30 November 2022: Articles 
An Infant with Bilateral Keratitis: From Infectious to Genetic Diagnosis
Challenging differential diagnosis
Louis-Philippe Thibault1ABCDEF*, Grant A. Mitchell2BCDEF, Brigitte Parisien1BCDE, Patrick HamelDOI: 10.12659/AJCR.937967
Am J Case Rep 2022; 23:e937967
Abstract
BACKGROUND: Tyrosinemia Type II (TYRII) is a rare autosomal recessive inborn error of metabolism caused by deficiency of tyrosine aminotransferase (TAT), leading to hypertyrosinemia. TYRII patients often present in the first year of life with ocular and cutaneous findings, including corneal ulcers, pseudodendritic keratitis, and palmoplantar hyperkeratosis. The corneal involvement is often mistaken for herpes simplex virus (HSV) keratitis, which is a much commoner condition.
CASE REPORT: A previously healthy 10-month-old male infant was referred to Ophthalmology for acute onset photophobia. Bilateral dendritiform corneal lesions raised the suspicion for herpetic keratitis. Additionally, a papular, crusted lesion was found on his thumb after a few days of hospitalization, also raising concerns about HSV. The patient’s clinical condition seemed to improve under intravenous acyclovir and supportive treatment. A conjunctival swab and crusted lesion on the thumb were tested for HSV using a polymerase chain reaction (PCR) technique, and both were negative. Nevertheless, given the clinical presentation and the favorable course of signs and symptoms, hospital discharge was planned with oral acyclovir. It was halted by an alternative diagnosis of autosomal recessive inborn error of metabolism, tyrosinemia type II, confirmed by elevated plasma tyrosine level and later by molecular analysis requested as a confirmatory investigation by the genetics medical team.
CONCLUSIONS: The corneal involvement in TYRII is often mistaken for HSV keratitis, and clinical course alone should not halt further investigations to rule out TYRII. Clinicians should suspect TYRII clinically when its characteristic ocular dendritiform lesions are present, namely in infancy or early childhood, and even in the absence of its typical cutaneous palmoplantar hyperkeratosis plaques.
Keywords: Herpes Simplex, Keratitis, Dendritic, Metabolism, Inborn Errors, Tyrosinemias, Child, Preschool, Infant, Humans, Male, Keratitis, Herpetic, Corneal Ulcer, acyclovir, Administration, Intravenous
Background
Tyrosinemia type II (TYRII), also known as oculocutaneous tyrosinemia or Richner-Hanhart syndrome, is a rare autosomal recessive inborn error of metabolism. It was first defined by Richner in 1938 and the description of its clinical presentation was confirmed by Hanhart in 1947 [1,2]. It is caused by deficiency of tyrosine aminotransferase (TAT), leading to hypertyrosinemia. Tyrosinemia type I, caused by deficiency of the enzyme fumarylacetoacetase, and tyrosinemia type III, caused by deficiency of p-hydroxyphenylpyruvic acid dioxygenase, do not present with the oculocutaneous findings of TYRII [3]. Although tyrosinemia type I is now included in many Canadian newborn screening programs, the screening marker (succinylacetone) is specific to tyrosinemia type I. The term, “tyrosinemia screening” may provide a false sense of security because TYRII is not detected by this test. Diagnosis requires awareness of the clinical signs of TYRII, a high level of clinical suspicion, and confirmation by plasma amino acid chromatography [1]. While histopathological investigation is not part of the usual workup, findings from skin biopsy may show hyperkeratosis, acanthosis, and parakeratosis, which are not specific to TYRII [1–6].
In the first year of life, 75% to 85% of TYRII patients present with ocular findings, including photophobia, conjunctival redness, increased lacrimation, corneal ulcers, and pseudodendritic keratitis [3,4,7]. The corneal involvement is often mistaken for herpes simplex virus (HSV) keratitis, which is a much commoner condition. However, in these cases, it will usually be recalcitrant to antiviral treatment [3,8–11]. Patients also present in the same time frame with cutaneous findings, namely palmoplantar hyperkeratosis. These lesions usually present as plaques on hypothenar and thenar eminences of the soles and palms and can be painful [4,7].
