26 April 2023: Articles 
Laparoscopic Cholecystectomy in a Patient with Situs Inversus Totalis and a Double Superior Vena Cava
Challenging differential diagnosis, Rare coexistence of disease or pathology
Nizar Abu-oddos1BE, Mohammad Abu-JeyyabDOI: 10.12659/AJCR.938774
Am J Case Rep 2023; 24:e938774
Abstract
BACKGROUND: Situs inversus totalis (SIT) is an uncommon condition characterized as a congenital disorder in which the visceral organs are inverted relative to their typical anatomical position. SIT with double superior vena cava (SVC) is an even rarer presentation. Due to the underlying anatomical difference, the diagnosis and treatment of gallbladder stones in patients with SIT are challenging.
CASE REPORT: We report the case of a 24-year-old male patient who presented with an intermittent history of epigastric pain for 2 weeks. Clinical assessment and radiological investigations confirmed gall bladder stones with evidence of SIT and double superior vena cava (SVC). The patient underwent elective laparoscopic cholecystectomy (LC) with an inverted laparoscopic approach. The recovery from the operation went smoothly, the patient was discharged from the hospital the following day, and the drain was removed on the third postoperative day.
CONCLUSIONS: Because anatomical variations in the SIT can affect localization of symptoms in patients with complicated gallbladder stones, the diagnosis of patients who have abdominal pain and SIT necessitates both a high index of suspicion and a thorough assessment. Although LC is considered to be a technically challenging surgery and calls for modification of the standard protocol, it is nevertheless feasible to perform the procedure effectively. To the best of our knowledge, this is the first time that LC has been documented in a patient who has SIT and double SVC.
Keywords: Cholecystectomy, Laparoscopic, persistent left superior vena cava, Situs Inversus, Male, Humans, young adult, Adult, Vena Cava, Superior, Laparoscopy, Gallstones, Dextrocardia
Background
Situs inversus (SI) is an extremely uncommon form of congenital abnormality that results from restriction of visceral rotation during the early stages of embryonic development [1]. SI can develop with primary ciliary dyskinesia (PCD), a recessive genetic disease that disrupts motile cilia [1,2]. Early in development, motile cilia generate a leftward fluid flow that helps form the left-right body axis in an embryonic formation [2,3]. When recessive PCD mutations prevent leftward flow, the viscera’s position becomes random [3,4]. Although the methods by which non-PCD genes regulate visceral laterality are not fully known, some of these genetic codes for proteins are linked with cilia rather than coding directly for cytoskeletal components of cilia [3].
Estimates indicate that SI occurs 1 in 5000–25 000 births [1,3]. SI refers to a variety of visceral transpositions in the body, such as situs inversus totalis (SIT), in which both the chest and abdominal organs are reversed, generating a mirror image of the normal anatomical structures, and situs inversus partialis, in which either the thoracic or abdominal organs are reversed. Situs ambiguous, on the other hand, refers to the presence of an abnormally positioned organ [4].
During the embryonic period, atrophy or patency of particular veins connected with the cardinal veins, which are considered the embryo’s primary venous drainage system, may result in variants such as double superior vena cava (SVC), double inferior vena cava (IVC), or other uncommon venous connections [5]. Double SVC is the most common congenital abnormality of SVC, with a prevalence of up to 0.5% in normal populations [5,6]. It is a rare abnormality characterized by the persistence of the left SVC, which is formed by the union of the right common cardinal vein and the right anterior cardinal vein and is primarily derived from the right anterior cardinal vein [7].
Diagnosis and treatment of symptomatic gallbladder stones in SIT patients can be challenging; thus, we are presenting this case to the surgical community in the hopes that it would be of assistance to others. Although minimally invasive surgery is the preferable approach, it is technically challenging due to anatomical diversity [8]. However, a study of the relevant literature revealed that laparoscopic cholecystectomy (LC) is feasible and safe for this patient population [9]. No mortalities or major complications, such as bile duct injury, were reported [7,9]. In addition, ERCP combined with endoscopic sphincterotomy was utilized to successfully manage the accompanying CBD stone [9].
We present for the first time a patient with SIT associated with double SVC who required LC due to symptomatic gallstones.
