06 June 2023: Articles 
Unlocking Pain Relief for Chronic Low Back Pain: The Potential of the 4xT Method – A Dual Case Study Analysis
Unusual setting of medical care
Robbert N. van AmstelDOI: 10.12659/AJCR.939284
Am J Case Rep 2023; 24:e939284
Abstract
BACKGROUND: The 4xT method is a therapeutic approach involving 10 sequential steps. The 4xT method uses the steps test, trigger, tape, and train, sequentially executed until the patient can train with an acceptable level of pain. The report aimed to evaluate the effectiveness of 4xT therapy in managing chronic nonspecific low back pain (LBP) after the first treatment and after 6 weeks of therapy by measuring changes in range of motion (ROM) and pain levels using the numeric rating scale (pain NRS).
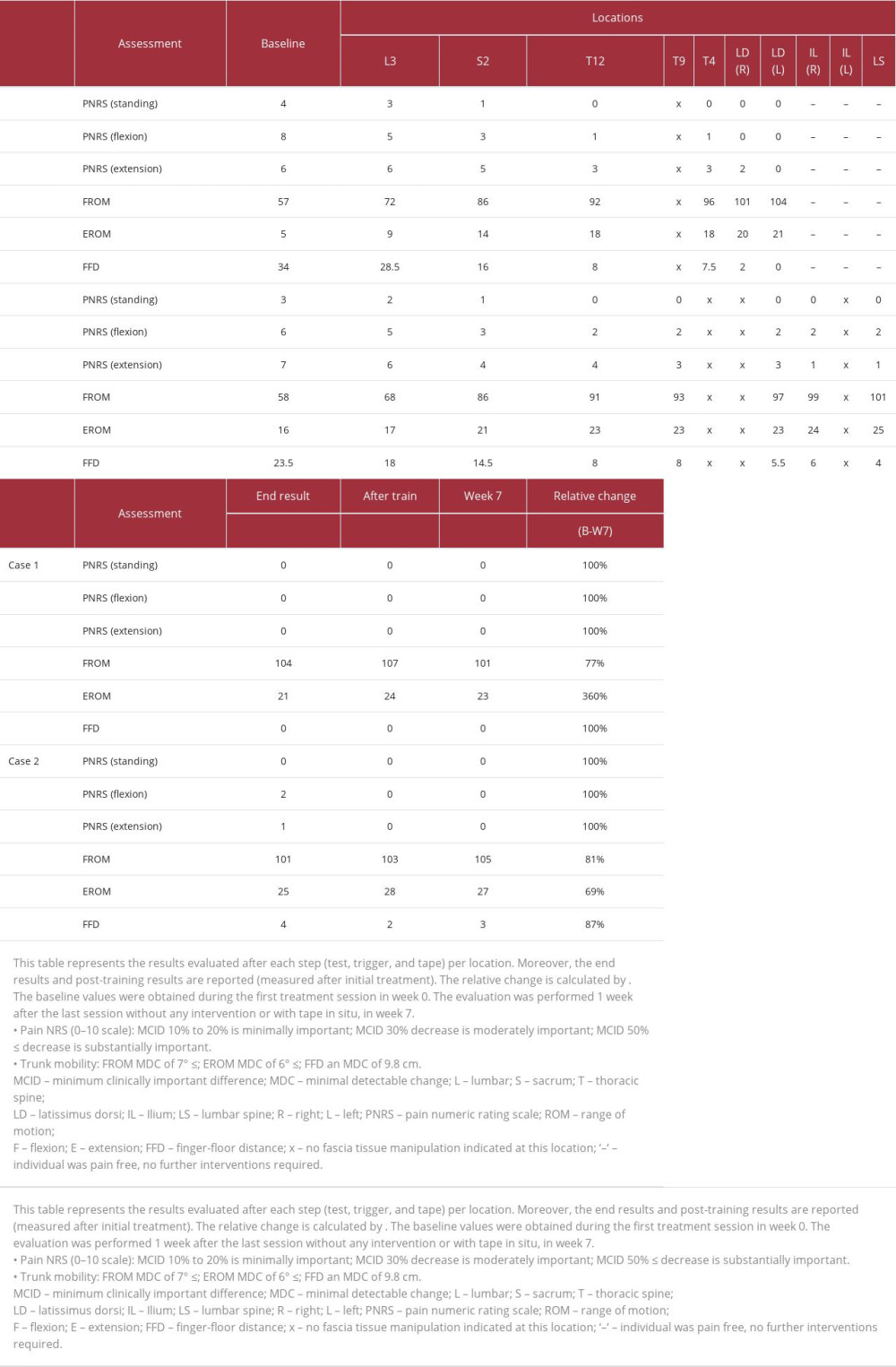
CASE REPORT: After the first treatment, patient 1 (42-year-old woman with 16 years of LBP, having a profession requiring standing) improved substantially in ROM, increasing flexion from 57° to 104° and extension from 5° to 21°. The pain NRS during flexion decreased from 8 to 0 (after step 6), and during extension, it decreased from 6 to 0 (after step 7). Similarly, patient 2 (43-year-old man with 13 weeks of LBP, having a sedentary occupation) showed ROM improvements, increasing extension from 16° to 25° and flexion from 58° to 101°. After step 8, pain NRS during extension decreased from 7 to 1, and during flexion, it decreased from 6 to 2 (after step 3). Pain further reduced to NRS0 after training. After 6 weeks of 4xT therapy, LBP improved, and mobility substantially increased in both patients.