Neurodevelopmental delay and intellectual disability are inconsistently present in affected patients and occurs in up to 50–60% of subjects [1,2,4,8].
While this clinical triad – ocular, cutaneous and neurodevelop-mental abnormalities – outlines the usual findings in TYRII patients, it is worth noting that manifestations may occur in only 1 of these areas, namely on initial presentation [7,8,10–17].
Clinicians should suspect TYRII clinically when its characteristic ocular and/or cutaneous manifestations appear in infancy or early childhood. We report the case of a male infant with the ocular clinical signs described above, who had undergone HSV workup and treatment and who was clinically improving.
Case Report
A 10-month-old previously healthy White infant was referred to Ophthalmology for acute onset of photophobia. He was born at term to a primiparous mother, following an unremarkable pregnancy. His weight gain and development were normal. The mother reported a 7-day history of eye blinking and rubbing, irritability, and decreased oral intake. Ophthalmological examination showed significant photophobia, epiphora, and difficulty maintaining his eyelids open. Dendritiform corneal lesions were seen bilaterally, raising the suspicion of herpetic keratitis. The mother confirmed she had been having cold sores. The presence of herpes simplex virus (HSV) had never been tested for, but the lesions responded well to valacyclovir. An Infectious Diseases consultant recommended hospitalization for intravenous acyclovir treatment. A conjunctival swab and a papular, crusted, raised lesion on the thumb were each tested for HSV using a polymerase chain reaction (PCR) technique. Both PCRs were negative. Daily ophthalmological examinations showed ongoing improvement. After 10 days of intravenous acyclovir, the corneal lesions had resolved completely. Hospital discharge was planned with an additional week of oral acyclovir. However, at discharge, the physician received an urgent call from the biochemical genetics laboratory suggesting an alternate diagnosis.
Plasma amino acid chromatography was performed because of the presence of dentritiform corneal lesions, compatible with tyrosinemia type II (TYRII, also known as oculocutaneous tyrosinemia or Richner-Hanhart syndrome). The diagnosis of TYRII was confirmed by finding a markedly elevated plasma tyrosine level (1262 µmol/L, reference range, 40–80 µmol/L). TYRII enters the differential diagnosis of bilateral keratitis in young infants. After 2 weeks on diet, the patient’s plasma tyrosine level was 152 µmol/L, which is mildly elevated. The corneal lesions had not recurred. The small, papular, crusted lesion on the thumb, while not necessarily related to TYRII, had disappeared. One year later, his developmental milestones were age-appropriate.
Molecular analysis further confirmed the diagnosis of TYRII, revealing 2 variants in the TAT gene, 1 from each parent: c.889C>T (p.Arg297*, a known pathogenic premature stop variant) and c.227T>C (p.Leu76Pro, not previously reported, of unknown significance, although other variants at this residue can cause TYRII). Following diagnosis confirmation, the family received genetic counselling about the way TYRII has been inherited in their child, how it could affect another child of their own, and the way it could be passed to the next generation if their child also wanted to have children himself (following autosomal recessive inheritance, as shown in Figure 1). Additionally, the family was given general information about this rare disease and explanations regarding the usual clinical evolution and prognosis. The parents also received nutritional counselling from the Genetics Division’s dietician. See Table 1 for previously published TYRII case reports emphasising ocular clinical presentation.