Case Report
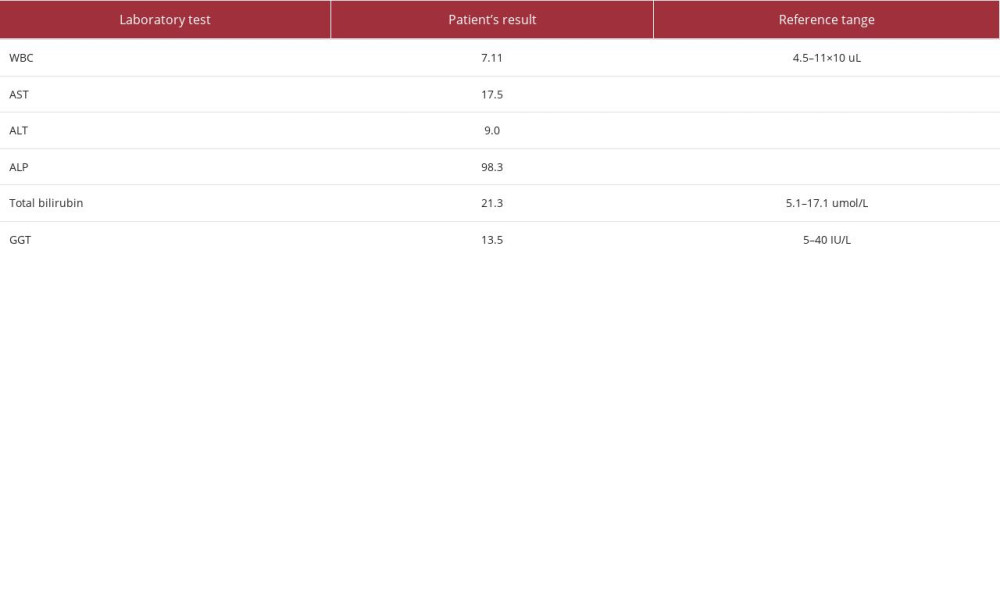
A 24-year-old man known to have SIT started to have constant epigastric and left upper-quadrant (LUQ) pain with a severity of 8/10. The pain radiated to the back and was associated with eating a fatty meal. He started to have chills, nausea, and diarrhea, with no vomiting. The physical examination revealed no fever or jaundice at the time of examination, but he had LUQ tenderness. The laboratory work-up documented normal WBC, liver function test for aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP), and total bilirubin (T-Bil) and gamma-glutamyl transferase (GGT) showed levels of 17.5 IU/L, 9.0 IU/L, 98.3 IU/L, 21.3 umol/L, and 13.5 IU/L, respectively (Table 1).
Ultrasound of the abdomen confirmed the situs inversus; the liver was on the left side, and the spleen was on the right, with normal echotexture of the liver, spleen, and kidneys. However, the gall bladder was contracted, and the common bile duct was dilated and measured about 1.6 cm, with suspicion of stone impaction distally. There was no evidence of peritoneal free fluid in the abdomen or pelvis.
Chest, abdominal, and pelvic CT scans revealed SIT and duplicated SVC. The liver, spleen, pancreas, and both suprarenal glands had normal echogenicity, with SIT (Figures 1, 2). MRCP revealed a dilated CBD with multiple filling defects observed from the level to the ampullary portion, consistent with CBD stones, and a dilated common hepatic duct (Figure 3).
Elective LC with CBD stone extraction was performed using an inverted laparoscopic approach. We placed an umbilical trocar for the camera and 3 trocars in the normal subcostal positions mirrored to the left. The surgeon and assistant stood on the right side of the patient while the monitor was placed on the left. The intra-abdominal drain left in place. The cystic duct and cystic artery were found and dissected circumferentially until a critical view was achieved. The cystic duct and cystic artery were then double-clipped and dissected with the right hand through the subcostal port. Electrocautery was used to dissect the gallbladder from its peritoneal attachments, and the gall-bladder was removed. The duration of the entire procedure was 55 minutes. We are aware of the conundrum of post-LC drain advantages; we usually insert the drain in complicated cases only, but we felt it would be more reasonable in this case because it was our first time operating on a patient with this anomaly and we wanted to be aware of bile duct injury earlier.
The following day, the patient was released from the hospital, with an uneventful recovery period. The drain was removed on the first postoperative clinic visit.
Discussion
SIT is a generalized defect of situs orientation because it results in a spectrum of laterality disruptions due to the inability to establish normal left-right asymmetry [1]. It develops when the cardiac tubes rotate to the left, and the heart and other internal organs are positioned in the opposite direction of the normal configuration. However, the precise process that controls the rotation and migration of internal organs, or left-right asymmetry, is unknown [10]. SI is typically related to congenital cardiac disease in 3–9% of SIT cases, and almost 80% in situs ambiguous [1]. However, vascular abnormalities such as an interrupted inferior vena cava and a preduodenal portal vein have been recorded in up to 20% and 42%, respectively, of patients with situs anomaly [1].
