11 November 2022: Articles 
Inflammation of Pericardial Transverse Sinus Leading to Suspicion of Takayasu Syndrome
Challenging differential diagnosis, Educational Purpose (only if useful for a systematic review or synthesis), Rare coexistence of disease or pathology
Dominika Stępniak1ABCDEF*, Maciej Żechowicz1ABDF, Beata Moczulska1DF, Leszek Gromadziński1EGDOI: 10.12659/AJCR.937196
Am J Case Rep 2022; 23:e937196
Abstract
BACKGROUND: The purpose of this case report was to present a rare course of pericarditis starting with transverse sinus inflammation in a patient with recurrent chest pain. Typically, the effusion accumulates along the diaphragmatic surface of the back heart, and other localizations, such as the transverse sinus, are uncommon. The main risk factor for pericarditis in Europe is viral infection. In this uncommon case, we strongly suspected underlying Takayasu syndrome. The positive response to treatment with steroids in pericarditis and Takayasu arteritis may be misleading.
CASE REPORT: A 61-year-old woman was admitted to the Cardiology Clinic because of recurrent chest pain in the form of a retrosternal burning pain with radiation to both arms. With the results of laboratory tests, electrocardiogram, and computer tomography (CT), we excluded acute coronary syndrome, pulmonary embolism, and aortic dissection. In chest CT and transthoracic echocardiography (TTE), we found an effusion around the ascending aorta with uncertain inflammation and in the transverse sinus of the pericardium. After typical pericarditis treatment with non-steroidal anti-inflammatory drugs (NSAIDs) and afterward with steroids, which is similar to Takayasu syndrome treatment, we observed a significant improvement of the patient’s clinical condition and no recurrence of chest pain.
CONCLUSIONS: Despite clinical symptoms, laboratory results, and aorta thickening with surrounding inflammation, Takayasu syndrome was excluded by rheumatologists because of the patient’s age. Transverse sinus inflammation is a very rare presentation of pericarditis, but should be considered, especially based on TTE and CT imaging, when other possible causes of retrosternal pain are excluded.
Keywords: Pericarditis, Takayasu arteritis, Female, Humans, Middle Aged, Pericardium, Chest Pain, Inflammation
Background
Pericarditis is an inflammatory process caused by infectious factors, autoimmune diseases, diseases of surrounding organs, metabolic disorders, pregnancy, injuries, neoplastic processes, and idiopathic factors [1]. Idiopathic factors are the most common cause for pericarditis in the United Kingdom and Western Europe [2,3]. Most often, this idiopathic factor is caused by viruses [3], in contrast to in developing countries, where the main cause is tuberculosis among immunosuppressed patients [2,4]. Most often, inflammatory effusion accumulates along the diaphragmatic surface of the back heart, but sometimes it accumulates in other parts of the pericardium, such as the transverse sinus. Transverse pericardial sinus inflammation is a rare presentation of pericarditis, in which effusion is localized between the ascending aorta and the left atrium [5].
Independent from the location of inflammation, patients with an acute onset of pericarditis experience sudden, sharp pain in the chest, which can radiate to the neck, left shoulder, and jaw. Additionally, shortness of breath, cough, rhinorrhoea, low-grade fever, fatigue, and weight loss could be observed [6]. For this reason, the pericarditis should be differentiated from a myocardial infarction, myocarditis [6], unstable angina, pulmonary embolism, heart failure aggravation, pathological musculoskeletal conditions, pneumonia, pneumothorax, lung cancer, and gastroenterological diseases [7].
Pericarditis treatment should be based on the main etiological factor, and usually only high-risk patients with fever, immuno-suppression, anticoagulation therapy or no improvement after an initial 7-day treatment with non-steroidal anti-inflammatory drugs (NSAIDs) should be considered for hospitalization [6]. NSAIDs or aspirin with colchicine are the usual first-line treatment [8]. The second-line treatment is corticosteroids [2,6,7]. Most patients have a good prognosis, but some develop recurrent pericarditis. The main risk factors of complicated pericarditis are a high level of C-reactive protein (CRP), early use of corticosteroids, and omission of colchicine in treatment [3].