Discussion
TYRII is a rare autosomal recessive inborn error of metabolism caused by deficiency of tyrosine aminotransferase (TAT), leading to hypertyrosinemia. TAT is encoded by the TAT gene on chromosome 16q22.1. The mechanisms by which TAT deficiency leads to ocular and cutaneous findings remain unclear, but may be related to an inflammatory response to deposition of tyrosine crystals in corneal epithelium and spinous cells of epidermis [3,8]. Prior to diagnosis, the fact that our patient clinically improved under supportive care and intravenous acyclovir but without therapeutic restrictive diet aligns with this hypothesis of underlying inflammatory process. To the best of our knowledge, it is the first case report to document such clinical improvement initially, without appropriate dietary restriction. This should even further raise awareness among general pediatricians and primary care providers about the importance of ruling out TYRII in children with pseudodentritic keratitis alone, regardless of the initial clinical evolution. Several other authors have discussed the diagnostic confusion that may exist with HSV in the context of ocular pseudodentritic keratitis lesions, but all of these authors reported patients who eventually clinically deteriorated and/or did not respond to acyclovir, which differs from our case [3,8–11,14,17].
Unlike classic HSV-associated cutaneous vesicular lesions, TYRII usually causes painful, irregular, discrete, non-vesicular hyper-keratotic lesions of the palms and soles, and their presence strongly suggests the diagnosis of TYRII. Patients often, but not always, show painful hyperkeratotic lesions of the flexor surfaces of palms, fingers, soles, and toes [8,9]. This is consistent with the presentation of our patient, as typical palmoplantar lesions were not present. Indeed, similarly to the case we describe, previous reports also presented patients in which pseudodentritic keratitis was the first and sometimes the only clinical manifestation of TYRII [8,10–18]. Moreover, it has been previously reported that skin lesions may at first be small, subtle, and difficult to differentiate from other keratotic lesions [4]. This also aligns with the present case, as the small, papular, crusted lesion found on the thumb of the child was rather non-specific, but may have been the initial development of the palmoplantar hyperkeratotic lesions typically found in TYRII patients.
TYRII patients are also at risk for learning problems and intellectual disability, although this does not affect all patients [1].
No developmental delay was identifiable at the follow-up visit in the child we describe. However, it might be too early to make such an assessment, as others have described patients presenting neurodevelopmental impairment later in life, justifying the relevance of a lifelong follow-up [3].
In patients with ocular and/or cutaneous lesions suggestive of TYRII, the diagnosis is confirmed by amino acid chromatography showing hypertyrosinemia (>500 µmol/L in patients on a normal diet).
Management involves dietary restriction of tyrosine and phenylalanine, with supplementation with other essential amino acids, vitamins, and trace elements, allowing for normal growth, as well as follow-up with metabolic genetics. This regimen lowers plasma tyrosine levels, and oculocutaneous signs resolve in days to weeks. This was the case for our patient, which is consistent with descriptions in the literature [9]. During hospitalization, the fact that the child showed clinical improvement raised many questions within the medical team. While the introduction of the appropriate diet is the only correct treatment for TYRII, our hypothesis remains that supportive treatment given to the patient in conjunction with intravenous acyclovir, including generous intravenously administered fluids and anti-inflammatory drugs, helped reduce the inflammation of the corneal lesions and helped child’s anabolism, hence explaining the clinical improvement. Continuation of this treatment might have shown otherwise, as transient improvement has been described following HSV keratitis treatment in TYRII patients [8]. Nevertheless, early clinical diagnosis with metabolic control is the criterion standard for therapy and to prevent profound neurological impairment [1].
Conclusions
Pediatricians must consider tyrosinemia type II (TYRII) in infants and young children with bilateral herpes-like corneal lesions, especially if they are recurrent and culture-negative. With this case report, we suggest that suspicion of TYRII should also be present even if it is the first ocular episode of that sort and even if the child is presenting clinical improvement under supportive care. Early introduction of diet therapy effectively controls eye and skin signs and potentially prevents or limits learning and intellectual disabilities in TYRII patients.
