18 March 2024: Articles 
Effective Management of Acute Oral Chemical Burns After NaOH Ingestion: A Case Report
Rare disease
Liu Bo Li1E*, Yu Hai Xia2B, Liang Ping2B, Mou Hai3C, Qiao Hong Tu4F, Dai Qing Yun1F, Yong Zhang1ADOI: 10.12659/AJCR.943134
Am J Case Rep 2024; 25:e943134
Abstract
BACKGROUND: Chemical burns in the oral cavity, although rare, cause more severe tissue damage than thermal burns, continuing tissue destruction even after removing the causative substance. Prompt identification of the substance, exposure extent, time from injury to treatment, and the injured area are imperative for effective management. This report details severe oral burns in an elderly woman from accidental NaOH ingestion.
CASE REPORT: A 70-year-old female patient was presented to our hospital approximately 15 h after inadvertent consumption of approximately 20 ml of NaOH (sodium hydroxide) solution. This incident led to oral discomfort and restricted mouth opening. The ingested solution, erroneously assumed to be a beverage, was later identified as a potent alkaline substance typically employed in grease removal. Initial manifestations included intense burning sensation, oral edema, and heightened salivation, which exacerbated on the following day, adversely impacting her alimentation and verbal communication. Clinical examination disclosed extensive damage to the oral mucosa. The diagnosis encompassed a chemical burn in the oral cavity coupled with chronic gastritis. The treatment regimen comprised dietary limitations, administration of famotidine for gastric acid suppression, intravenous hydration, nutritional support, oral care with Kangfuxin liquid, and nebulization therapy. Six months after therapy, she exhibited complete recovery, with the absence of discomfort and restored normal oral functions.
CONCLUSIONS: Timely and targeted treatment strategies, particularly nebulization medication and Kangfuxin liquid, are effective in managing chemical burns in the oral cavity, promoting wound healing, and preventing complications.
Keywords: treatment, Chemical Burns, Oral, NaOH, Sodium Hydroxide
Introduction
Chemical burns within the oral cavity are defined as localized injuries resulting from direct contact between various chemical substances and the oral mucosal tissue. These injurious agents can include potent acids, strong alkali, specific pharmaceuticals, or other toxic compounds, all of which can corrode and damage the oral tissues [1]. While there has been a notable decrease in accidental injuries in contemporary society, the prevalence of such injuries, particularly those stemming from inadvertent ingestion or improper use, remains a significant concern. For instance, a comprehensive study conducted in Germany between 1997 and 2014 recorded 482 instances of oral chemical burns, with a substantial 78% being attributed to accidental causes [2].
Substances of a caustic nature, such as sodium hydroxide (NaOH), are known to induce rapid and severe burn injuries as well as dissolution effects upon contact with biological tissues. The underlying pathophysiological mechanism involves disruption of cellular membranes, leading to compromised exchange of materials both within and outside the cells, resulting in cellular lysis and subsequent tissue necrosis [3]. Statistical data reveal that patients suffering from chemical burns represent approximately 1.4–10.7% of all hospitalized burn patients. Furthermore, fatalities arising from chemical burns constitute up to 30% of all deaths associated with burns [4]. Despite the extensive implementation of safety protocols, such incidents continue to occur, predominantly due to human error. These events not only cause significant physical harm but also impose severe psychological distress on the individuals affected.
This paper presents a case of oral burns caused by accidental ingestion of a caustic alkali solution, exploring the diagnostic, therapeutic processes, and subsequent management. Through this case, we aim to heighten the awareness of medical practitioners and the public regarding the hazards of chemical injuries and to reinforce preventative measures against such injuries. This study was reviewed and approved by the hospital’s Ethics Review Board and we obtained informed consent from the patient involved.
Case Report
On June 12, 2022, a 70-year-old woman was admitted to our hospital 15 h after accidental ingestion of an unidentified liquid, approximately 20 ml in volume. She reported oral pain and exhibited limited mouth opening. Her husband, who worked as a scavenger, had found a bottle containing the liquid (semi-transparent with minor white flocculent material) in a roadside trash bin, mistaking it for a beverage, and gave it to her. The patient ingested around 20 ml, immediately experiencing a burning sensation in her mouth. She spat it out reflexively, avoiding swallowing, and noticed oral swelling and stiffness, increased salivation, but only rinsed her mouth with water without seeking medical attention. The following morning, her symptoms intensified, affecting her ability to eat and communicate verbally, prompting her hospital visit. She denied experiencing fever, nausea, hematemesis, abdominal or chest pain, palpitations, or breathing difficulties. Her medical history was clear of cardiovascular diseases, diabetes, infectious diseases such as hepatitis, drug allergies, or mental health issues.