Takayasu syndrome is an inflammatory disease of the large and medium arteries, such as the aorta. The first manifestation of this kind of vasculitis could be aortic wall thickening [9] in some cases, but pericarditis in the first phase is rare [10]. Corticosteroids are the most common option in the treatment of Takayasu syndrome, similar to the advanced second-line schema for pericarditis [9,11]. The diagnosis of Takayasu syndrome is difficult in daily clinical practice. Among the 6 criteria (3 of them should be fulfilled) are age below 40 years, difference in systolic blood pressure of at least 10 mm Hg between the upper limbs, claudication of an upper limb, a murmur over a subclavicular artery or abdominal aorta by auscultation, weaker pulse, mainly in any of the upper limbs, and arteriogram abnormality (according to the American College of Rheumatology criteria). At the same time, the literature describes later forms of disease, which is diagnosed in patients over 50 or 60 years of age [12,13]. The purpose of the present case was to present a rare course of pericarditis starting with transverse sinus inflammation in a patient with recurrent chest pain of an unknown origin. Additionally, it led to the suspicion of Takayasu syndrome, based on the computed tomography (CT) scans of the aorta, laboratory tests, and positive response to the final treatment with steroids.
Case Report
A 61-year-old woman had periodic chest pain for nearly 2 years, usually in the form of a retrosternal burning pain with radiation to both arms, especially when inhaling and lying down. The symptoms had been strongly aggravated in the last 2 weeks (3/6 points in visual analogue scale [VAS]), with accompanying dyspnea. Since then, she was hospitalized several times in Emergency Departments and had short-lasting clinical effect after various medications and after acute coronary syndromes were excluded, based on Troponin T (TnT) protocols and repeated electrocardiograms (ECGs). Because of a history of asthma, she was also hospitalized in the Pulmonary Department, where, once again, cardiac ischemia was excluded based on TnT (0.004 ng/mL; N<0.014 ng/mL) and ECG findings (Figure 1). In angiographic CT of the chest, pulmonary embolism, aortic dissection, and pneumonia were excluded, but the examination revealed a slight contrast enhancement around the ascending aorta within the pericardium. Additionally, the coronary vessels visible in the scans had neither features of calcifications nor relevant stenosis; therefore, invasive coronary angiography had not been performed. Moreover, the patient’s case was discussed with invasive cardiologists and cardiac surgeons in reference hospital, and no indications for invasive diagnostics or treatment were found. No additional pericardial effusion was observed at that time. Because of a high CRP level (123 mg/L; N<5 mg/L) and sterile blood cultures, empirical antibiotic therapy was included (clarithromycin, cefuroxime). With a primary diagnosis of aortic inflammatory process, the patient was transferred to our clinic for further care.