References:
1.. Scott CR, The genetic tyrosinemias: Am J Med Genet C Semin Med Genet, 2006; 142c(2); 121-26
2.. Viglizzo GM, Occella C, Bleidl D, Rongioletti F, Richner-Hanhart syndrome (tyrosinemia II): Early diagnosis of an incomplete presentation with unusual findings: Pediatr Dermatol, 2006; 23(3); 259-61
3.. Locatelli F, Puzenat E, Arnoux JB, Richner-Hanhart syndrome (tyrosinemia type II): Cutis, 2017; 100(6); E20-22
4.. Kaye CI, Accurso F, La Franchi S, Newborn screening fact sheets: Pediatrics, 2006; 118(3); e934-63
5.. el-Shoura SM, Tallab TM, Richner-Hanhart’s syndrome: New ultrastructural observations on skin lesions of two cases: Ultrastruct Pathol, 1997; 21(1); 51-56
6.. Larrègue M, De Giacomoni P, Odièvre P, Prigent F, Changes in the keratinocytes in oculo-cutaneous tyrosinosis: Richner-Hanhart syndrome: Ann Dermatol Venereol, 1980; 107(11); 1023-30
7.. al-Essa MA, Rashed MS, Ozand PT, Tyrosinaemia type II: An easily diagnosed metabolic disorder with a rewarding therapeutic response: East Mediterr Health J, 1999; 5(6); 1204-7
8.. Macsai MS, Schwartz TL, Hinkle D, Tyrosinemia type II: Nine cases of ocular signs and symptoms: Am J Ophthalmol, 2001; 132(4); 522-27
9.. Martin GC, de Lonlay P, Chapron T, Bilateral dendriform ulcer leading to an early diagnosis of tyrosinemia type 2: J AAPOS, 2020; 24(2); 120-22
10.. Charlton KH, Binder PS, Wozniak L, Digby DJ, Pseudodendritic keratitis and systemic tyrosinemia: Ophthalmology, 1981; 88(4); 355-60
