12 June 2022: Articles 
Decompression Illness Treated with the Hart-Kindwall Protocol in a Monoplace Chamber
Management of emergency care
Yoshiaki Inuzuka1CDEF, Naoki Edo12ACDEFG*, Yuichi Araki3BCD, Takafumi Hoshi4BE, Mayuko Maruta1CD, Nana Nakamoto4BD, Shinya Suzuki5CDFDOI: 10.12659/AJCR.935534
Am J Case Rep 2022; 23:e935534
Abstract
BACKGROUND: Hyperbaric oxygen (HBO₂) therapy in a multiplace chamber is the standard treatment for severe altitude decompression illness (DCI). However, some hospitals may only have a monoplace chamber. Herein, we present the case of a patient with severe altitude DCI caused by rapid decompression during an actual flight operation that was successfully treated through emergency HBO₂ therapy with the Hart-Kindwall protocol, a no-air-break tables with the minimal-pressure oxygen approach in a monoplace chamber due to unavailability of rapid access to a multiplace chamber.
CASE REPORT: A 34-year-old male aviator presented with chest pain, paresthesia, and mild cognitive impairment following rapid decompression 20 minutes after take-off, which comprised 10 minutes of reaching a height of 10 058 m (33 000 feet) and 10 minutes of cruising at that altitude. He then initiated flight descent and landing. He visited a primary clinic, and severe DCI was suggested clinically. However, since the closest hospital with a multiplace chamber was a 3-hour drive away, we provided emergency HBO₂ therapy with the Hart-Kindwall protocol in a monoplace chamber at a nearby hospital 4 hours after the initial decompression. He recovered fully and returned to flight duty 2 weeks later.
CONCLUSIONS: Emergency HBO₂ therapy with the Hart-Kindwall protocol in a monoplace chamber may be a suitable option for severe DCI, especially in remote locations with no access to facilities with a multiplace chamber. However, prior logistical coordination must be established to transfer patients to hospitals with multiplace chambers if their symptoms do not resolve.
Keywords: Altitude, Decompression, Hyperbaric Oxygenation, Adult, Chest Pain, Decompression Sickness, Humans, Male
Background
Decompression illness (DCI) is caused by bubbles in the blood or tissues during or after a reduction in ambient pressure. It is characterized by 2 pathophysiological syndromes: arterial gas embolism (AGE) and the more common decompression sickness (DCS). AGE comprises a series of symptoms caused by alveolar gas expanding and rupturing the alveolar capillaries and entering the arterial circulation. DCS is caused by the formation of and an increase in the size of extravascular and intravascular bubbles when the sum of the dissolved gas tensions (ie, oxygen, carbon dioxide, nitrogen, and helium) and when water vapor exceeds the local absolute pressure [1]. While the incidence of DCI has been reported to be less than 0.1% per exposure in altitude training or flight operation [2], anonymous surveys of high-altitude U.S. Air Force pilots indicated higher frequencies [3]. Thus, concerns exist about a high proportion of unrecognized cases. Moreover, the rare incidence and underreporting of symptoms make it difficult to assess the clinical features of altitude DCI. Nevertheless, in a previous study, the brain has been found to be usually affected in aviators, whereas the spinal cord is most commonly affected in divers [4]. Severe DCI may have long-term neurological and cardiorespiratory effects and can be an inherent danger to flight crews. In the most severe cases, it can result in permanent disability or even death.
Recent hypobaric exposure and symptoms compatible with DCI usually indicate the need for emergency hyperbaric oxygen (HBO2) therapy with oxygen in a pressure chamber [1,5]. The likelihood of complete recovery decreases as the delay between symptom onset and subsequent treatment increases [5]. Although the toxic effects of excessive oxygen can increase the seizure risk during and after HBO2 therapy [6], adverse effects are relatively rare. Therefore, HBO2 therapy must be administered immediately after DCI diagnosis. Usually, a multiplace chamber is better than a single-occupant chamber (a monoplace chamber) for administering HBO2 therapy because the patients can be accompanied during treatment, and it enables the provision of air-breaks. However, some local hospitals only have access to a monoplace chamber. In such cases, a patient’s prognosis may be improved by providing emergency HBO2 therapy in a monoplace chamber using no-air-break tables that meet the requirements of the minimal-pressure oxygen approach [7,8].