Upon specialist examination, she appeared conscious but distressed, with stable respiration and normal body temperature. Examination of the head, neck, and facial areas showed symmetry with no significant tenderness or abnormalities in the temporomandibular joints. Her mouth opening was limited to approximately 2.0 cm. The oral examination revealed widespread congestion, erosion, scattered submucosal hemorrhagic spots, and areas with yellow pseudomembranes on the inner aspects of the upper and lower lips, vestibular sulcus, gingiva, tongue, mouth floor, and palatopharyngeal mucosa, which were relatively soft. No active bleeding or significant tenderness was noted, and tongue movement was painful and restricted (Figure 1A, 1B). No enlarged lymph nodes were palpated in the submandibular or neck regions. She was admitted to the Gastroenterology Department for further evaluation and treatment for chronic gastritis; no corrosive injuries or stenosis in the esophagus were found. Blood tests indicated a significant inflammatory response (Table 1).
The unidentified liquid, upon pH testing, showed a pH of 14, identifying it as a strong alkali solution. It was later confirmed to be a NaOH solution, used by a nearby restaurant for grease removal and improperly disposed of in a beverage bottle.
Oral Pathology Biopsy: Biopsy from the patient’s lower-lip erosive area and submucosal glandular tissue showed mucosal erosion with shallow ulceration, infiltrated by inflammatory cells (Figure 2).
Final Diagnosis: 1. Chemical burn in the oral cavity; 2. Chronic gastritis.
Treatment: The patient received famotidine to inhibit gastric acid secretion, intravenous hydration, nutritional support, and topical Kangfuxin liquid for mucosal healing. Nebulization therapy with dexamethasone, gentamycin, vitamin C, and vitamin B12 was administered for anti-inflammatory and antibacterial purposes. Oral prednisolone acetate tablets and vitamin C were prescribed after autonomous water intake. Medication details are provided in Table 2. Significant improvement was noted in mouth opening and mucosal healing within 2 days of treatment (Figure 1C, 1D). By the third day, she had no discomfort and could eat and swallow normally (Figure 1E, 1F). Blood tests showed improved inflammatory markers, and she was discharged on the fourth day (Table 3).
Follow-up: Six months later, the patient reported no discomfort, with normal facial symmetry, temporomandibular joint function, mouth opening, oral vestibule, tongue movement, and mucosal conditions.
Discussion
The damage from chemical injuries persists until the causative substances are neutralized or metabolized. Current treatment principles for chemical burns emphasize immediate first aid at the site of injury, prompt removal of harmful substances, early interruption of chemical reactions to prevent further tissue damage and systemic entry, administration of specific antidotes, organ-protective measures, complication prevention, and timely surgical interventions when necessary [5,6]. In this case, the patient immediately spat out the ingested NaOH solution and did not swallow it. However, the delay in seeking medical care resulted in missed opportunities for optimal emergency treatment, leading to severe oral burns and extensive ulcerations. Laboratory investigations, including blood routine and pathological biopsies, indicated a marked inflammatory response. Alkali injuries, such as those from NaOH, are typically more severe than acidic injuries (eg, sulfuric or hydro-chloric acid) due to deeper tissue penetration [3,7]. NaOH not only affects the surface area of contact but also penetrates deeper tissues, causing more significant damage [8]. It disrupts the secondary and tertiary protein structures, leading to denaturation and cellular death [9], and can cause leakage of cellular contents through saponification reactions, triggering cell death [3].
Given the patient’s dietary restrictions, we opted for nebulization therapy with dexamethasone, gentamycin, vitamin C, and vitamin B12 injections to suppress inflammation and prevent bacterial infections. Nebulization therapy has been shown to effectively deliver medication in aerosolized form directly to oral ulcers, promoting healing [10]. This therapy reduces inflammation, improves oral mucosal tissue elasticity, and facilitates wound healing. Early corticosteroid use can alleviate symptoms such as redness, heat, and pain by reducing pore dilation, exudation, and edema, while its later use can suppress capillary and fibroblast proliferation, collagen and mucopolysaccharides synthesis, and granulation tissue growth, preventing adhesion and scar formation, and mitigating post-inflammatory complications [11–13].