11.. Soares DC, Stroparo MN, Lian YC, Herpetiform keratitis and palmoplantar hyperkeratosis: Warning signs for Richner-Hanhart syndrome: J Inherit Metab Dis, 2017; 40(3); 461-62
12.. Colditz PB, Yu JS, Billson FA, Tyrosinaemia II: Med J Aust, 1984; 141(4); 244-45
13.. Goddé-Jolly D, Larregue M, Roussat B, Van Effenterre G, A case of Richner-Hanhart syndrome (tyrosinosis with ocular, cutaneous and mental manifestations): J Fr Ophtalmol, 1979; 2(1); 23-28
14.. Gokhale NS, Dherai AJ, Desai H, Ashavaid TF, Unusual dendritic keratitis: Indian J Ophthalmol, 2007; 55(1); 57-59
15.. Hervé F, Moreno JL, Ogier H, Incurable keratitis and chronic palmoplantar hyperkeratosis with hypertyrosinemia. Cure using a tyrosine-restricted diet. Type II tyrosinemia: Arch Fr Pediatr, 1986; 43(1); 19-22
16.. Podglajen-Wecxsteen O, Delaporte E, Oculocutaneous type II tyrosinosis: Ann Dermatol Venereol, 1993; 120(2); 139-42
17.. Tsai CP, Lin PY, Lee NC, Corneal lesion as the initial manifestation of tyrosinemia type II: J Chin Med Assoc, 2006; 69(6); 286-88
18.. Kymionis GD, Kankariya VP, Kontadakis GA, Ziakas NG, Isolated corneal pseudodendrites as the initial manifestation of tyrosinemia type II in monozygotic twins: J Pediatr Ophthalmol Strabismus, 2012; 49 Online: e33–36
Tables
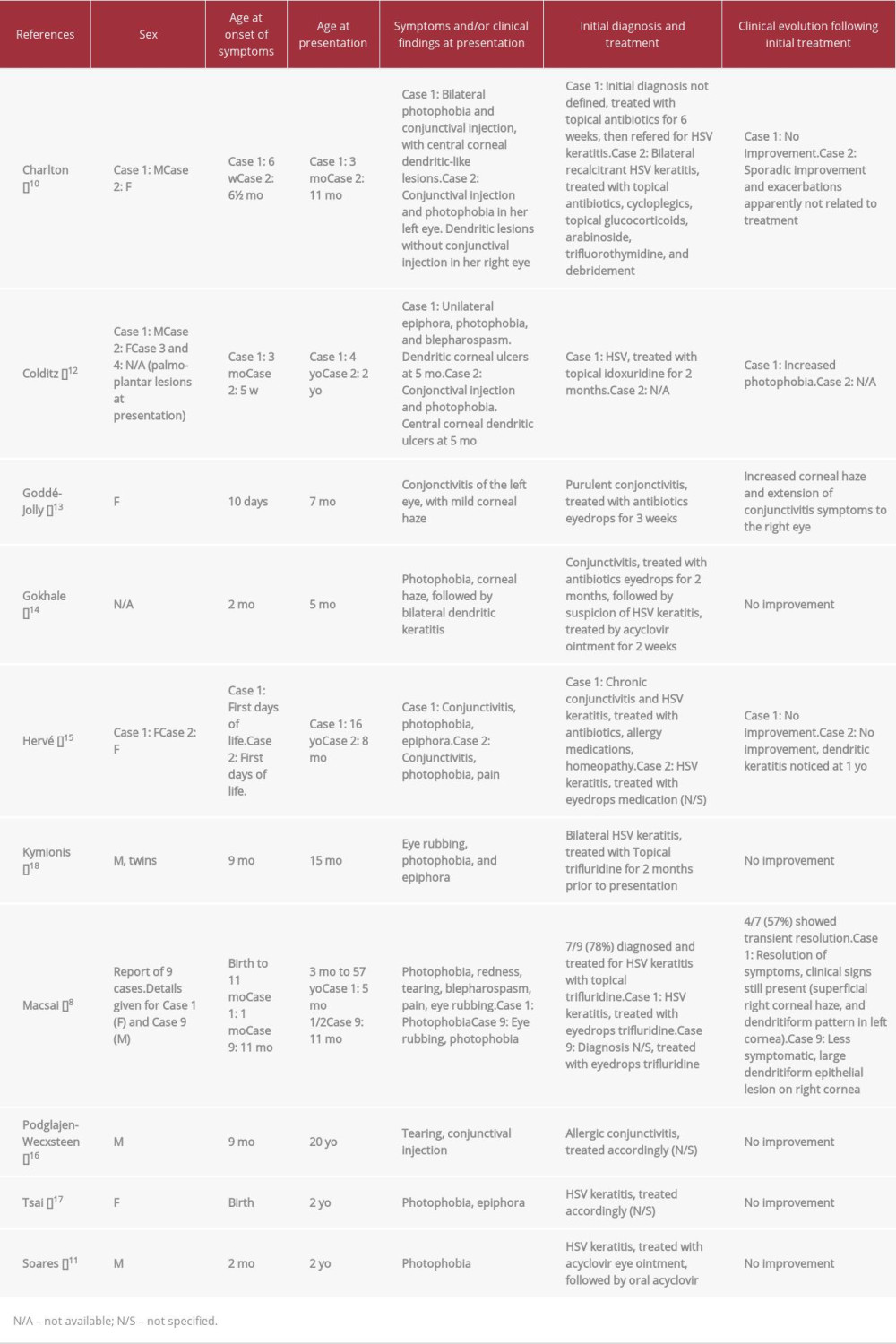 Table 1.. Comparison of main characteristics of previously published TYRII case reports, with emphasis on ocular lesions at initial clinical presentation (presented in author alphabetical order).