CONCLUSIONS: The 4xT method was effective in reducing pain and improving mobility in 2 LBP patients after initial treatment and 6 weeks of therapy. Further research is necessary to validate these results in larger populations.
Keywords: Low Back Pain, Physical Therapy Modalities, Back Muscles, Range of Motion, Articular, Spine, Fascia, Male, Female, Humans, Adult, pain management
Background
RESEARCH DESIGN:
This case report is part of a randomized controlled trial that compared the effects of the 4xT method to exercise-only therapy during a 6-week period on trunk mobility, pain level, and quality of life. Two patients were randomly selected from the 4xT group to provide a detailed description of the effects of the 4xT method on pain and mobility per step (location and direction) [24]. The study was approved by the Committee of Medical Ethics at the University Hospital University of Brussels (B.U.N. 143201627110) and was prospectively registered (NCT03309540).
EVALUATION PROCEDURE:
The level of pain experienced was assessed in the standing position, end trunk flexion, and end trunk extension. The level of pain experienced was evaluated using the numeric rating scale (pain NRS) score (0 representing no pain, 10 representing the worst imaginable pain) [29]. A decrease in pain NRS score between 10% and 20% is considered minimally important, a 30% decrease is moderately important, and a decrease of 50% or more is substantially important [30].
The trunk ROM was measured for trunk flexion (FROM) and extension (EROM) with an inclinometer (model 10602, Fabrication Enterprise Inc, USA) and finger-floor distance (FFD) [31,32]. The FROM and EROM were assessed by placing the inclinometer at L1-T12, as described in the literature [31,33], and the FFD by measuring the distance between the patient’s right index finger and the floor using a standard measuring tape [34]. The trunk ROM was measured while the patients were barefoot and actively performing movements. To facilitate measurement, markings were made on the body with a dermatological pencil (S1-S2 and L1-T12) and labeled with strappal tape® (BSN Medical) (L1-T12). An inclinometer was used to measure the angle of trunk flexion and extension, and it was placed on the marked points with the tape between the inclinometer arcus and set to 0°. Before the first measurement, the patients were instructed to perform a knee-raising warm-up 10 times. They were then asked to stand upright with feet hip-width apart, arms straight alongside the body, thumbs forward, and forward gaze. During the test, the inclinometer was kept on L1-T12 as the investigator instructed the patients to bend forward with arms hanging. The distance between the right index finger and the floor was also measured from this position. Next, the patients were asked to put their hands on their pelvis and bend backward while the inclinometer remained on L1-T12. The FFD, EROM, and FROM were recorded by a ‘blinded’ operator who was masked to the patient allocation. The aim of the test was to provide an objective measurement of trunk mobility. This measurement method has been performed in several studies and has been found reliable [31,35].
The trunk ROM was measured 5 times with a 30-s rest period between each measurement. The mean of the 5 values was calculated. Research has shown no carry-over effects of the SKD when a 30-s break is taken between each test [23]. To minimize the measurement error, the minimum detectable change (MDC) for the inclinometer measurement and FFD was considered. The inclinometer FROM MDC90% of 7° and EROM MDC90% of 6° were taken into account [31], and the FFD MDC95% of 9.8 cm was taken into account [34].
The evaluation procedure was thoroughly explained to the patients to ensure their comprehension of how to accurately express their level of pain and perform trunk movements for precise trunk ROM measurement, following the standardized test method outlined by van Amstel et al [36]. The patients were evaluated by the same operator.
First, the patients performed the baseline trunk motions (flexion and extension) to retrieve the baseline pain NRS and trunk ROM values assessed by the operator. Based on the baseline data, the trunk motion that elicited the most pain was selected as the reference test, and the direction of motion that caused the least pain was identified as the directional preference [16]. To determine the positive direction for the trigger and tape application at the predetermined location (see § therapeutic intervention), the physiotherapist used the SKD at the specified location, while the patient performed the reference trunk motion. The pain NRS and trunk ROM values were evaluated after each step (test, trigger, and tape) per location up till the end (end results); moreover, the post-training results with tape in situ were documented (Table 1). The final results on pain NRS and trunk ROM were evaluated after a 6-week therapy period without intervention or tape in situ (Table 1).
Case Reports
PATIENT 1:
The case report concerns a 42-year-old female patient with a profession that required standing who had been experiencing LBP for over 16 years. The patient first developed acute LBP, which was resolved within 12 weeks, but the pain recurred twice a year. The pain was felt from her lumbar back up to her right upper leg, and the patient had received a diagnosis of lumbar disc herniation with right nerve entrapment at L4/5. Despite undergoing surgery (micro endoscopic discectomy) 14 years ago, the pain never completely went away. During pregnancy 6 years ago, the patient experienced no back problems, but LBP returned in the postpartum period. Four months after giving birth, the patient sprained her back while lifting her baby, which worsened her pain. Since then, the pain had been constant, although there had been episodes when it was less severe. A few times a year, the patient experienced severe LBP after spraining her back, which the patient could slightly alleviate with rest, heat, and walking. The patient’s most recent magnetic resonance imaging (MRI; T1: repetition time 600 ms, echo time 15 ms; T2: repetition time 3000 ms, echo time 100 ms) showed moderate lumbar disc degeneration and Modic changes (type 1), and physiotherapy was prescribed. However, the physiotherapy consisting of exercise therapy and massage did not improve her pain, physical functions, or disability. A year later, the patient sought treatment from a physiotherapy practice specialized in the 4xT method.
