27 May 2022: Articles 
Postoperative Serotonin Syndrome Following Administration of Preoperative Intrapulmonary Methylene Blue and Intraoperative Granisetron: A Case Report
Unusual clinical course, Unexpected drug reaction
Wei-Hsiu Huang1EF, Min-Jia Li1EF*DOI: 10.12659/AJCR.936317
Am J Case Rep 2022; 23:e936317
Abstract
BACKGROUND: Methylene blue (MB), which is often used perioperatively, is a potent monoamine oxidase inhibitor that can strongly block the clearance of extracellular serotonin. Granisetron, a serotonin receptor subtype 3 (5-HT3) antagonist, is an antiemetic used to prevent or treat postoperative nausea and vomiting (PONV). Through its antagonism, granisetron can increase the extracellular serotonin concentration. Serotonin syndrome is a potentially life-threatening condition resulting from a drug reaction that affects serotonin levels. This report is of a 50-year-old woman with postoperative serotonin syndrome following co-administration of preoperative intrapulmonary methylene blue and intraoperative granisetron.
CASE REPORT: A 50-year-old woman with well-controlled gastroesophageal regurgitation disease presented under impression of lung cancer. She received a computed tomography (CT)-guided localization followed by video-assisted thoracic surgery under endotracheal general anesthesia. The surgery was completed uneventfully. Her postoperative course was significant for serotonin syndrome, likely triggered by co-administration of preoperative intrapulmonary MB for tumor localization and intraoperative granisetron. Other differential diagnoses were ruled out. Her management was primarily supportive, using benzodiazepine administration, and resulted in full neurologic recovery.
CONCLUSIONS: Intrapulmonary MB can lead to serotonin syndrome in combination with 5HT-3 antagonists when used for preoperative tumor localization. Because both MB and 5-HT3 antagonists are being widely used clinically at present, this report has highlighted that physicians, surgeons, and anesthesiologists should be aware of serotonin syndrome, its presenting features, and management, and its association with the use of methylene blue and 5-HT3 receptor antagonists, including granisetron.
Keywords: Methylene Blue, Drug Interactions, Serotonin Syndrome, Granisetron, Female, Granisetron, Humans, Middle Aged, Neoplasms, Serotonin
Background
Serotonin syndrome, also known as serotonin toxicity, is a potentially life-threatening condition that results from inappropriately high levels of synaptic serotonin. The serotonergic hyperactivity can be precipitated by blocking its extracellular clearance or by increasing its release from serotonergic neurons [1]. Serotonin toxicity has a wide spectrum of clinical features, such as autonomic signs, neuromuscular changes, and altered mental status [2]. Patients with serotonin syndrome may develop minor symptoms such as tachycardia, shivering, diaphoresis, inducible clonus, or agitation. Under severe conditions, fatal symptoms such as unstable hemodynamics, hyperthermia, sustained clonus, and muscle rigidity can occur. The Hunter serotonin toxicity criteria are mostly used to confirm a diagnosis of serotonin syndrome owing to its simplicity, high sensitivity (84%), and high specificity (97%) [2]. Once serotonin toxicity is diagnosed, physicians must remove the precipitating drugs as soon as possible. Serotonin syndrome is not believed to resolve spontaneously without discontinuing the precipitating agents. Other therapies should also be initiated based on the severity of toxicity. Patients with mild manifestations can usually be managed with supportive care and benzodiazepines. Moderate and severe cases, with unstable hemodynamics, should be aggressively corrected and may benefit from the administration of serotonin receptor subtype 2a (5-HT2a) antagonists. Severely ill patients, whose temperature is higher than 41.1°C or with rapidly deteriorating conditions, should receive aggressive therapies as well as neuro-muscular paralysis and orotracheal intubation [3].
Methylene blue (methylthioninium chloride, MB), which is often used perioperatively for diagnostic purposes, is a potent monoamine oxidase inhibitor (MAOI) that can strongly block the clearance of extracellular serotonin. Use of MB in combination with a variety of medications with serotonergic activity, including selective serotonin reuptake inhibitors [1,4,5], serotonin norepinephrine reuptake inhibitors [6], opiate analgesics [4], and antiemetics [5], can contribute to serotonin toxicity. Owing to the risk of this central nervous system reaction, the United States Food and Drug Administration published a Drug Safety Communication in 2011, which advised that MB should generally not be administered to patients on serotonergic drugs [7]. Although several studies showed that intravenous MB can cause severe serotonin syndrome when used in conjunction with serotonergic agents [1,5,6], no case report has mentioned the risk of MB when used in tumor localization. There also have been few reports on the development of serotonin syndrome after administration of serotonin receptor subtype 3 (5-HT3) antagonist, although it is an uncommon but potentially life-threatening adverse effect. 5-HT3 receptor antagonists, including granisetron, ondansetron, and palonosetron, are commonly used perioperatively for treatment or prevention of postoperative nausea and vomiting (PONV) and in patients undergoing cancer treatment. They work on the neural pathways involved with vomiting by blocking serotonin from entering nerve cells. It is unlikely that even high doses of 5-HT3 antagonist, alone, would cause severe serotonin toxicity [8,9]. However, previous reports showed that when used concomitantly with other serotonergic medicines, 5-HT3 antagonists could be linked with a potential risk of serotonin syndrome [5,8–11]. In 2012, the World Health Organization (WHO) concluded that 5-HT3 antagonists can contribute to the development of serotonin syndrome in susceptible patients who are concomitantly receiving other drugs affecting the serotonin system [12]. Here, we report the case of a 50-year-old woman with postoperative serotonin syndrome following administration of preoperative intrapulmonary methylene blue and intraoperative granisetron.
