01 May 2023: Articles 
Chest Tightness with Cycling Turned Out To Be Pneumomediastinum
Rare disease, Rare coexistence of disease or pathology
Fahad Zafar1ABCDEFG*, Ommar Afzal1ABCDEFGDOI: 10.12659/AJCR.939170
Am J Case Rep 2023; 24:e939170
Abstract
BACKGROUND: Pneumomediastinum, or mediastinal emphysema, means air present inside the mediastinum. It usually presents with symptoms of chest pain and shortness of breath. Examination can be significant for crepitus along the neck area. There are many risk factors associated with pneumomediastinum, including asthma and COVID-19. Most cases of pneumomediastinum improve with conservative management, and surgery (mediastinotomy) is reserved for complicated cases with tension pneumomediastinum.
CASE REPORT: This is the case of a 23-year-old man who presented with chest tightness after 3.5 h of cycling. The patient did have a prior history of clinically stable asthma, with no recent exacerbation, and denied any other associative factors. Imaging was significant for pneumomediastinum. The patient was admitted for observation in the hospital and treated with supportive care, without any surgical intervention. The patient had appropriate improvement in his symptoms in 24 h. Repeat imaging showed improvement in the pneumomediastinum, and the patient was discharged to outpatient follow-up.
CONCLUSIONS: Our case presents a unique link between cycling and pneumomediastinum. Prolonged cycling may emerge as a risk factor for this complication. People with a previous history of pneumomediastinum should be careful to review other risk factors prior to planning long-distance bicycling. Physicians need to keep this differential diagnosis in mind when encountering a patient with similar symptoms so that a timely diagnosis is made.
Keywords: Bicycling, Chest Pain, Pneumomediastinum, Diagnostic, Male, Humans, young adult, Adult, Mediastinal Emphysema, COVID-19, Tomography, X-Ray Computed, Asthma
Background
The mediastinum is the anatomical area between the lungs and has various important structures, including the heart. The presence of air in the mediastinum is described as pneumomediastinum [1]. Secondary pneumomediastinum because of traumatic injury was first presented by Rene Laennec in 1819, and primary or spontaneous pneumomediastinum was later first presented by Louis Hamman in 1939 [2]. There are multiple causative and underlying risk factors associated with pneumomediastinum, which include underlying pulmonary disorders (asthma) and COVID-19. We present a unique case of pneumomediastinum associated with prolonged bicycling, which was managed conservatively, without any surgical intervention.
Case Report
A 23-year-old man with past medical history of asthma presented to the Emergency Department for evaluation of an acute onset of chest tightness. The patient had been visiting his mother in the northeastern United States for summer vacation. He was a young athletic man who enjoyed cycling daily along the canal bank for about 2 h. On the day of presentation, he continued cycling for a total of 3.5 h, but had to stop because he was not feeling well. He initially noticed a change in his voice quality. A few minutes later, he started having tightness in his chest and neck. The patient took a break, but his symptoms did not improve with rest; therefore, he decided to come to Emergency Department for further evaluation.
He denied any recent trauma, significant coughing spells, falls, fever, nausea, vomiting, sick contacts, recent COVID-19 exposure, or any prior similar issues. The patient had no history of smoking, alcohol, or intravenous drug use. He did report that he occasionally smoked marijuana, but he denied using it during this summer holiday time.
The initial evaluation showed that the patient was hemodynamically stable, with a blood pressure of 118/64 mmHg, heart rate of 59 beats per min, respiratory rate of 20 breaths per min, temperature of 36.5°C, and 97% oxygen saturation on room air. The physical examination was significant for crepitus, palpated over the left lateral neck. The lungs were otherwise clear to auscultation, with normal respiratory effort and no wheezing, rhonchi, or crackles. The patient had normal heart sounds with no murmurs, rubs, or gallops.