Herein, we present a case of a patient with severe altitude DCI caused by rapid decompression during actual flight operation; this was successfully treated through emergency HBO2 therapy with the Hart-Kindwall protocol in a monoplace chamber due to unavailability of rapid access to a multiplace chamber.
Case Report
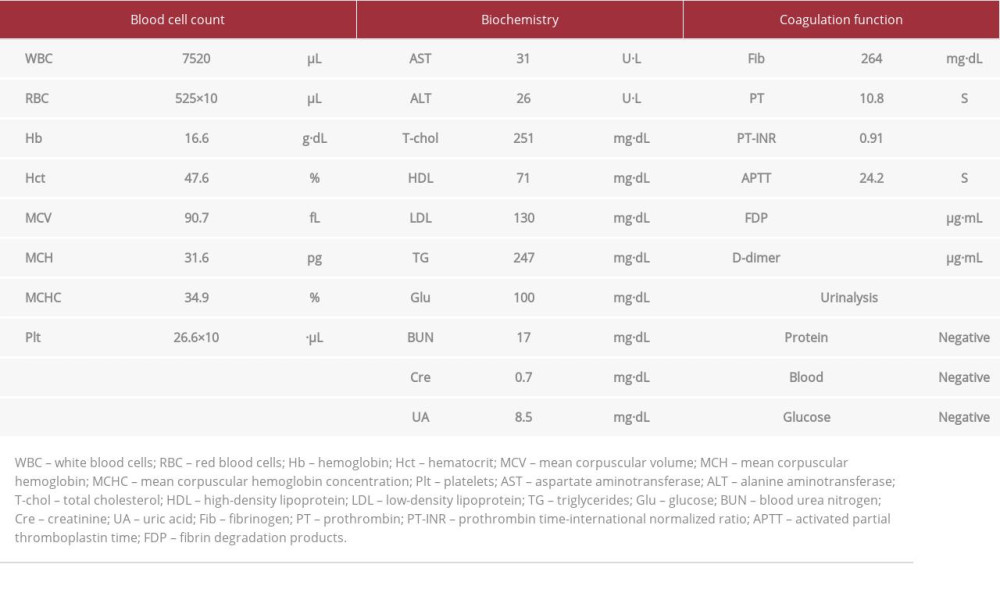
A 34-year-old male aviator visited a clinic and presented with limb numbness and a dazed feeling. On presentation, a physical examination indicated a maximum score of 15 on the Glasgow Coma Scale despite the dazed feeling. His oxygen saturation was 99% with an oxygen mask (5 L·min–1), and his other vital signs were normal. There were no remarkable physical or neurological findings, except for limb numbness and discomfort in the right ear. Laboratory findings are shown in Table 1, and no bubbles were found on the brain, chest, or abdominal computed tomography (CT).
The patient had a past history of hyperuricemia (without medication). He experienced rapid decompression while flying a single-seat, high-performance jet aircraft 20 minutes after take-off, which comprised about 10 minutes of reaching a height of 10 058 m (33,000 feet) and 10 minutes of cruising at that altitude. He immediately initiated the descent of the aircraft, lowering the aircraft to an altitude of 4572 m (15 000 feet) in approximately 3 minutes. He noticed discomfort in his right ear 10 minutes after the decompression. The aircraft reached 2438 m (8000 feet) approximately 13 minutes after the decompression and landed at a nearby airfield 17 minutes after the decompression. Soon after landing, he experienced chest pain and paresthesia and visited a primary care clinic.
