08 November 2022: Articles 
Apixaban-Associated Diffuse Alveolar Hemorrhage in an Elderly Man with Multiple Complications
Unusual clinical course, Adverse events of drug therapy
Takuya Ozawa1ABCDE, Hideki Terai1ACDE*, Akiyoshi Kajino2ABC, Shiro Otake1ABCDE, Ayaka Saito1ABC, Miyuki Nishie1ABCD, Yoshikazu Kishino2ABC, Hirofumi Kamata1ABCD, Kentaro HayashidaDOI: 10.12659/AJCR.937809
Am J Case Rep 2022; 23:e937809
Abstract
BACKGROUND: Diffuse alveolar hemorrhage (DAH) caused by direct oral anticoagulants (DOACs) has increased in recent years with the increase in prescriptions of DOACs. Generally, DOACs are considered to have a lower bleeding risk than the traditional anticoagulant, warfarin. However, major bleeding, including DAH, due to DOACs can be seen in clinical practice, and there are few reports to elucidate when DOAC-associated alveolar hemorrhage occurs and whether DOAC-induced DAH has a trigger.
CASE REPORT: An 80-year-old man diagnosed and treated for atrial fibrillation with apixaban 2.5 mg twice daily for 1 year before admission, underwent 2 invasive medical procedures over a short period of time. Hemoptysis began after the procedures. He experienced shortness of breath and rapidly progressive hypoxic respiratory failure. His postsurgical oxygen saturation level dropped rapidly. Chest radiography and computed tomography images showed pulmonary infiltration and ground-glass opacity in both lungs. Apixaban treatment was discontinued, and mechanical ventilation was initiated. Bronchoalveolar lavage cytology revealed hemosiderin-laden macrophages. A diagnosis of diffuse alveolar hemorrhage (DAH) was made. In previous reports about DAH caused by DOACs, most patients had bleeding triggers; drug interactions in patients taking DOACs are one of such triggers. Although DOACs are relatively safe for elderly patients, DAH can occur in patients receiving either early-stage or long-term treatment.
CONCLUSIONS: The onset of DOAC-associated DAH is not limited to the early stages of medication initiation. Various triggers can induce DAH in patients receiving DOACs.
Keywords: Apixaban, Hemorrhage, Male, Humans, Aged, Aged, 80 and over, Warfarin, Pyridones, Anticoagulants, Atrial Fibrillation, Lung Diseases, Respiratory Insufficiency, Stroke, Administration, Oral
Background
Diffuse alveolar hemorrhage (DAH) is a fatal disease [1]. While many causes of DAH are immune-mediated, non-immune-mediated causes include drug-induced DAH [2]. DAH caused by direct oral anticoagulants (DOACs) has increased in recent years with the increase in prescriptions of DOACs [3]. In several clinical trials comparing DOACs with warfarin for atrial fibrillation, gastrointestinal bleeding was more common in the DOAC groups (especially in the rivaroxaban and high-dose edoxaban groups), but overall major bleeding tended to be similar or less in the DOAC groups [4–7]. In a randomized double-blind study of 5395 patients with acute venous thrombosis, major bleeding occurred in 0.6% of patients who received apixaban and in 1.8% of those who received conventional therapy (sub-cutaneous enoxaparin, followed by warfarin). The study concluded that apixaban is associated with a significantly lower rate of major bleeding than that associated with conventional therapy [8]. These results suggest that the risk of bleeding is generally lower with DOACs, including apixaban. However, it is also true that major bleeding, including DAH, due to DOACs can be seen in clinical practice, and there are few reports to elucidate when DOAC-associated alveolar hemorrhage occurs and whether DOAC-induced DAH has a trigger.
We report a case of apixaban-induced DAH that occurred more than 1 year after treatment initiation and required mechanical ventilation. We also reviewed this case based on previous reports of DOAC-associated DAH.