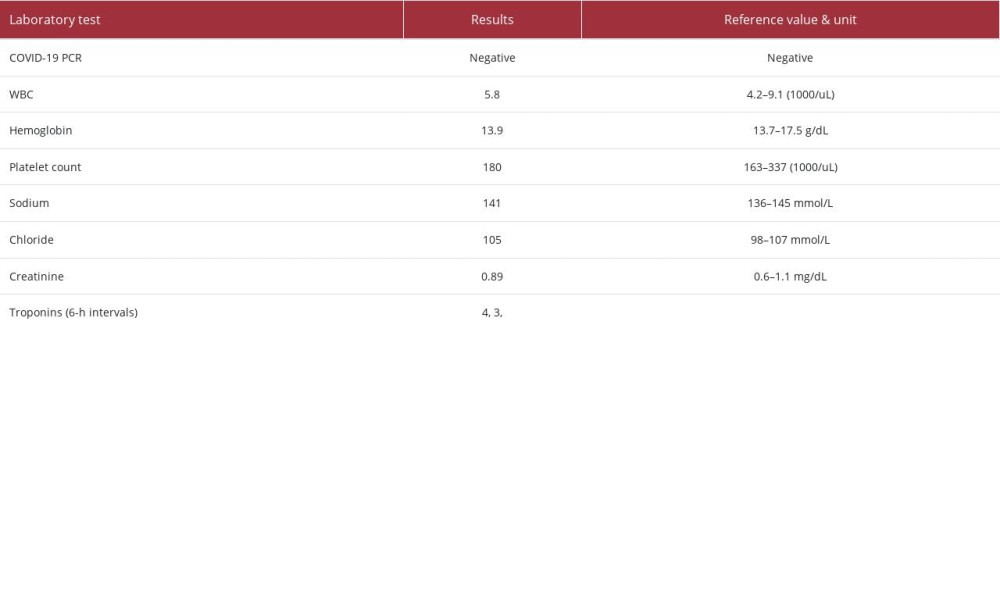
Results of a complete blood count and basic metabolic panel were unremarkable. COVID-19 PCR and troponin tests were negative (Table 1). Electrocardiography showed normal sinus rhythm, with no acute ST- or T-wave changes. An initial chest X-ray with posteroanterior and lateral views (Figure 1) showed pneumomediastinum. Computerized tomography (CT) of the chest (Figure 2A, 2B) and neck area (Figure 3A–3C) with intravenous contrast also showed findings concerning for pneumomediastinum, along with subcutaneous emphysema in the neck area, but no pneumothorax or other acute cardiopulmonary abnormality was noted.
Diagnosis of pneumomediastinum and subcutaneous neck emphysema was made, and the patient was admitted to the hospital for observation. The surgical team was consulted and recommended that no acute surgical intervention was required and that close monitoring of patient’s condition and vitals should continue. His asthma was stable, and lung auscultation did not show wheezing. He was continued on his home inhalers of albuterol, mometasone, and montelukast. His symptoms of chest tightness and voice change improved after a few hours, but he was kept in the hospital overnight for careful observation. A second chest X-ray was done the following day and showed improvement in pneumomediastinum (Figure 4).
The patient was re-evaluated by the surgical team, who recommended that he was stable for discharge since he had improvement in his symptoms, remained hemodynamically stable, and his chest X-ray showed improvement in pneumomediastinum. A follow-up was arranged for the patient the next week with his primary care physician, and he was discharged in stable condition. The patient reported continued improvement and no recurrence of symptoms during a follow-up phone call a week later.
Discussion
Pneumomediastinum, or mediastinal emphysema, means air present inside the mediastinum. It usually presents with symptoms of chest pain and shortness of breath. Examination can be significant for crepitus along the neck area [1]. Pneumomediastinum can be traumatic or non-traumatic [2]. It can be associated with different risk factors. Particularly, repeated coughing spells in acute exacerbation of asthma have been associated with pneumomediastinum [3,4], as has recreational drug use, especially marijuana [2,7] and cocaine use. Our patient did admit to the use of marijuana, and there has also been some association of pneumomediastinum with it [2,7]. Weis et al did a retrospective review of 21 cases of pneumomediastinum over a 1-year period and identified 14 to be associated with marijuana [8].
As we are passing through the phase of the COVID-19 pandemic, there have been many case reports linking coronavirus infection [9,10] with pneumomediastinum as well. However, our patient denied any recent exposure and his COVID-19 PCR test was negative.