We clinically diagnosed him with DCI, started intravenous fluid administration, and determined that emergency HBO2 oxygen therapy was required on suspicion of severe DCI based on his limb numbness and dazed feeling. However, transfer to the nearest hospital with a multiplace hyperbaric chamber would require a 3-hour drive. Thus, emergency HBO2 therapy was administered according to the Hart-Kindwall protocol (283.7 kPa [2.8 atmospheres absolute {atm abs}] for 30 minutes, reduction to 202.7 kPa [2.0 atm abs] over the course of 30 min, maintenance of 202.7 kPa [2.0 atm abs] for 60 minutes, and reduction to ground-level pressure over the course of 30 minutes) at the nearest emergency hospital with a monoplace hyperbaric chamber (Figure 1) [7,8]. Treatment was commenced approximately 4 hours after the initial rapid decompression. On the following 2 days, we administered additional HBO2 treatment (202.7 kPa [2.0 atm abs] for 60 minutes, followed by reduction to ground-level pressure over the course of 30 minutes) to reduce the late recurrence risk [9]. Echocardiography did not reveal any residual bubbles in the venous system and a persistent foramen ovale. All symptoms were resolved following emergency treatment on the first day, and no signs of recurrent DCI were observed. The patient was discharged on the third post-treatment day, and he returned to flight duty 2 weeks after the episode.
Discussion
In this report, we present a case of DCI during actual flight operation, where emergency HBO2 therapy according to the Hart-Kindwall protocol in a monoplace chamber was performed due to unavailability of rapid access to a multiplace chamber. This case is unique because emergency HBO2 therapy was performed for a DCI case that occurred during an actual flight operation.
Altitude DCI develops owing to a series of pathophysiological changes associated with reduced ambient pressure [1]. It poses an inherent danger to flight crews as it can have prolonged effects. In cases involving severe neurological and cardiorespiratory comorbidities, DCI can lead to permanent disability or even death. In high-performance combat aircraft, where weight and performance are primary considerations, there is often a threat to the cabin’s integrity. Therefore, crew members use oxygen equipment throughout the flight, and the cabin differential pressure is relatively low [10].
To minimize the hypoxia effect due to malfunction/misuse of oxygen equipment and reduce the incidence of DCI, the maximum cabin differential pressure employed in practice is less than 34.5 kPa (0.4 atm abs) [10]. In light of a previous review, it is preferable that the cabin altitude does not exceed 5486.4 m (18 000 feet) as a rapid increase in altitude beyond this increases the risk of DCI [1]. Thus, cabin altitude will not exceed an altitude of 5486.4 m (18 000 feet) at differential pressures less than 34.5 kPa (0.4 atm abs) until an aircraft reaches an altitude of approximately 15 910.6 m (52 200 feet). The patient in the present case flew his aircraft above 5486.4 m (18 000 feet) for less than 3 minutes. Furthermore, he started to inhale pure oxygen after he experienced rapid decompression; DCS is not typical under such conditions. However, he had persistent paresthesia and a dazed feeling after landing. As mentioned earlier, the brain has been found to be usually affected in aviators, whereas the spinal cord is most commonly affected in divers [4]. Thus, based on our patient’s symptoms and response to HBO2 therapy, his neurological symptoms might have resulted from pulmonary barotrauma and micro-AGE rather than pulmonary-DCS and micro-AGE, although no bubbles were detected on the brain, chest, or abdominal CT. The risk of DCI is associated with various factors, such as denitrogenation, exercise, and duration of exposure and susceptibility to decompressed pressure [11]. The patient did not exhibit any evident risk factors for DCI, including dehydration and repeated decompression.
Type II altitude DCS, along with AGE – now mostly referred to as severe DCI – has a wide range of manifestations, including joint pain, neurologic changes, pulmonary symptoms, and skin manifestations (Table 2) [1,12]. Joint pain is the most common of these manifestations, affecting 70.7–86.1% of patients with type II DCS; this is followed by neurological symptoms (10.8–32.9%), such as paresthesia and numbness [2,13,14]. The wide variation in the frequencies of neurological symptoms may be attributed to differences in the documented signs and symptoms, the arbitrary nature by which DCI affects the nervous system, and the possibility of other etiologies (eg, hyperventilation). In our case, results of the physical examination findings were unremarkable, and the patient’s symptoms were limited to transient chest pain, paresthesia, and a dazed feeling. A previous study reported that in some cases, patients are unaware of any cognitive impairments, which can only be detected via direct examination [1]. Therefore, a neurological examination should be performed in suspected DCI cases, if available, including radiographic examination such as CT. An exception would be a case where there is a rapid evolution of obvious neurological abnormalities, and in such cases HBO2 therapy should be initiated without delay.