Case Report
An 80-year-old man was prescribed apixaban 2.5 mg twice daily for atrial fibrillation for 1 year before admission. A reduced dose of apixaban was used because he was above 80 years old and weighed 48 kg, which is less than 60 kg. His medical history included hypertension, dyslipidemia, and cerebral infarction, for which he was receiving enalapril 2.5 mg and rosuvastatin 2.5 mg once daily. Fifteen days before admission, he underwent transcatheter aortic valve implantation for aortic stenosis via a right femoral artery puncture. After being discharged from the hospital, he presented with right coxalgia and was re-admitted to the hospital with suspected septic arthritis of the hip. The patient was prescribed loxoprofen 60 mg 3 times a day as an analgesic. Antibiotic treatment with cefazolin was initiated, but his symptoms did not improve. On day 8, right hip lavage drainage was performed under general anesthesia. The right hip joint was released and washed with saline. The joint fluid was not cloudy, and bacteriological evaluation was negative, reducing the possibility of infectious arthritis. Hemoptysis began after the surgery, and he experienced shortness of breath and rapidly presented with progressive hypoxic respiratory failure. On physical examination, lung auscultation revealed bilateral coarse crackles. Chest radiography revealed infiltration in the left upper lung fields and ground-glass opacity in the bilateral lower lung fields (Figure 1); chest computed tomography images showed the same findings (Figure 2). The apixaban treatment was discontinued, and mechanical ventilation was initiated on day 12.
Laboratory findings showed a white blood cell count of 8.8×103/µL, hemoglobin level of 7.3 g/dL, activated partial thromboplastin time of 46 s, prothrombin time-international normalized ratio of 1.62, creatinine level of 0.81 mg/dL, C-reactive protein level of 22.8 mg/dL, urine occult blood (1+), urine red blood cell cast of 10–19/HPF, and a positive fecal occult blood test. We performed bronchoalveolar lavage of the inferior lingular segment on day 13, and the collected fluid contained blood (Figure 3). We considered the possibility of traumatic intubation to be low, since no obvious bronchial injury was observed using bronchoscopy.
Bronchoalveolar lavage cytology revealed hemosiderin-laden macrophages. Testing for connective tissue disease and vasculitis evaluation were negative, and heart failure was ruled out through a cardiologist’s examination, including echocardiography. Given these clinical findings, alveolar hemorrhage secondary to apixaban was diagnosed [2]. We also suspected complications of bacterial pneumonia and changed cefazolin to piperacillin-tazobactam; however, the bacterial culture of the collected fluid was negative. The patient’s respiratory condition improved, and chest radiography revealed significant improvement (Figure 4). On day 16, he was extubated and exhibited no recurrence of anemia or hemoptysis; thus, apixaban was resumed and he was subsequently discharged.
Discussion
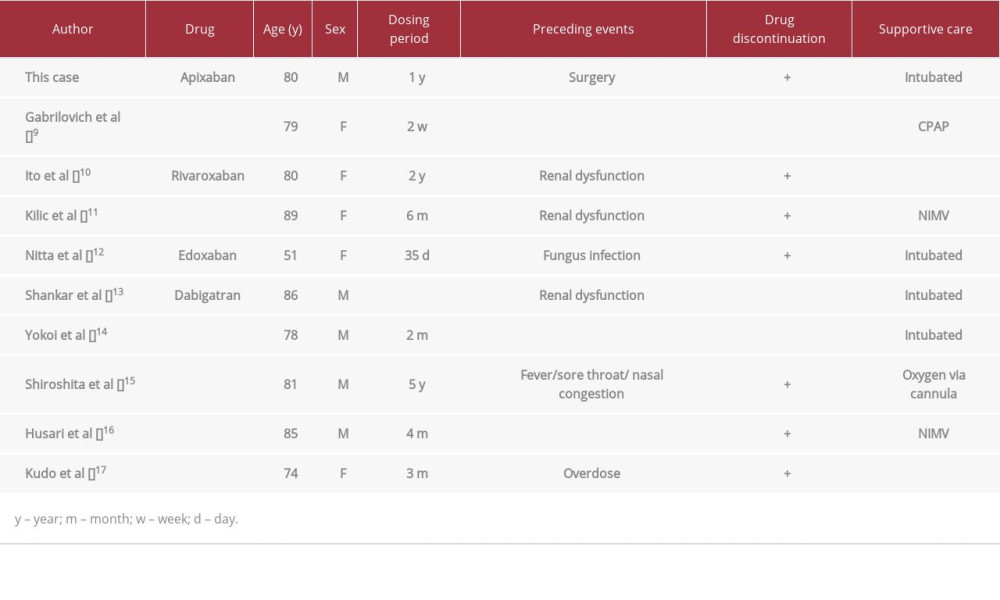
Previous case reports of alveolar hemorrhage caused by DOACs (apixaban, rivaroxaban, edoxaban, and dabigatran) [9–17], are summarized in Table 1.
