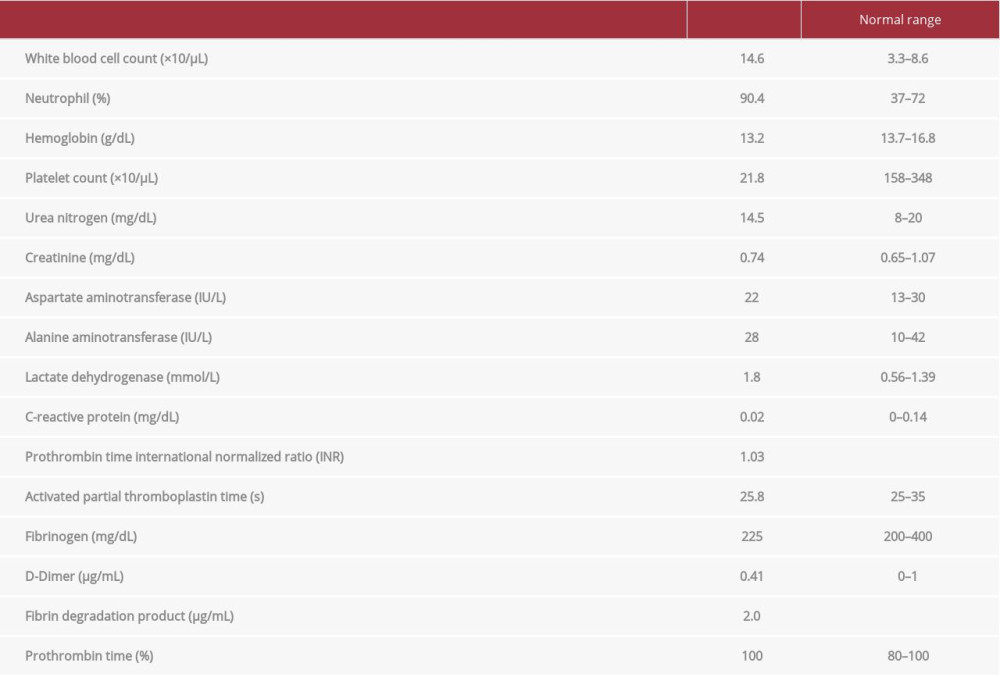 Table 1.. Laboratory findings on admission.
Table 1.. Laboratory findings on admission.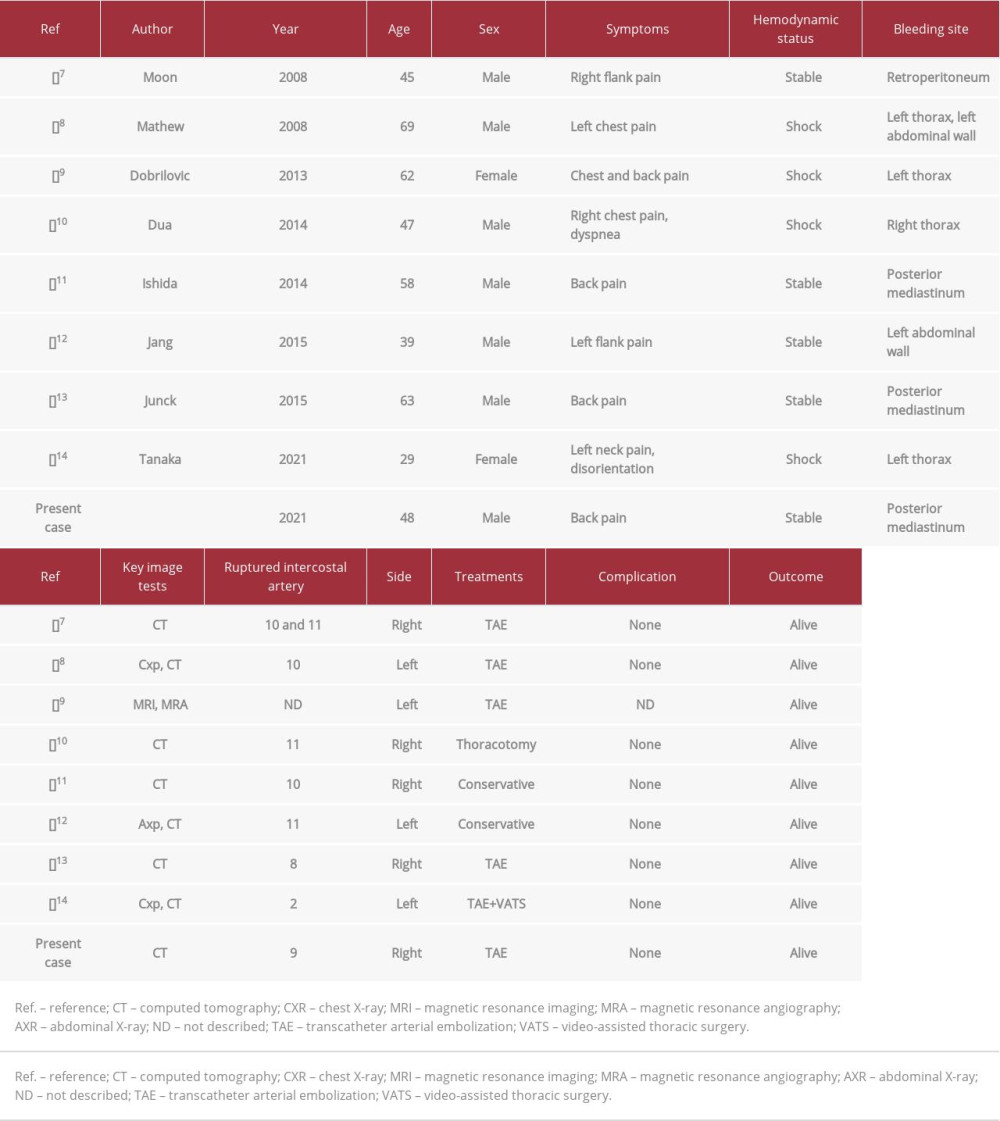 Table 2.. Summary of previous cases and the present case with spontaneous intercostal artery rupture without known underlying disease.
Table 2.. Summary of previous cases and the present case with spontaneous intercostal artery rupture without known underlying disease. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