The patient presented to physiotherapy 2.5 years after the last MRI diagnosis, reporting pain in the paravertebral region with a tight sensation in her left hamstring. The pain level was rated as pain NRS4 for standing, pain NRS8 for maximal flexion, and pain NRS6 for the maximal extension. The trunk mobility measurements showed a FROM of 57°, an EROM of 5°, and an FFD of 34 cm (Table 1).
PATIENT 2:
The case report concerns a 43-year-old man with a sedentary occupation who had been experiencing LBP for the past 13 weeks. The patient had experienced LBP 3 years prior, which was resolved within 4 weeks. The current episode began during a prolonged meeting and started as moderate stiffness in his back. The next morning, the patient woke up with severe stiffness and pain in his back, which worsened during the day but improved with rest and heat. Over the following weeks, the intensity of the pain varied, but it did not subside. Five weeks later, the patient visited his family doctor, who prescribed paracetamol (200 mg) twice a day for 1 week, which temporarily eased the pain but did not resolve it. Two weeks after stopping the medication, the pain recurred and radiated to his right gluteal region. The patient visited his family doctor, who referred him to physiotherapy. The patient visited a physiotherapy practice specialized in the 4xT method 1 week later.
At the time of the initial assessment, the patient reported pain located at L3, which was more pronounced at the right quadratus lumborum and radiated to his right gluteus. The pain level was rated as pain NRS3 for standing, pain NRS6 for maximal flexion, and pain NRS7 for maximal extension. The trunk mobility measurements showed a FROM of 58°, an EROM of 16°, and an FFD of 23.5 cm (Table 1).
PHYSIOTHERAPIST TRAINING:
The 4xT back protocol was performed by a registered physiotherapist (BSc) [37] who had completed the comprehensive 4xT orthopedic rehabilitation for LBP course [24], which includes 24 h of practical training and 8 h of e-learning to equip participants with essential knowledge and skills for managing patients with LBP [38]. After completion of the 4xT program, the physiotherapist had obtained approximately 600 h of clinical experience with the 4xT method over the course of 1 year before the study was conducted.
THERAPEUTIC INTERVENTION:
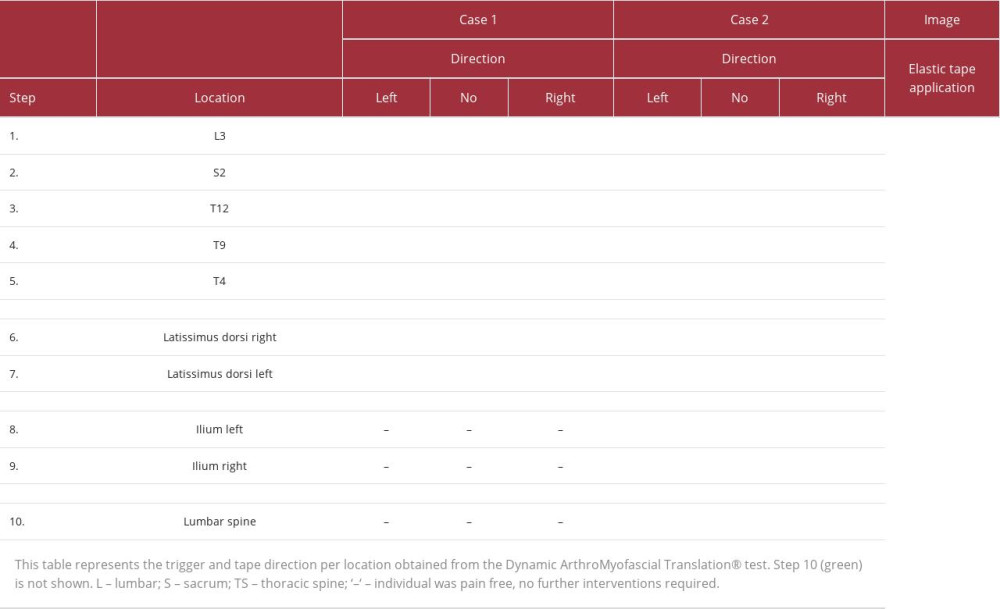
The intervention in this case report followed the test-trigger-tape-train algorithm: the intervention started with the DAMT-test (Figure 1) to determine the location and direction of the trigger and tape. The test, trigger, and tape steps were sequentially executed at the following locations: 1st L3, 2nd S2, 3rd T12, 4th T9, 5th T4, 6th thoracolumbar fascia/latissimus dorsi right, 7th thoracolumbar fascia/latissimus dorsi left, 8th ilium right, 9th ilium left, and finally, 10th step vertically over the lumbar spine till the patient was able to move with an acceptable pain level (pain NRS ≤2), required for rehabilitation exercise (train). To ensure clarity, we have provided a detailed explanation of the entire procedure below. While we have used L3 as an example, it is important to note that the same procedure applies to all locations.