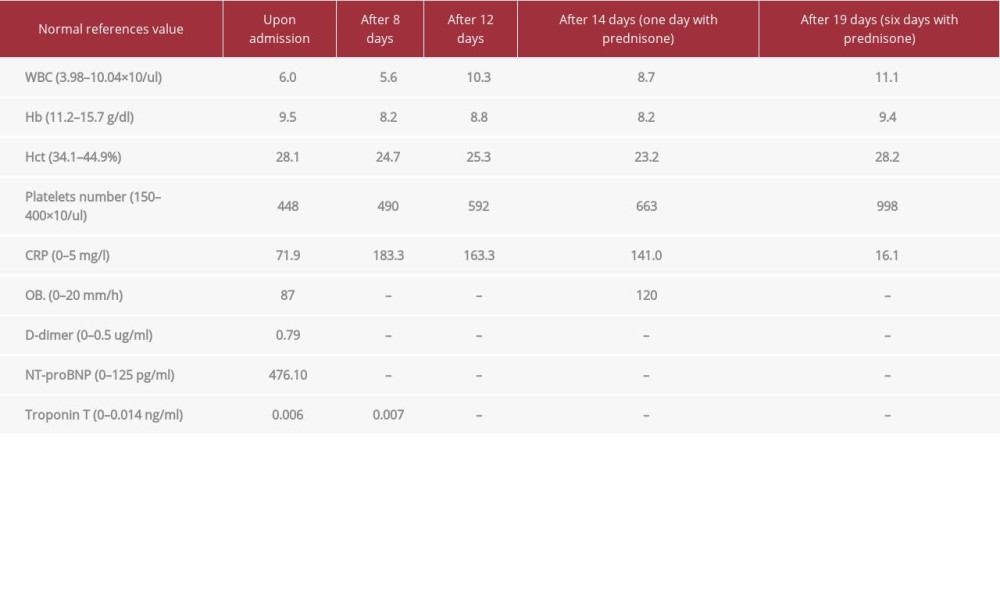
On physical examination, an audible systolic murmur in the Erb’s point and on the apex (3/6) was detected, without any other clinically relevant pathology. In laboratory tests, CRP (71.9 mg/L), erythrocyte sedimentation rate (OB, 87 mm/h), fibrinogen (670 mg/dL), platelet count (663×103/uL), and NT-pro-BNP (476 pg/mL) were significantly elevated. Moreover, the tests showed anemia (Hb 10.2 g/dL), without leucocytosis (Table 1). The transthoracic echocardiography (TTE) revealed hyperechogenic pericardial effusion in the vicinity of the ascending aorta and the left atrium (max 10–11 mm in diastole), without echocardiographic evidence of a cardiac tamponade (Figure 2). After additional sessions with radiologists and re-interpretation of the previous TTEs and chest CT scans, a rare diagnosis of transverse sinus pericarditis was proposed (Figure 3).
After 12 days, despite the treatment with colchicine (0.5 mg per day), NSAID (ibuprofen 600 mg 3 times a day), and antibiotics (cefuroxime 750 mg 3 times a day with ciprofloxacin 400 mg 2 times a day, then amikacin 500 mg 2 times a day and metronidazole 500 mg 3 times a day), the chest pain was significantly aggravated (9/10 points on VAS scale), with a need of strong analgesics usage, including morphine. Temporarily, the patient needed vasopressors because of a tendency to low blood pressure (85/55 mm Hg). In laboratory tests, worsening of anemia (8.2 g/dL), increased thrombocytosis (490 tys/uL), and increased CRP level (185 mg/L) were observed. In repeated
TTEs, increasing pericardial effusion was noted (up to 13 mm in diastole), without any features of possible cardiac tamponade or indirect features of pulmonary embolism (Figure 4). In angio-CT of the chest, enlarged mediastinal lymph nodes were detected, as well as further thickening in the wall of aortic arch and ascending aorta to 3.5 mm. In chest X-ray, an accumulation of effusion in the right pleural space was confirmed. The viral or bacterial background was excluded (B and C hepatitis, Lyme disease, odontogenic focus), as well as tuberculosis, which remains a very important differential diagnosis for autoimmune diseases. The examination of the right pleural effusion showed transudate, without any bacterial infection. Considering no evidence for bacterial etiology of pericardial effusion and no presentation of cardiac tamponade with a high risk of complications after paracentesis, we withdrew from this procedure, suspecting an autoimmune background of the disease. There were no indices of neoplastic diseases in additional diagnostics (endoscopy, abdominal CT scan). Finally, corticosteroids (prednisone) were added as the second-line pericarditis treatment.
After 6 days of prednisone treatment with 60 mg a day, the patient reported having no chest pain. The follow-up TTE showed significant reduction of pericardial effusion (1–2 mm in diastole). Furthermore, the level of CRP decreased significantly (16.1 mg/L), but the platelet number increased at the same time (998 tys/uL). Due to previous inflammatory changes in the aortic wall and the quick and positive reaction to prednisone treatment, Takayasu syndrome was suspected, although the criteria according to the American College of Rheumatology were not sufficiently fulfilled. The patient was discharged with plans for further diagnostics and treatment in the Rheumatology Outpatient Clinic.