Table 1.. Comparison of main characteristics of previously published TYRII case reports, with emphasis on ocular lesions at initial clinical presentation (presented in author alphabetical order).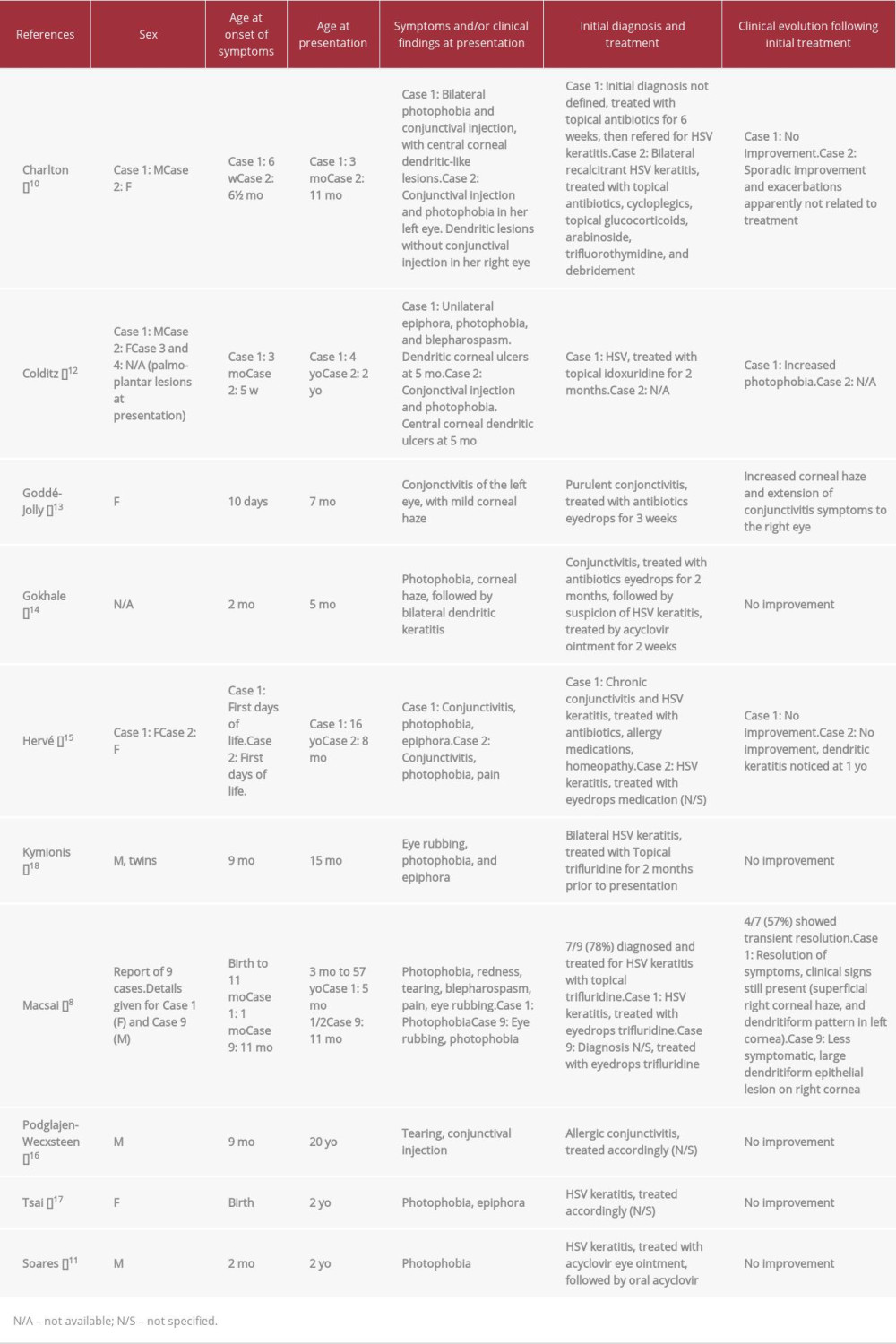 Table 1.. Comparison of main characteristics of previously published TYRII case reports, with emphasis on ocular lesions at initial clinical presentation (presented in author alphabetical order).
Table 1.. Comparison of main characteristics of previously published TYRII case reports, with emphasis on ocular lesions at initial clinical presentation (presented in author alphabetical order). In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