TEST: The LBP patients started standing straight up. During the baseline test, maximal trunk flexion and maximal trunk extension movement were performed to retrieve the baseline values (pain NRS and ROM) (Figure 1(1)). The most painful trunk motion (highest pain NRS score) was selected as the reference test, and the direction causing the least pain was identified as the directional preference (lowest pain NRS score). The reference test was used to examine the effect of displacing the skin and underlying fasciae on both the pain NRS and ROM. The reference test with ongoing SKD was carried out, conforming to the 4xT back protocol [24]. The SKD consisted of (1) a mediolateral-directed lumbodorsal SKD to the right and left direction at the height of the spinal locations L3, S2, T12, T9, and T4 (Figures 1(2) and 2), subsequently, (2) diagonal cranial and caudal SKD above the latissimus dorsi muscle, (3) anterior and posterior SKD above the ilium, and (4) cranial and caudal SKD over the lumbar spine. The SKD intensity was beyond the skin and underlying fasciae slack (grade 4), equivalent to Maitland’s passive tissue stretch grading scale [39,40]. The SKD direction that led to the most significant improvement in terms of decreased pain NRS and increased trunk ROM was selected as the ‘positive’ direction and deemed the best trigger and tape direction at that time. It should be noted that when the reference test without SKD produced the most positive result on pain and/or trunk ROM, ‘no intervention’ was indicated at this location.
TRIGGER: At the targeted location, a cluster of triggers was applied in a standing position with slight flexion (approximately 60° [31]) and posterior pelvic tilt, while leaning forward on a physio plinth. The fascia and muscles were then released using the open fist and adduction technique (Figure 1(3)). Subsequently, spinal mobilization (grade 4) was performed to mobilize the spinal segment (eg, L3) in the directional preference and the positive SKD direction (eg, trunk flexion including right SKD L3=trunk extension including left L3 rotation mobilization). The medial aspect of the palm was placed at the arcus posterior, and the 5th phalange was positioned approximately at the process transverses L3 while the patient was standing. The physiotherapist assessed the spinal slack in the SKD direction and instructed the patient to take a deep breath, which was then held for 4 s. During exhalation, the joint was mobilized by moving the segment in the SKD direction, which was held for 4 s and repeated 4 times consecutively (Figure 1(4)). After the spinal mobilization, the elastic tape was applied in the positive mediolateral SKD direction at L3 while the patient was leaning forward on the physio plinth.
TAPE: The elastic tape was applied in the positive SKD direction with the fascia displacement technique utilizing approximately a 20-cm length of elastic tape (Easytape®, Msys BV) [24]. For example, at L3, the anchor (¼) of the elastic tape was stuck on the skin approximately 7 cm laterally of the spinous process L3 (Figure 3). The skin and underlying fasciae were then rubbed out simultaneously with the elastic tape (¾) with medium-high pressure in the contralateral direction (Figure 3), with the idea to align, displace, and place under tension the tissues underneath the tape in the direction of the SKD (Figure 1(5)) [24,41]. Subsequently, the reference test was retested with tape in situ in evaluating the FTMs effect. Then, the full procedure was executed at the next location (test, trigger, and tape) till the most painful trunk movement direction could be performed with an acceptable pain level needed for training.
TRAIN: The exercises were performed in the least painful ‘positive’ direction obtained from the baseline test (directional preference). The total training time was 30 min. The training schedule consisted of a 10-min warm-up session, followed by muscle endurance resistance training, muscle strength resistance training, flexibility training, and motor control exercises. The exercises were separated into 2 directional preference programs: (1) flexion direction program, which included recumbent bike, abdominal crunch machine, chess press machine, child pose Pilates position, and Pilates half rollback; or (2) extension direction program, which included cross-trainer, lower back extension machine, lat pull-down, puppy Pilates position, and Pilates-breaststroke exercise (in accordance with the 4xT back training protocol). The 4xT back training protocol focuses on isolating the lumbar multifidus and transverse abdominal muscles during muscle strength training, which are considered core muscles and are essential for trunk stability in all directions. To activate the core muscles during Pilates and machine exercises, anisometric-isotonic and anisometric-anisotonic contractions were performed by the patients, respectively. For muscle endurance resistance training, the patients performed 4 sets of 15 to 20 repetitions at a super-slow tempo (8 s for the concentric phase and 8 s for the eccentric phase) at an intensity of ≥50% 1RM. For muscle strength resistance training, the patients performed 4 sets of 8 to 12 repetitions with an eccentric emphasis at an intensity of 70% to 85% of 1RM (1 s for the concentric phase and 4 s for the eccentric phase) [42]. A rest period of 60 s was taken between sets, consistent with the recommendation by Schoenfeld et al [42].
PATIENT 1:
From the baseline data, trunk flexion was indicated as the reference test since it was scored with the highest pain score (pain NRS8) and trunk extension as the directional preference (pain NRS6).
In general, from the baseline until the end result, the FROM increased and flexion pain NRS decreased (Table 1). The greatest improvement in FROM and flexion pain NRS was found for the first step (L3, pain NRS= 37.5%; FROM 26.5%) and in FFD for the second step (43%). The pain NRS scores demonstrated a substantial reduction, decreasing from 8 to 0 during flexion (after step 6) and from 6 to 0 during extension (after step 7). The 100% reduction in pain NRS for both flexion and extension represents a meaningful improvement [30]. Based on the baseline to final result difference (Δ), the MDC90 was substantially achieved for all trunk ROM measurements (FROM 7° <Δ47°, EROM 6° <Δ16°, FFD 9.8 cm <Δ34 cm).