The entire pharmacological treatment lasted 3 months (ASA and ibuprofen for 3 weeks, colchicine for 3 months, and prednisone for about 12 weeks, in decreasing doses). In the follow-up TTE and angio-CT scan of the chest after the first 12 months, there were further reductions of pericardial effusion and aortic wall thickening observed. In the Hematology Department, any significant bone marrow failure was excluded. Moreover, Takayasu syndrome was finally excluded by the Rheumatology Department, as the necessary 3 of 6 diagnostic criteria were not fulfilled (they could not be fulfilled because the patient was >40 years old). Therefore, the reason for the unusual pericarditis and aortic inflammation were not fully clarified. Similarly, the accompanying anemia seemed to have an inflammatory autoimmune background, because the hematological and onco-logical background were excluded and the anemia significantly and permanently improved after the treatment with steroids.
The patient remained under cardiologic and rheumatologic follow-up, without recurrence of the primary symptoms, despite occasionally having some slight retrosternal pain.
Discussion
Pericarditis is an inflammatory process caused by many different risk factors [1]. Without typical symptoms on physical examination, about 85% of patients present with pericardial friction rub, which is similar to pleural friction [14] but is not mandatory for the final diagnosis, especially when the pericar-dial effusion is relatively recent and not yet hyperechogenic. In electrocardiography, diffuse ST segment elevations and PR segment depression (especially present in I, II, aVL, V3–V5) are typical, dependent on the location of the pericardial inflammation and accompanying myocarditis. QT prolongation is mostly not present, compared to in acute coronary syndromes [2,14]. In laboratory tests, CRP, troponin, and CK-MB levels are usually elevated. In noninvasive diagnostic technologies, such as TTE, transesophageal echocardiography (TEE), CT, and cardiac magnetic resonance, we can find a pericardial effusion coexisting with or without adjacent heart muscle impairment [2]. Despite the highly advanced imaging in CT and cardiac magnetic resonance, liquid in the transverse sinus is most commonly detected incidentally. The main issue for the clinician is to correctly differentiate the normal and pathological structure surrounding the heart [15], and the transverse sinus is certainly one of the structures communicating between the left and right pericardial space in the close vicinity of the 2 outflow arteries of the heart. For these reasons, the preferred method should be TTE or TEE. Transthoracic parasternal long-axis views and transesophageal long-axis views show space between the ascending aorta and the left atrium [5]. In daily clinical practice, all noninvasive methods should be complementary and widely used, although they are available only at more advanced sites.
In the present case, during prolonged hospitalization, we performed comprehensive diagnostics and confirmed the diagnosis of rare transverse sinus pericarditis, which later developed into larger pericardial effusion. Our patient presented the typical symptoms of pericarditis, such as acute pain in the chest and dyspnea when lying down. Additionally, the laboratory tests showed an ongoing inflammatory process. Although we performed thorough diagnostic testing, a specific risk factor and the inflammatory trigger were primarily not found. In accordance with cardiology guidelines, in the first-line treatment we used an NSAID (ibuprofen) and colchicine [2,7], with no improvement. Therefore, after necessary exclusion of bacterial infection or tuberculosis, corticosteroids were implemented as the second-line treatment [2,3]. The advantage of this therapy is quick symptom relief; however, according to many systematic reviews and meta-analyses, there is a relationship between corticosteroid use and an increase in the risk of disease recurrence [2,3]. Another meta-analysis by Mager et al showed the combination of colchicine and prednisone results in an increase of the recurrence rate [16].