Case Report
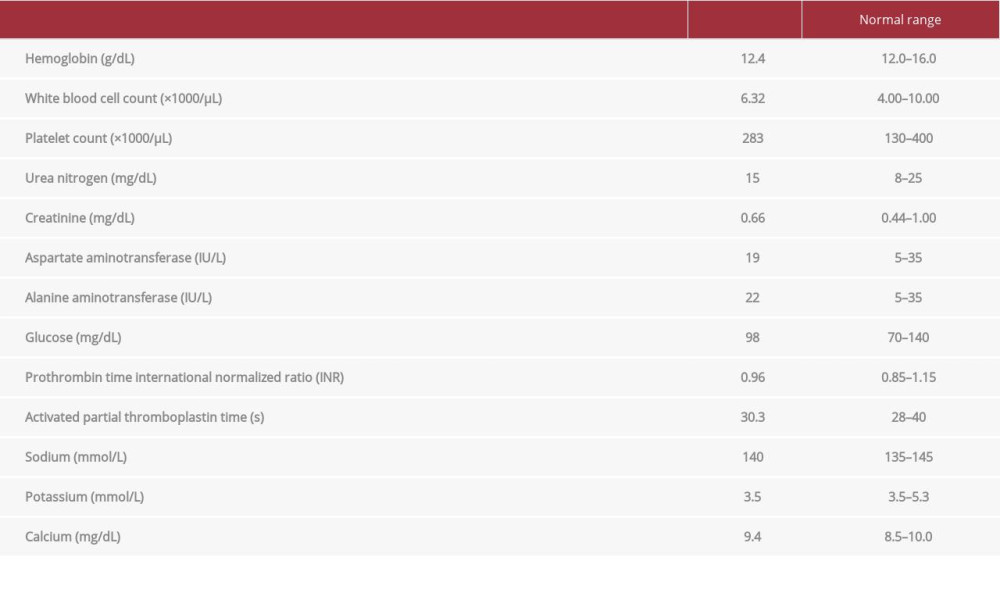
A 50-year-old, 46-kg, American Society of Anesthesiologists physical status 2, Asian woman with a history of well-controlled gastroesophageal reflux disease presented to our hospital. She denied any medication history on admission. Her surgical history was remarkable for cesarean section decades earlier. This time, she was admitted for computed tomography (CT)-guided localization followed by video-assisted thoracic surgery under endotracheal general anesthesia under the diagnosis of adenocarcinoma in situ or minimally invasive adenocarcinoma. According to her statement, CT imaging conducted in a previous routine health examination had incidentally revealed multiple small ground-glass opacites in the bilateral lungs. She had no respiratory or systemic symptoms. After admission, preoperative evaluations were completed. Her baseline vital signs data were body temperature 36.3°C, heart rate 79 beats per minute, and blood pressure 134/57 mmHg. A chest radiograph and electrocardiograph showed no abnormalities. Subsequently, she underwent abdominal sonography, abdominal magnetic resonance imaging, echocardiography, positron emission tomography, and whole-body bone scanning, which revealed no remarkable findings. Her laboratory data, shown in Table 1, were within the normal range.
On the day of surgery, she underwent CT-guided localization with approximately 50 mg of intrapulmonary MB, after which she was transferred to the operating room. Upon arrival, monitors were placed, including the bispectral index (BIS) monitor, along with arterial and peripheral lines. Her vital signs were temperature 37.2°C, heart rate 82 beats per minute, and blood pressure 132/85 mmHg. After preoxygenation, general anesthesia was induced with 110 mg of propofol, 150 μg of fentanyl, 30 mg of rocuronium, and 5 mg of dexamethasone. After adequate anesthesia was ensured, the patient was intubated with a cuffed endotracheal tube with an internal diameter of 8 mm and a blocker. Lung isolation was performed through the bronchial blockage of the right bronchus while the surgery was performed. Desflurane and dexmedetomidine infusion (0.65 mcg/kg/h) were used to maintain anesthesia and the BIS value was in the range of 40–60. Intermittent bolus rocuronium was administered according to the value of train-of-four monitor. Continuous epidural 1% lidocaine infusion was used for pain management. The surgery was completed un-eventfully within 3 h. At the end of surgery, 1 mg of granisetron was intravenously administered as prophylaxis for PONV. The patient was awakened 30 min later and then transferred to the postanesthesia care unit (PACU) with smooth spontaneous respiration. In the PACU, the patient was agitated, confused, and restless. Her vital signs were all stable, with blood pressure between 125/80 mmHg and 139/80 mmHg, heart rate around 90 beats per minute, and body temperature around 37.6°C. Nevertheless, she failed to cooperate with any physical examination. She was administered midazolam 2 mg for sedation, which relieved her agitation after 20 min. However, she was still disoriented, with ocular clonus. Subsequently, a diagnosis of serotonin toxicity was established according to the Hunter serotonin toxicity criteria [2]. Because the clinical symptoms improved over time, the patient was kept under observation. After approximately 1.5 h of her arrival at the PACU, she became orientated and regained the ability to talk to her family. Subsequently, under stable vital signs and clear consciousness, she was transferred back to the general ward. The postoperative course at the general ward was smooth, without any altered mental status. She recovered from a surgical standpoint and was discharged home 6 days after the operation.