The positive direction obtained from the SKD varied per location (Table 2). At the mid-thoracic spine (T9) both SKD directions at the tested location had a negative effect on symptoms, and no intervention was indicated at this location (Table 2, step 4). After triggering and taping the fascia in the direction of the right latissimus dorsi (diagonal-cranial), the trunk flexion could be performed without any pain (pain NRS0). In a clinical setting, the test, trigger, and tape stop when the patient is able to move during the reference test with an acceptable pain level (pain NRS ≤2); although during evaluation, further treatment seemed to also reduce the extension pain and increase EROM, so the test was continued. After triggering and taping the left myofascia in the direction of the right latissimus dorsi (diagonal), the trunk extension could also be performed without any pain (pain NRS0). The total duration of this procedure from baseline to the final result was 12 min (excluding the measurement time). After the test, trigger, and tape, the patient followed an extension direction training program. The patient reported no pain during and after training. After the training, ROM showed a modest increase (Table 1). After this session, the 4xT back protocol was repeated in each session for 6 weeks. One week after the last physiotherapy session (week 7), the final results showed a substantial change in pain NRS and ROM measured without any intervention or with tape in situ (Table 1).
PATIENT 2:
From the baseline data, the extension trunk motion was indicated as the reference test since it was scored with the highest pain score (pain NRS7) and trunk flexion as the directional preference (pain NRS6).
In general, from the baseline to the final result the EROM increased, and extension pain NRS score decreased. The greatest improvement in EROM and extension pain NRS score was found for the second step (S2, pain NRS= 33.3%; EROM 35.3%).
During extension, the pain NRS score decreased from 7 to 1 after step 8, while during flexion, it decreased from 6 to 2 after step 3. Overall, a significant improvement in Pain NRS was observed for both flexion (86%) and extension (67%) at the end of the procedure, representing a substantial and meaningful change [30]. Based on the baseline-end result difference, the MDC was substantially achieved for all trunk ROM measurements (FROM 7° <Δ43°, EROM 6° <Δ9°, FFD 9.8 cm <Δ19.5 cm).
The positive direction obtained from the SKD varied per location (Table 2). At T9, left latissimus dorsi, and left ilium both SKD directions at the tested location had a negative effect on the pain, and no intervention was indicated at these locations (Table 2, steps 5,6,8). After triggering and taping the fascia of the right ilium, the trunk flexion and extension could be performed with an acceptable level of pain (pain NRS ≤2). Although, after evaluating the effectiveness of the following steps, the pain NRS score did not change; however, the trunk ROM showed a small increase. The total duration of this procedure from baseline to the final result was 16 min (excluding the measurement time). After the test, trigger, and tape steps, the patient followed a flexion direction training program. At the start of the training, the patient reported pain (pain NRS2), which subsequently decreased to zero (pain NRS 0) as the training progressed. After the training, a small improvement was found (Table 1). The 4xT back protocol was repeated in each subsequent session for 6 weeks. The final results, observed 1 week after the last session, revealed a significant improvement in both pain NRS and ROM measured without any intervention or with tape in situ (Table 1).
Discussion
The case report investigated the effectiveness of the 4xT method on pain and trunk ROM in 2 patients with chronic nonspecific LBP. Pain NRS and trunk ROM were evaluated after each step: test, trigger, and tape, which were sequentially executed until the patients could perform the movement with a pain NRS ≤2. Results showed that the 4xT method effectively reduced pain and improved trunk mobility in both patients within the initial treatment.
The reference test relied on the baseline test; however, both patients’ low difference between flexion and extension pain NRS score (≤2) was critical [29], as it raised concerns about the accuracy of determining the directional preference, potentially leading to incorrect treatment decisions and impacting therapy effectiveness. The patients’ preferred direction for triggers and tape application was determined by displacing the skin to another position during the reference test, as described in the DAMT-Test [24]. Van Amstel et al [24] found evidence that the used SKD in the DAMT-test can affect ROM in different regions of the body. The reported statistical significance and effect sizes demonstrate the magnitude of these effects, while the MDC95% values provide measures of precision for the change in ROM measurements [23]. The SKD of the DAMT-test is reported to have good intra- and inter-tester reliability [23]. More research is required to establish the practical value of the SKD of the DAMT-test in the diagnosing of or intervention for pain and joint mobility effects. Although this case report offers a starting point for investigating the potential applications of the DAMT-test, larger sample sizes and diverse populations are necessary to validate its usefulness.
Triggers were manually performed using myofascial release techniques and spinal mobilizations, which can manipulate and mobilize restricted connective tissues [42–44]. Tamartash et al [43–45] observed changes in tissue thickness and elasticity following lumbodorsal myofascial release, while Wong et al [46] found an increase in thoracolumbar fascia stress-strain and force output after myofascial release in healthy participants. Chen et al [47] reported improved transverse abdominal sliding mobility, and Arguisuelas et al [48] demonstrated a reduction in erector spinae myoelectric activity during trunk flexion in patients with chronic LBP. However, evidence supporting their effectiveness on disability, function, and pain is meager [19,20], and further research is needed to establish the effectiveness of myofascial release for LBP treatment. Spinal mobilizations can be performed in seated and standing positions [49–51], but evidence supporting their effectiveness is lacking [52,53]. More research is necessary to identify the most beneficial subgroups of patients and to understand the mechanisms of action of standing spinal mobilizations.