Additionally, Kangfuxin liquid was prescribed for gargling. This liquid, derived from American cockroach extract, demonstrates notable anti-inflammatory properties, alleviating mucosal injury and promoting wound healing. A meta-analysis has demonstrated that the combination of Kangfuxin liquid with standard therapy significantly improve the total effective rate and cure rate for treating diabetic foot ulcers compared to standard therapy alone. Additionally, this combination has been shown to reduce healing time, without any significant adverse reactions [14]. Yuan et al [15] found that Kangfuxin liquid effectively prevents radiotherapy-induced oral mucositis in patients with head and neck squamous cell carcinoma. It reduces oral mucosal reactions and pain, improves salivary gland function, diminishes inflammatory responses, promotes cellular immune function, enhances quality of life, and improves the prognosis. In our clinical practice, we have frequently used Kangfuxin liquid for treating conditions such as oral ulcers and oral lichen planus, achieving favorable results.
In this case, the combined treatment mentioned above showed good results. On the second day of treatment, the patient’s oral pain and swelling were significantly alleviated, and the oral ulcer surface shrank.
This case underscores the importance of ensuring hazardous chemicals like sodium hydroxide are managed properly, emphasizing the need for specialized services to handle their safe treatment and neutralization, clear labeling on containers to prevent misuse or accidental ingestion, public education campaigns about the risks and correct disposal methods, strengthened enforcement of disposal regulations with established reporting systems for unsafe disposals, and collaboration between local communities and businesses to promote safe handling practices [16].
Conclusions
Timely and targeted treatment strategies, particularly nebulization medication and Kangfuxin liquid, are effective in managing chemical burns in the oral cavity, promoting wound healing, and preventing complications.
Figures
References:
1.. Sundararajan D, Noonan V, Gallagher G, Oral mucosal chemical burn: J Massa Dent Soc, 2017; 65(4); 31
2.. Nehrlich J, Klöcking HP, Hentschel H, Oral chemical burns reported to the Poisons Information Centre in Erfurt, Germany, from 1997 to 2014: J Burn Care Res, 2017; 38(6); e913-e22