Only 1 study reported apixaban-induced alveolar hemorrhage. The median age of the patients was 80 years, and several patients required high-flow oxygenation, noninvasive ventilation, and tracheal intubation. Cases with bleeding tendencies, such as hematuria and melena, were included. In the present case, laboratory findings revealed a urine red blood cell cast and positive fecal occult blood test results, and we considered coagulation disorder caused by apixaban as the cause of DAH.
The 9 previous cases and the present case are shown in Table 1. The time between the initiation of DOACs and the onset of alveolar hemorrhage varied from 2 weeks to 5 years. In the present case, 1 year had passed since the initiation of apixaban therapy.
Six cases had preceding events; 3 were due to renal dysfunction, 2 were due to infection, and 1 was due to overdose. In the present case, the patient had no renal dysfunction or overdose. Generally, elderly patients are at an increased bleeding risk owing to low body weight [18], but this is insufficient to explain the sudden onset 1 year after the initiation of apixaban. The patient underwent 2 surgeries before the onset of DAH, which might have been too invasive for an elderly patient, resulting in deterioration of his general condition and the DAH caused by DOACs. Non-steroidal anti-inflammatory drugs (NSAIDs) were administered preoperatively. Given that NSAIDs can increase the likelihood of bleeding complications of DOACs [19], they were also considered as a trigger for DAH. Furthermore, hemorrhagic events due to concurrent administration of dabigatran and cephalosporins have been reported [20]. Although there are no reports about hemorrhagic events due to concurrent administration of apixaban and cephalosporins, DAH was triggered by the drug interaction between antibiotics and apixaban in the present case. The calculated imputability score was I3, because there was no cause of DAH other than the effects of apixaban, and DAH was a reported adverse event that improved with discontinuation [21,22]. Although the evaluation did not reveal any infection, we cannot exclude the possibility that bacterial pneumonia might have contributed to DAH.
The onset of DOAC-associated DAH is not limited to the early stages of medication initiation. With the increase in the number of DOAC prescriptions [3], similar cases are expected more frequently in clinical practice. Although DOACs are generally associated with lower rates of fatal bleeding than those associated with warfarin in elderly people [23], it should be recognized that DAH can occur with various triggers in patients taking DOACs.
Conclusions
The onset of DOAC-associated DAH is not limited to the early stages of medication initiation. Various triggers, such as multiple surgeries, infections, and drug interactions, can induce DAH in patients receiving DOACs.