Tape is described to align and provide tension of the fascia underneath the elastic tape [41]. Wang et al [54] found that elastic tape application (100% of tension over erector spinae at the height from the sacrum to T12 vertebrae) increased the lumbodorsal fascia and paraspinal muscle stiffness underneath the tape, observed with MRI elastography. A common finding of elastic tape application (10% of tension over erector spinae at the height from the sacrum to T12 vertebrae) has been reported to decrease the thoracolumbar fascia strain (ultrasound) during spinal flexion in healthy individuals [55]. However, elastic tape application does not affect erector spinae muscle activity in healthy female participants [56] and patients with chronic LBP [57]. A systematic review reported that paraspinal lumbar elastic tape does not influence trunk mobility [58]. To the best of our knowledge, the tape application method described in this case report has not been previously studied, in contrast to other studies that have explored elastic tape application in various contexts [58]. Therefore, there is a lack of evidence on the effectiveness of this specific tape method. Further research is needed to determine whether this method is effective in improving pain and mobility in individuals with LBP.
The 2 directional preference training programs were based on current evidence in the management of LBP [16]. A systematic review found that training in the preferred direction can lead to improvements in pain and disability in patients with LBP [59]. Halliday et al [60] found that training in the preferred direction led to increases in abdominal muscle thickness and improved function, but was not more effective than motor control exercise. Regarding meta-analysis, training in the preferred direction is not superior to motor control exercises and other forms of exercise [61]. Multiple meta-analyses concluded that there is no superior training method for treating LBP [62,63]. As a result, guidelines [15,64] recommend including multiple forms of exercise in a comprehensive training program for patients with LBP. It should be investigated if training in the preferred direction is better after the patient was able to make the most painful movement with an acceptable pain level.
The current case report provided some evidence of the potential impact of the 4xT method; however, caution should be exercised in interpreting the results, owing to the small sample size (n=2). Further research is necessary to establish the validity of the underlying mechanisms following the DAMT-test and to determine the efficacy of this 4xT method in larger, high-quality clinical trials. If successful, optimizing the direction and location of FTMs could lead to the most significant impact important for patients. Overall, more extensive research is needed before any firm conclusions can be drawn regarding the clinical effectiveness of the 4xT method.
Conclusions
The results of the 4xT method in managing chronic nonspecific LBP may be promising. In both patients in this case report, improvements were seen in mobility and pain after the first treatment. Additionally, after 6 weeks of 4xT therapy, both patients experienced significant improvements in LBP and mobility. It is important to acknowledge that the study had a small sample size and lacked a control group, which limits the certainty of the effectiveness of this treatment approach. Moreover, we only reported short-term outcomes, and the long-term efficacy of this treatment approach is yet to be determined. Therefore, further research with larger sample sizes, control groups, and longer follow-up periods are necessary to validate the potential benefits of the 4xT method in managing chronic, nonspecific LBP.
Figures
References:
1.. Madan I, Grime PR, The management of musculoskeletal disorders in the workplace: Best Pract Res Clin Rheumatol, 2015; 29(3); 345-55
2.. Staal JB, Hendriks E, Heijmans M, KNGF Clinical Practice Guideline for Physical Therapy in patients with low back pain. KNGF-richtlijn [Internet] July, 2017 Available from: https://www.fysionet-evidencebased.nl/index.php/richtlijnen/
3.. Wilke J, Schleip R, Klingler W, Stecco C, The lumbodorsal fascia as a potential source of low back pain: A narrative review.: Biomed Res Int, 2017; 2017; 5349620
4.. Sinhorim L, Amorim MDS, Ortiz ME, Potential nociceptive role of the thoracolumbar fascia: A scope review involving in vivo and ex vivo studies: J Clin Med, 2021; 10(19); 4342
5.. Schilder A, Hoheisel U, Magerl W, Sensory findings after stimulation of the thoracolumbar fascia with hypertonic saline suggest its contribution to low back pain: Pain, 2014; 155(2); 222-31
6.. Huijing PA, Epimuscular myofascial force transmission: A historical review and implications for new research. International Society of Biomechanics Muybridge Award Lecture, Taipei, 2007.: J Biomech, 2009; 42(1); 9-21
7.. Maas H, Significance of epimuscular myofascial force transmission under passive muscle conditions: J Appl Physiol (1985), 2019; 126(5); 1465-73