Identical to our patient’s case, Cavallari et al described as case of pneumomediastinum associated with exercise in a triathlete involved in cycling, swimming, and running in 2021 [11]. Herrmann et al described a case of pneumomediastinum associated with cycling in March 2022 [12]. To the best of our knowledge, there are no other case reports describing a link between cycling and pneumomediastinum.
Diagnosis is made with imaging modalities of chest X-ray, which shows a radiolucent area along the heart border [1]. A CT scan can further help visualize free air tracking along the anatomical structures [1,5]. If pneumomediastinum is extensive, it can result in free air appearing as radiolucency above the diaphragm and is called a continuous diaphragm sign [1]. If there are any signs or symptoms related to esophageal tear/ perforation, then a swallow study can be done using gastrograffin [13].
Sometimes pneumomediastinum can result in low blood pressure, which is indicative of tension pneumomediastinum. In this phenomenon, the air inside the mediastinum starts putting pressure on the cardiac chambers and vena cava, resulting in restriction in cardiac filling and stroke output. This eventually results in hypotension and shock [14]. Treatment is usually conservative, and surgery (mediastinotomy) is reserved for cases with tension pneumomediastinum.
Conclusions
We have presented a unique case of pneumomediastinum that was seen after prolonged cycling. Excessive exertion or exercise might emerge as a risk factor for pneumomediastinum if this link continues to be reported in other studies. This can help educate the general population (especially athletes) and physicians to identify this condition and provide appropriate management.
Figures
References:
1.. Kouritas VK, Papagiannopoulos K, Lazaridis G, Pneumomediastinum: J Thorac Dis, 2015; 7(Suppl 1); S44-49
2.. Dionísio P, Martins L, Moreira S, Spontaneous pneumomediastinum: Experience in 18 patients during the last 12 years: J Bras Pneumol, 2017; 43(2); 101-5
3.. Okafor C, Soin S, Ferraz JFFM, Spontaneous pneumomediastinum complicating asthma exacerbation: BMJ Case Rep, 2019; 12; bcr-2018-229118
4.. Inês F, Rute M, Abelha PF, Luisa C, Extensive pneumomediastinum following an acute asthma exacerbation: Med Case Rep, 2018; 4(4); 78
5.. Rampuri R, Ali Y, Verkerk M, Unusual cause of pneumomediastinum: BMJ Case Rep, 2018; 2018; bcr-2018-224343
6.. Soares DS, Ferdman A, Alli R, Subcutaneous emphysema and pneumomediastinum following cocaine inhalation: A case report: J Med Case Rep, 2015; 9; 195
7.. Khan HH, Witkowski A, Clark JA, Mata A, A 17-year-old girl with a recent history of marijuana use presented with pneumomediastinum and pneumopericardium and tested positive for SARS-CoV-2 infection on hospital admission: Am J Case Rep, 2021; 22; e931800
8.. Weiss ZF, Gore S, Foderaro A, Pneumomediastinum in marijuana users: A retrospective review of 14 cases: BMJ Open Respir Res, 2019; 6(1); e000391
9.. Ramezani R, Jafari F, Fahami Y, A case report of pneumomediastinum and subcutaneous emphysema associated with pandemic COVID-19 in a 43-year-old man: Clin Imaging, 2021; 76; 74-76
10.. Mohan V, Tauseen RA, Spontaneous pneumomediastinum in COVID-19: BMJ Case Rep, 2020; 13; e236519
11.. Cavallari C, Ayoub B, Mateja C, Exercise-induced pneumomediastinum in a triathlete: Am J Respir Crit Care Med, 2021; 203; A1924
12.. Herrmann A, Herrmann M, Passlick B, Cycling-induced recurrent spontaneous pneumomediastinum and pneumopericardium in a young female patient: Clin Case Rep, 2022; 10(3); e05587
13.. Hogan F, McCullough C, An important differential in acute chest pain: BMJ Case Rep, 2014; 2014; bcr2014207692
14.. Clancy DJ, Lane AS, Flynn PW, Seppelt IM, Tension pneumomediastinum: A literal form of chest tightness: J Intensive Care Soc, 2017; 18(1); 52-56
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250