HBO2 is the only definitive treatment for DCI. Its aims include the inhibition of disease progression, quick resolution of signs and symptoms, and prevention of residual effects [1,5]. It is recommended that patients with severe DCI be treated in multiplace chambers [1]. Monoplace chambers are less optimal for treating severe DCI owing to the limited patient access in cases involving a sudden change in clinical condition and a potential risk of oxygen toxicity due to the lack of an air-break. However, this disadvantage must be balanced against the risks associated with the long time required for patient transfer from a remote facility to a hospital with a multiplace chamber. Cianci et al [15] reviewed the outcomes in 140 DCI cases and evaluated the Hart-Kindwall protocol with short, no-air-break tables and demonstrated its effectiveness. Therefore, the use of this protocol for HBO2 therapy in a monoplace chamber could be a feasible alternative in facilities without rapid access to a multiplace chamber for patients with DCI. Furthermore, facilities providing emergency HBO2 therapy using a monoplace chamber should have pre-established arrangements for transferring patients to hospitals with multiplace chambers in the event that treatment is unsuccessful.
Owing to the nature of DCI, it is difficult to conduct a randomized trial to evaluate the efficiency and safety of short, no-air-break tables in a monoplace chamber. Further accumulation of cases is necessary to evaluate the effectiveness of these protocols.
Conclusions
In conclusion, the findings from our case indicate that the use of the Hart-Kindwall protocol for emergency HBO2 therapy in a monoplace chamber may be a suitable option for treating severe DCI, particularly at remote facilities without rapid access to a multiplace chamber.
References:
1.. Vann RD, Butler FK, Mitchell SJ, Moon RE, Decompression illness: Lancet, 2011; 377(9760); 153-64
2.. Bason RD, Yacavone , Bellenkes AH, Decompression sickness: USN operational experience 1969–1989: Aviat Space Environ Med, 1991; 62(10); 994-96
3.. Bendrick GA, Ainscough MJ, Pilmanis AA, Bisson RU, Prevalence of decompression sickness among U-2 pilots: Aviat Space Environ Med, 1996; 67(3); 199-206
4.. Wirjosemito SA, Touhey JE, Workman WT, Type II altitude decompression sickness (DCS): US Air Force experience with 133 cases: Aviat Space Environ Med, 1989; 68(3); 256-62
5.. Xu W, Liu W, Huang G, Decompression illness: Clinical aspects of 5278 consecutive cases treated in a single hyperbaric unit: PLoS One, 2012; 7(11); e50079
6.. Bennett MH, Lehm JP, Mitchell SJ, Wasiak J, Recompression and adjunctive therapy for decompression illness: Cochrane Database Sys Rev, 2012; 2012(5); CD005277
7.. Hart GB, Treatment of decompression illness and air embolism with hyperbaric oxygen: Aerosp Med, 1974; 45(10); 1190-93
8.. Kindwall EP, Use of short versus long tables in the treatment of decompression sickness and air embolism: Treatment of decompression illness. Proceedings of the 45th Undersea and Hyperbaric Medical Society Workshop, 1996; 122-26, Kensington (MD), Undersea and Hyperbaric Medical Society
9.. Hampson N, Atik D, Central nervous system oxygen toxicity during routine hyperbaric oxygen therapy: Undersea Hyperb Med, 2003; 30(2); 147-53
10.. Gradwell D, Rainford D: Ernsting’s aviation medicine, 2006; 84-116, London, CRC Press
11.. Kumar KV, Waligora JM, Calkins DS, Threshold altitude resulting in decompression sickness: Aviat Space Environ Med, 1990; 61(8); 685-89
12..
13.. Ryles MT, Pilmanis AA, The initial signs and symptoms of altitude decompression sickness: Aviat Space Environ Med, 1996; 67(10); 983-89
14.. Weien RW, Baumgartner N, Altitude decompression sickness: Hyperbaric therapy results in 528 cases: Aviat Space Environ Med, 1990; 61(9); 833-36
15.. Cianci P, Slade JB, Delayed treatment of decompression sickness with short, no-air-break tables: review of 140 cases: Aviat Space Environ Med, 2006; 77(10); 1003-8
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250