8.. Widmer J, Fornaciari P, Senteler M, Kinematics of the spine under healthy and degenerative conditions: A systematic review: Ann Biomed Eng, 2019; 47(7); 1491-522
9.. Zügel M, Maganaris CN, Wilke J, Fascial tissue research in sports medicine: From molecules to tissue adaptation, injury and diagnostics: consensus statement: Br J Sports Med, 2018; 52(23); 1497-97
10.. Mawston GA, Boocock M, Lumbar posture biomechanics and its influence on the functional anatomy of the erector spinae and multifidus: Phys Ther Rev, 2015; 20(3); 178-86
11.. Sadler SG, Spink MJ, Ho A, Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies: BMC Musculoskelet Disord, 2017; 18(1); 179
12.. Stanton TR, Moseley GL, Wong AY, Kawchuk GN, Feeling stiffness in the back: A protective perceptual inference in chronic back pain: Sci Rep, 2017; 7(1); 9681
13.. Reis FJJ, Macedo AR, Influence of hamstring tightness in pelvic, lumbar and trunk range of motion in low back pain and asymptomatic volunteers during forward bending: Asian Spine J, 2015; 9(4); 535
14.. Rushton A, Beeton K, Jordaan R, International Federation Oforthopaedic Manipulative Physical Therapists (Ifompt) Inc, Part A: Educational Standards 2016 Available from: https://www.ifompt.org/site/ifompt/IFOMPT%20Standards%20Document%20definitive%202016.pdf
15.. Swart NM, Apeldoorn AT, Conijn D, KNGF Clinical Practice Guideline for Low back pain and lumbosacral radicular syndrome. KNGF-richtlijn [Internet] 2021 Available from: https://www.kngf.nl/kennisplatform/themas/Lage-rugpijn
16.. George SZ, Fritz JM, Silfies SP, Interventions for the management of acute and chronic low back pain: revision 2021: Clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American Physical Therapy Association: J Orthop Sports Phys Ther, 2021; 51(11); CPG1-CPG60
17.. Stecco C, Day JA, The fascial manipulation technique and its biomechanical model: A guide to the human fascial system.: Int J Ther Massage Bodywork, 2010; 3(1); 38-40
18.. Chaitow L, What’s in a name: Myofascial release or myofascial induction?: J Bodyw Mov Ther, 2017; 21(4); 749-51
19.. Chen Z, Wu J, Wang X, The effects of myofascial release technique for patients with low back pain: A systematic review and meta-analysis: Complement Ther Med, 2021; 59; 102737
20.. Wu Z, Wang Y, Ye X, Myofascial release for chronic low back pain: A systematic review and meta-analysis: Front Med (Lausanne), 2021; 8; 697986
21.. Luz Junior MAD, Almeida MO, Santos RS, Effectiveness of kinesio taping in patients with chronic nonspecific low back pain: A systematic review with meta-analysis: Spine (Phila Pa 1976), 2019; 44(1); 68-78
22.. Li Y, Yin Y, Jia G, Effects of kinesiotape on pain and disability in individuals with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials: Clin Rehabil, 2019; 33(4); 596-606
23.. van Amstel RN, Jaspers RT, Pool-Goudzwaard AL, Skin Displacement as fascia tissue manipulation at the lower back affects instantaneously the flexion-and extension spine, pelvis, and hip range of motion: Front Physiol, 2022; 13; 1067816
24.. Noten K December 3, 2021; 10-15 Available from: https://doi.org/10.17605/OSF.IO/D85K3
25.. Fysiotherapie FP: Fysio Physics Fysiotherapie;, 2020 [cited 2020]; Available from: https://www.fysiophysics.nl/de-4xtmethode/
26.. Chaudhry H, Schleip R, Ji Z, Three-dimensional mathematical model for deformation of human fasciae in manual therapy.: J Am Osteopath Assoc, 2008; 108(8); 379-90
27.. Chaudhry H, Bukiet B, Ji Z, Deformations experienced in the human skin, adipose tissue, and fascia in osteopathic manipulative medicine: J Am Osteopath Assoc, 2014; 114(10); 780-87
28.. de Campos TF, Low back pain and sciatica in over 16s: Assessment and management NICE Guideline [NG59]: J Physiother, 2017; 63(2); 120
29.. Ostelo RW, Deyo RA, Stratford P, Interpreting change scores for pain and functional status in low back pain: Towards international consensus regarding minimal important change: Spine, 2008; 33(1); 90-94
30.. Breivik H, Borchgrevink PC, Allen SM, Assessment of pain: Br J Anaesth, 2008; 101(1); 17-24
31.. Kolber MJ, Pizzini M, Robinson A: Int J Sports Phys Ther, 2013; 8(2); 129-37
32.. Perret C, Poiraudeau S, Fermanian J, Validity, reliability, and responsiveness of the fingertip-to-floor test: Arch Phys Med Rehabil, 2001; 82(11); 1566-70
33.. Sadeghi R, Mosallanezhad Z, Nodehi-Moghadam A, The reliability of bubble inclinometer and tape measure in determining lumbar spine range of motion in healthy individuals and patients: Physical Treatments, 2015; 5(3); 137-44
34.. Robinson HS, Mengshoel AM, Assessments of lumbar flexion range of motion: Intertester reliability and concurrent validity of 2 commonly used clinical tests: Spine, 2014; 39(4); E270-E75
35.. Salamh PA, Kolber M, The reliability, minimal detectable change and concurrent validity of a gravity-based bubble inclinometer and iphone application for measuring standing lumbar lordosis: Physiother Theory Pract, 2014; 30(1); 62-67
36.. van Amstel RN, Vaes P, Malone S, The measurable impact of a protocoled multimodal physiotherapeutic intervention on the quality of life in patients with non-specific chronic low back pain: A RCT study. Phys Ther Rehabil, 2018; 5(1); 2