In the present case, the patient’s clinical condition deteriorated quickly under the colchicine and NSAID treatment. After addition of the corticosteroids to the schema, we observed a rapid improvement of the clinical condition, regression of the pericardial effusion, and CRP level normalization. Based on that, a dysfunction of the immune processes was suspected. Moreover, imaging tests revealed thickening of the aortic arch and ascending aorta, which indicated an ongoing inflammatory process in this vessel. Based on the obtained results, we suspected Takayasu syndrome. Unfortunately, the subsequent tests by rheumatologists did not confirm the diagnosis, since the patient met only 2 necessary diagnostic criteria. Takayasu arteritis can have a spectrum of presentation ranging from asymptomatic to catastrophic disease, presenting as malignant hypertension. As symptoms are nonspecific and the disease is so rare, there is often a delay in detecting it. In our case, despite the clinical presentation, aortic inflammation on CT scan, and positive laboratory tests, Takayasu syndrome could not be confirmed. Fortunately, despite many risk factors of recurrent pericarditis (like high level of inflammatory factors, bad general condition, combination of colchicine and steroids), a new onset of pericarditis has not been observed for more than 36 months, at the time of this report.
Conclusions
Transverse sinus inflammation is a rare presentation of pericarditis, but should be considered, especially based on TTE and CT images, when other possible causes of retrosternal pain are excluded. Each time, a thorough search for the background of pericarditis should be done, as the reason enables efficient and life-saving treatment to be conducted. In the present case, despite symptoms, laboratory results, and aorta thickening with surrounding inflammation, Takayasu syndrome was excluded by the rheumatologists because of the patient’s age and lack of additional criteria set by the American College of Rheumatology; although, from the clinical point of view, there was a strong suspicion of the disease. Fortunately, the steroid-based pharmacological treatment was successful, independent of the confirmation of this rare rheumatic disease, which we think first presented with transverse sinus inflammation.
Figures
References:
1.. Maisch B, Seferović PM, Ristić AD, Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology: Eur Heart J, 2004; 25(7); 587-610
2.. Tuck BC, Townsley MM, Clinical update in pericardial diseases: J Cardiothorac Vasc Anesth, 2019; 33(1); 184-99
3.. Cremer PC, Kumar A, Kontzias A, Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment: J Am Coll Cardiol, 2016; 68(21); 2311-28
4.. Gleen F, Diethelm AG, Surgical treatment of constrictive pericarditis: Ann Surg, 1962; 155(2); 883-93
5.. Penmasta S, Silbiger JJ, The transverse and oblique sinuses of the pericardium: Anatomic and echocardiographic insights: Echocardiography, 2019; 36(1); 170-76
6.. Doctor NS, Shah AB, Coplan N, Kronzon I, Acute pericarditis: Prog Cardiovasc Dis, 2017; 59(4); 349-59
7.. Rahman A, Saraswat A, Pericarditis: Aust Fam Physician, 2017; 46(11); 810-14
8.. Lazaros G, Tousoulis D, Vassilopoulos D, Editorial commentary: Recurrent pericarditis in the era of interleukin-1 inhibition: Trends Cardiovasc Med, 2021; 31(5); 275-76
9.. Tacoy G, Management of Takayasu arteritis: Future Cardiol, 2018; 14(2); 105-8
10.. Derg AK, Pericarditis as an initial symptom in Takayasu arteritis: Anatol J Cardiol, 2011; 375-76
11.. Gori T, Coronary vasculitis: Biomedicines, 2021; 9(6); 622
12.. Sharma BK, Jain S, Suri S, Numano F, Diagnostic criteria for Takayasu arteritis: Int J Cardiol, 1996; 54(Suppl.); S141-47
13.. Onen F, Akkoc N, Epidemiology of Takayasu arteritis: Presse Med, 2017; 46(7–8 Pt 2); e197-e203
14.. Snyder MJ, Bepko J, White M, Acute pericarditis: Diagnosis and management: Am Fam Physician, 2014; 89(7); 553-60
15.. Żurada A, Ustymowicz A, Loukas M, Computerized tomography of the transverse pericardial sinus: Normal or pathologic?: Clin Anat, 2017; 30(1); 61-70
16.. Mager A, Talmor Y, Chezar Azzerad C, Does colchicine decrease the rate of recurrence of acute idiopathic pericarditis treated with glucocorticoids?: J Cardiol, 2018; 71(4); 409-13
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250