3.. Hoffman RS, Burns MM, Gosselin S, Ingestion of caustic substances: N Engl J Med, 2020; 382(18); 1739-48
4.. Friedstat J, Brown DA, Levi B, Chemical, electrical, and radiation injuries: Clin Plast Surg, 2017; 44(3); 657-69
5.. Chai H, Chaudhari N, Kornhaber R, Chemical burn to the skin: A systematic review of first aid impacts on clinical outcomes: Burns, 2022; 48(7); 1527-43
6.. Walsh K, Hughes I, Dheansa B, Management of chemical burns: Br J Hosp Med (Lond), 2022; 83(3); 1-12
7.. Izadpanah A, Chemical burn: Diagnosis and treatments: Handbook of Burns, 2020; 1; 511-16
8.. Ahmadi Ashtiani HR, Noori Garmroodi AR, Hazrati E, A Review of management methods and modern treatments for chemical wounds: J Arch Mil Med, 2021; 9(1); e112029
9.. Atug O, Dobrucali A, Orlando RC, Critical pH Level of Lye (NaOH) for esophageal injury: Dig Dis Sci, 2009; 54(5); 980-87
10.. Oldoini G, Frabattista GR, Saragoni M, Ozone therapy for oral palatal ulcer in a leukaemic patient: Eur J Case Rep Intern Med, 2020; 7(2); 001406
11.. Rhen T, Cidlowski JA, Antiinflammatory action of glucocorticoids – new mechanisms for old drugs: N Engl J Med, 2005; 353(16); 1711-23
12.. Barnes PJ, How corticosteroids control inflammation: Quintiles Prize Lecture 2005: Br J Pharmacol, 2006; 148(3); 245-54
13.. Coutinho AE, Chapman KE, The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights: Mol Cell Endocrinol, 2011; 335(1); 2-13
14.. Qu KS, Li Y, Liang Y, KangFuXin liquid in the treatment of diabetic foot ulcer: A systematic review and meta-analysis: Evid Based Complement Alternat Med, 2019; 2019; 3678714
15.. Yuan H, Su J, Tan J, Efficacy of kangfuxin liquid on radiotherapy-induced oral mucositis for patients with head and neck squamous cell carcinoma and its effect on salivary glands and immune function: Am J Transl Res, 2022; 14(9); 6792-804
16.. Wang C, Wang X, Chen M, Status quo of laboratory chemical waste disposal and improvement strategy: Univ Chem, 2023; 38(8); 268-74
Figures
Tables
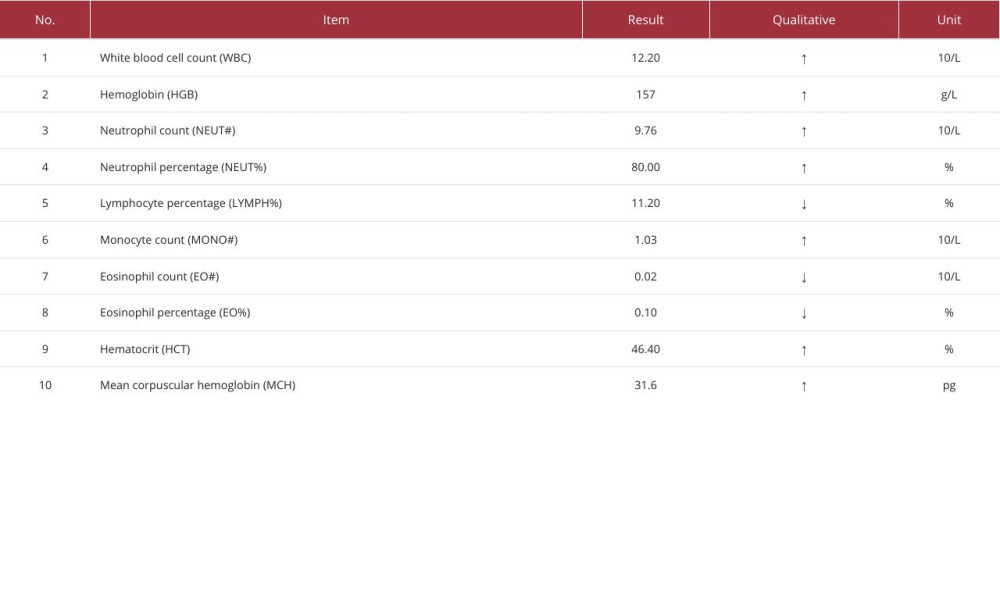 Table 1.. Results of complete blood count test.
Table 1.. Results of complete blood count test. Table 2.. Patient medication information.
Table 2.. Patient medication information.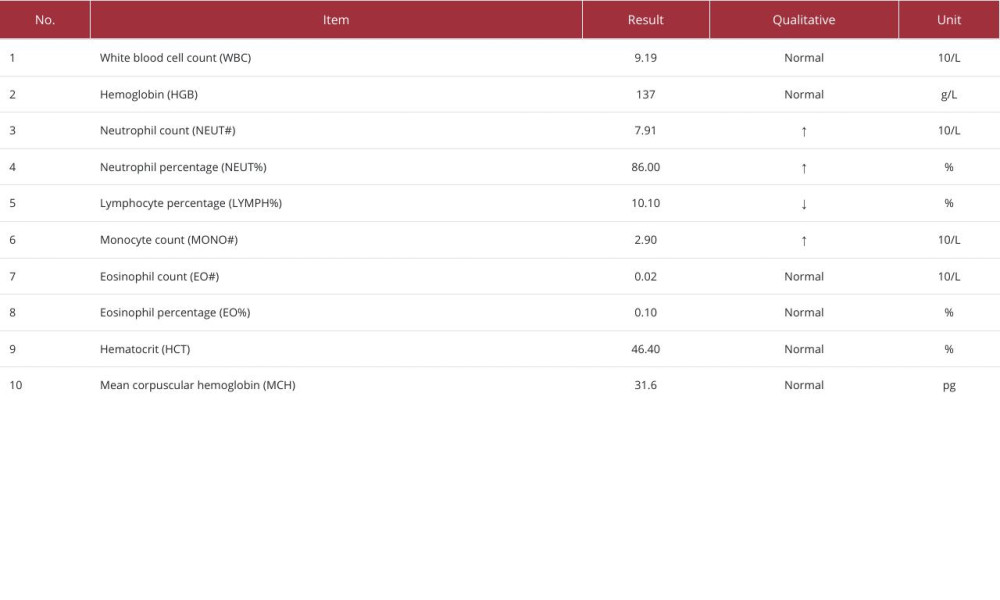 Table 3.. Results of complete blood count test on the third day of treatment.