37.. , De 4xT Therapeut register., 2022 Available from: https://4xt-therapeut.nl/register/
38.. , 4xT Orthopedic Rehabilitation for LBP. Available from: https://fysiotherapieopleiding.nl/shop/nascholing-fysiotherapie/rugpijn-orthopedische-revalidatie/
39.. Lee RY, Kinematics of rotational mobilisation of the lumbar spine.: Clin Biomech (Bristol, Avon), 2001; 16(6); 481-88
40.. Chester R, Swift L, Watson MJ, An evaluation of therapist’s ability to perform graded mobilization on a simulated spine: Physiother Theory Pract, 2003; 19(1); 23-34
41.. Kase K: Clinical therapeutic applications of the Kinesio (!R) taping method., 2008, Tokyo, Japan, Ken Ikai Co., Ltd
42.. Schoenfeld BJ, Peterson MD, Ogborn D, Effects of low- vs. high-load resistance training on muscle strength and hypertrophy in well-trained men.: J Strength Cond Res, 2015; 29(10); 2954-63
43.. Tamartash H, Bahrpeyma F, Dizaji MM, The effect of myofascial release techniques on lumbar fascia thickness and low back pain: J Mod Rehabil, 2022; 16(1); 244-51
44.. Tamartash H, Bahrpeyma F, Comparative effect of lumbar myofascial release with electrotherapy on the elastic modulus of lumbar fascia and pain in patients with non-specific low back pain: J Bodyw Mov Ther, 2022; 29; 174-79
45.. Tamartash H, Bahrpeyma F, Dizaji MM, Effect of remote myofascial release on lumbar elasticity and pain in patients with chronic nonspecific low back pain: A randomized clinical trial: J Chiropr Med, 2023; 22(1); 52-59
46.. Wong KK, Chai HM, Chen YJ, Mechanical deformation of posterior thoracolumbar fascia after myofascial release in healthy men: A study of dynamic ultrasound imaging: Musculoskelet Sci Pract, 2017; 27; 124-30
47.. Chen YH, Chai HM, Shau YW, Increased sliding of transverse abdominis during contraction after myofascial release in patients with chronic low back pain: Man Ther, 2016; 23; 69-75
48.. Arguisuelas MD, Lisón JF, Doménech-Fernández J, Effects of myofascial release in erector spinae myoelectric activity and lumbar spine kinematics in non-specific chronic low back pain: Randomized controlled trial: Clin Biomech (Bristol, Avon), 2019; 63; 27-33
49.. Wilson E, The Mulligan concept: NAGS, SNAGS and mobilizations with movement: J Bodyw Mov Ther, 2001; 2(5); 81-89
50.. Hussein HM, Morsi AA, Abdelraoof NA, The immediate effect of sustained natural apophyseal glide on postural stability and pain in individuals presenting with flexion-dominant chronic low back pain: A randomized single-blinded placebo-controlled trial: J Back Musculoskelet Rehabil, 2021; 34(6); 1079-86
51.. Kaltenborn FM, Evjenth O, Kalternborn TB: Manual mobilization of the joints; The Kaltenborn method of joint examination and treatment, 2003, Oslo, Norway, Norli
52.. Coulter ID, Crawford C, Hurwitz EL, Manipulation and mobilization for treating chronic low back pain: A systematic review and meta-analysis: Spine J, 2018; 18(5); 866-79
53.. Rubinstein SM, De Zoete A, Van Middelkoop M, Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: Systematic review and meta-analysis of randomised controlled trials: Br Med J, 2019; 364; 1-14
54.. Wang CK, Fang YD, Lin LC, Magnetic resonance elastography in the assessment of acute effects of kinesio taping on lumbar paraspinal muscles: J Magn Reson Imaging, 2019; 49(4); 1039-45
55.. Tu SJ, Woledge RC, Morrissey D, Does ‘Kinesio tape’ alter thoracolumbar fascia movement during lumbar flexion? An observational laboratory study: J Bodyw Mov Ther, 2016; 20(4); 898-905
56.. Ruggiero SA, Frost LR, Vallis LA, Brown SH, Effect of short-term application of kinesio tape on the flexion-relaxation phenomenon, trunk postural control and trunk repositioning in healthy females: J Sports Sci, 2016; 34(9); 862-70
57.. Grześkowiak M, Krawiecki Z, Łabędź W: J Sport Rehabil, 2019; 28(5); 402-12
58.. van Amstel RN, Noten K, van den Boomen LN, Systematic review of lumbar elastic tape on trunk mobility: A debatable issue: Arch Rehabil Res Clin Transl, 2021; 3(3); 100131
59.. Halliday MH, Garcia AN, Amorim AB, Treatment effect sizes of mechanical diagnosis and therapy for pain and disability in patients with low back pain: A systematic review: J Orthop Sports Phys Ther, 2019; 49(4); 219-29
60.. Halliday MH, Pappas E, Hancock MJ, A randomized controlled trial comparing the McKenzie method to motor control exercises in people with chronic low back pain and a directional preference: J Orthop Sports Phys Ther, 2016; 46(7); 514-22
61.. Lam OT, Strenger DM, Chan-Fee M, Effectiveness of the McKenzie method of mechanical diagnosis and therapy for treating low back pain: Literature review with meta-analysis: J Orthop Sports Phys Ther, 2018; 48(6); 476-90
62.. Owen PJ, Miller CT, Mundell NL, Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis: Br J Sports Med, 2020; 54(21); 1279-87
63.. Hayden JA, Ellis J, Ogilvie R, Some types of exercise are more effective than others in people with chronic low back pain: A network meta-analysis: J Physiother, 2021; 67(4); 252-62
64.. Liguori G: ACSM’s guidelines for exercise testing and prescription, 2020, Philadelphia, PA, USA, Wolters Kluwer Health
Figures
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250