Superior vena cava (SVC) congenital malformations may emerge as accidental childhood observations, be associated with underlying cardiac conditions, or have a syndromic origin [5]. Persistent left-sided superior vena cava, also known as double SVC, is the most common systemic venous anomaly in the thorax, with a reported prevalence of up to 0.5% in normal populations; however, this percentage is reported to be higher in patients with congenital heart disease, in the range of 3–10% [6,11]. Double SVC is significantly more common in association with situs ambiguous than with other types in up to 60–70% of cases. There appears to be a relationship between the existence of certain SI abnormalities and a higher number of SVC abnormalities. In a group of 18 patients with different kinds of SVC anomalies studied by Buirski et al, 72% had double SVC. SVC duplication can result in hemodynamic instability if it is accompanied by other congenital cardiac defects. In contrast, when this duplication occurs without concomitant cardiac defects, as in our case, the patient is asymptomatic [6].
A patient with SI is typically diagnosed accidentally when using conventional imaging techniques, such as ultrasound (US) or plain film X-rays, and or using advanced imaging modalities like computed tomography (CT) or magnetic resonant imaging (MRI) performed for other medical reasons [1]. This condition can complicate the diagnosis and treatment of common acute surgical illnesses. Gastroenterologists, radiologists, and surgeons rarely see these patients because of their rarity; this anomaly might present itself to even the busiest surgeon once or twice in their whole career. In our case, the patient went to the emergency room reporting only epigastric pain radiating to the left; this finding is described by most published case reports dealing with a cute cholecystitis in this patient population [7].
LC is a very effective treatment for dealing with acute cholecystitis, even if the patient has SIT [7]. However, this approach is more challenging, especially for right-handed surgeons, because of the mirror-image anatomy [9]. LC in SIT is described in a number of published articles [7,9]. However, there is no recognized standard approach, and the authors even propose taking certain additional safety measures to eliminate associated biliary tract anomalies or bile duct injuries. The method we employed is the most common method outlined in a recent systematic review that evaluated the best port placement to perform LC for patients with SI [9]. With this method, the surgeon can conduct the dissection with their right hand through the left midclavicular port while retaining the infundibulum in place with their left hand through the subxiphoid port. Because of the rarity of this anomaly, we were unable to find any literature that discussed the delayed versus the immediate LC for this particular patient cohort.
Intraoperative cholangiogram and ERCP for an associated CBD stone were reported in SI patients during LC; however, CBD exploration with stone extraction has been reported in 1 case [12]. No mortalities or major complications were reported in the literature [7], and 1 instance of conversion to open surgery due to challenging cystic duct dissection in acute cholecystitis has been documented [9].
Conclusions
Diagnosis of patients with abdominal pain and SIT necessitates a high index of suspicion of common causes of acute abdomen and a thorough evaluation, as well as a physical examination and radiological studies. LC is feasible and safe in patients with SIT, although it is technically more challenging.
Figures
References:
1.. Eitler K, Bibok A, Telkes G, Situs inversus totalis: A clinical review: Int J Gen Med, 2022; 15; 2437-49
2.. Fliegauf M, Benzing T, Omran H, When cilia go bad: Cilia defects and ciliopathies: Nat Rev Mol Cell Biol, 2007; 8(11); 880-93
3.. Postema MC, Carrion-Castillo A, Fisher SE, The genetics of situs in-versus without primary ciliary dyskinesia: Sci Rep, 2020; 10(1); 3677
4.. Campbell M, The mode of inheritance in isolated laevocardia and dextrocardia and situs inversus: Br Heart J, 1963; 25; 803-13
5.. Taşkent İ, Danışan G, Aydın AM, Situs inversus totalis with double superior vena cava: An unusual case report: J Surg Med, 2019; 3(10); 774-76
6.. Batouty NM, Sobh DM, Gadelhak B, Left superior vena cava: Cross-sectional imaging overview: Radiol Med, 2020; 125(3); 237-46
7.. AlKhlaiwy O, AlMuhsin AM, Zakarneh E, Taha MY, Laparoscopic cholecystectomy in situs inversus totalis: Case report with review of techniques: Int J Surg Case Rep, 2019; 59; 208-12
8.. Ren JJ, Li SD, Geng YJ, Xiao R, Modified laparoscopic cholecystectomy technique for treatment of situs inversus totalis: A case report: J Int Med Res, 2017; 45(3); 1261-67
9.. Chaouch MA, Jerraya H, Dougaz MW, A systematic review of laparoscopic cholecystectomy in situs inversus: J Invest Surg, 2021; 34(3); 324-33
10.. Pavlidis TE, Psarras K, Triantafyllou A, Laparoscopic cholecystectomy for severe acute cholecystitis in a patient with situs inversus totalis and posterior cystic artery: Diagn Ther Endosc, 2008; 2008; 465272
11.. Burney K, Young H, Barnard SA, CT appearances of congential and acquired abnormalities of the superior vena cava: Clin Radiol, 2007; 62(9); 837-42
12.. Kang SB, Han HS, Laparoscopic exploration of the common bile duct in a patient with situs inversus totalis: J Laparoendosc Adv Surg Tech A, 2004; 14(2); 103-6
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250