Figures
References:
1.. Ugajin M, Kani H, Hattori H, Anticoagulant use as an independent risk factor and higher in-hospital mortality in patients showing alveolar hemorrhage in diffuse lung disease: Medicina (Kaunas), 2021; 57; 1094
2.. Lara AR, Schwarz MI, Diffuse alveolar hemorrhage: Chest, 2010; 137; 164-71
3.. De Jong LA, Koops M, Gout-Zwart JJ, Trends in direct oral anticoagulant (DOAC) use: Neth J Med, 2018; 76; 426-30
4.. Granger CB, Alexander JH, McMurray JJV, Apixaban versus warfarin in patients with atrial fibrillation: N Engl J Med, 2011; 365; 981-92
5.. Patel MR, Mahaffey KW, Garg J, Rivaroxaban versus warfarin in nonvalvular atrial fibrillation: N Engl J Med, 2011; 365; 883-91
6.. Giugliano RP, Ruff CT, Braunwald E, Edoxaban versus warfarin in patients with atrial fibrillation: N Engl J Med, 2013; 369; 2093-104
7.. Connolly SJ, Ezekowit MD, Yusuf S, Dabigatran versus warfarin in patients with atrial fibrillation: N Engl J Med, 2009; 361; 1139-51
8.. Agnelli G, Buller HR, Cohen A, Oral apixaban for the treatment of acute venous thromboembolism: N Engl J Med, 2013; 369; 799-808
9.. Gabrilovich MI, Buxton DE, Lykins DM, Diffuse alveolar hemorrhage secondary to apixaban administration: Chest, 2014; 146; e115-16
10.. Ito Y, Kondo S, Itani H, Diffuse alveolar hemorrhage associated with rivaroxaban therapy: The Journal of the Japan Society for Respiratory Endoscopy, 2018; 40; 216-20
11.. Kilic S, Saracoglu E, Alkan G, A rare complication in a patient taking rivaroxaban: Alveolar hemorrhage: Turk Kardiyol Dern Ars, 2018; 46; 73-75
12.. Nitta K, Imamura H, Yashio A, Diffuse alveolar hemorrhage associated with edoxaban therapy: Case Rep Crit Care, 2016; 2016; 7938062
13.. Shankar S, Saxena A, Saverimuthu A, Dabigatran-associated diffuse alveolar hemorrhage: Am J Ther, 2020; 27; e301-3
14.. Yokoi K, Ishida K, Kimura T, Adachi T, Diffuse alveolar hemorrhage associated with dabigatran: Intern Med, 2012; 51; 2667-68
15.. Shiroshita A, Nakashima K, Tanaka Y, Successful treatment with idarucizumab for diffuse alveolar hemorrhage induced by dabigatran etexi-late: A case report: J Thromb Thrombolysis, 2018; 46; 271-73
16.. Husari A, Beydoun A, Ammar AS, The untold story of Dabigatran etexilate: Alveolar hemorrhage in an elderly patient with interstitial pulmonary fibrosis: J Thromb Thrombolysis, 2013; 35; 81-82
17.. Kudo K, Tanimoto Y, Hisamoto A, Dabigatran etexilate-induced alveolar hemorrhage: Annals of the Japanese Respiratory Society, 2012; 247-50 1:
18.. Bauersachs RM, Herold J, Oral anticoagulation in the elderly and frail: Hamostaseologie, 2020; 40; 74-83
19.. Edith AN, Allison B, John F, Pharmacology of anticoagulants used in the treatment of venous thromboembolism: J Thromb Thrombolysis, 2016; 41; 15-31
20.. Giuseppe L, Emmanuel JF, Camilla M, Combined administration of antibiotics and direct oral anticoagulants: A renewed indication for laboratory monitoring?: Semin Thromb Hemost, 2014; 40; 756-65
21.. Gawai PP, Overview of important methods used for causality assessment of adverse drug events in pharmacovigilance: Journal of Pharmacovigilance and Drug Research, 2020; 1; 6-12
22.. Dangoumau J, Evreux JC, Jouglard J, [Mehtod for determination of undesirable effects of drugs.]: Therapie, 1978; 33; 373-81 [in French]
23.. Wilkinson C, Wu J, Searle SD, Clinical outcomes in patients with atrial fibrillation and frailty: Insights from the ENGAGE AF-TIMI 48 trial: BMC Med, 2020; 18; 401
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250