Table 3.. Results of complete blood count test on the third day of treatment.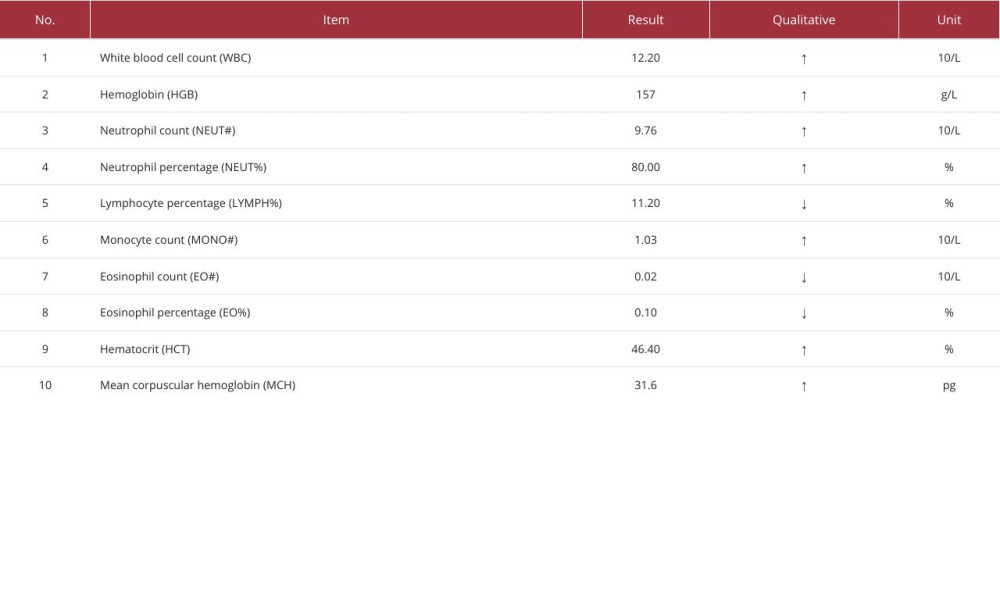 Table 1.. Results of complete blood count test.
Table 1.. Results of complete blood count test. Table 2.. Patient medication information.
Table 2.. Patient medication information.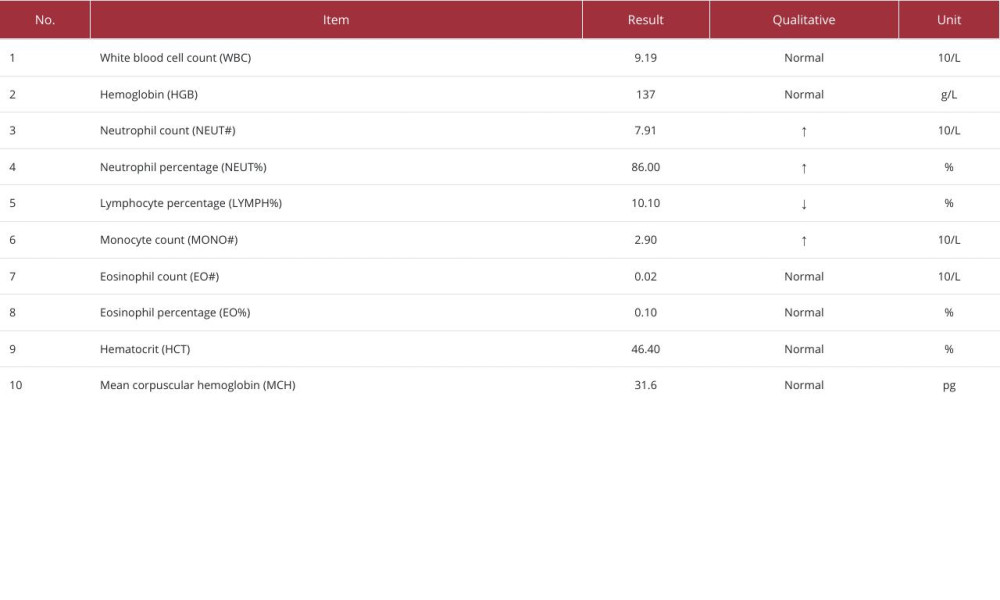 Table 3.. Results of complete blood count test on the third day of treatment.
Table 3.. Results of complete blood count test on the third day of treatment. In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