Discussion
This case report revealed that preoperative intrapulmonary MB for tumor localization can lead to serotonin syndrome in combination with 5HT-3 antagonists. The case report also showed that postoperative serotonin syndrome is easily mis-diagnosed or underdiagnosed due to its variable presentation. As a case report of drug interaction, the authors used the Drug Interaction Probability Scale (DIPS) (Table 2) [13] to evaluate our patient. Previous studies showed that MB and granisetron both can contribute to increased serum serotonin concentration (answers to the question 2 and 3 below), and there are several credible case reports provided evidence supporting the drug interaction between MB and 5-HT3 antagonists (answer to the question 1 below). In our scenario, serotonin toxicity was diagnosed according to the Hunter serotonin toxicity criteria (answer to the question 9 below). The estimated terminal half-life of MB after administration is 5.25 h [14], and the time course of the change in MB concentrations was consistent with a change in its elimination (answer to question 4 below). The patient received fentanyl only at the beginning of the operation. There was no known serotonergic agent or serotonin clearance blocking agent other than MB and granisetron administrated (answer to the question 7, below). Therefore, we achieved 6 out of 10 points, suggesting a probable causation between the drug interaction and the event of serotonin toxicity [13].
Serotonin syndrome is a potentially lethal condition that manifests with many clinical signs. Owing to its variable symptoms, this condition is often misdiagnosed, especially when it occurs postoperatively [15]. van Ewijk reported that awareness of potential serotonin toxicity is low among physicians [8]. Detecting the signs of serotonin syndrome postoperatively is difficult in patients undergoing general anesthesia. For example, agitation and confusion may be interpreted as delirium, and elevated temperature may be misdiagnosed as malignant hyperthermia. Furthermore, anesthetics, such as benzodiazepines and muscle relaxants, can mask symptoms. Therefore, early identification of patients at risk for serotonin syndrome is crucial and will likely determine the patient’s perioperative outcome.
In our clinical scenario, a definitive diagnosis was delayed until the ocular clonus was noted. Supportive care consisting of hydration and benzodiazepines was initiated and resulted in full neurologic recovery. Neuroleptic malignant syndrome and anticholinergic syndrome were considered less likely due to the lack of administration of a dopamine antagonist and anticholinergic agent. Malignant hyperthermia was also deemed unlikely because of the absence of fever, increasing concentrations of end-tidal carbon dioxide, or metabolic acidosis.
In this case report, our patient was given intrapulmonary MB rather than intravenous MB. The development of toxicity indicates that MB can be absorbed during the tumor localization. MB, as an indicator dye, is often used to confirm the location of the parathyroid gland, to delineate the lymph node and lymphatic vessels, and to localize tumors. Currently, MB is commonly used in the preoperative CT-guided localization of malignant pulmonary nodules smaller than 1 cm in diameter. Moreover, MB acts as a potent reversible MAOI. Thus, use of MB in combination with other serotonergic agents can lead to serotonin toxicity [16]. Previous studies have only reported that the concomitant use of intravenous MB and serotonergic agents can be fatal [1,6]. No study has reported on the accurate systemic concentration of MB in patients undergoing intrapulmonary tumor localization. We did not measure the plasma levels of MB in our patient. However, human data have shown that an intravenous dose of only 0.75 mg/kg of MB produced a peak plasma concentration of 500 ng/mL in the central nervous system, which could inhibit MAO A [17]. This indicates that even a small amount of systemic absorption of MB during localization can lead to MAO inhibition. Serotonin syndrome was reported in a patient undergoing urological surgery who had received a low concentration of MB to assess for ureteral patency [4]. Our case report confirmed that MB injected into the lung can also lead to serotonin toxicity.
5-HT3 antagonists, such as ondansetron, granisetron, and palonosetron, are commonly used to prevent or treat PONV. Through their antagonism, 5-HT3 antagonists can increase the extracellular serotonin concentration. 5-HT levels need to be increased by 40-fold over baseline to induce relevant toxicity; thus, 5-HT3 antagonists usually do not play a major role in inducing serotonin syndrome [8,9]. However, some factors can affect patients’ susceptibility to developing significant serotonergic toxicity, including illness severity [10], blood–brain barrier disturbances, and cytochrome P450 polymorphisms [11]. In 2001, Turkel et al reported the occurrence of serotonin syndrome in 2 severely ill children who received ondansetron in combination with other serotonin reuptake blocking agents [10]. Stanford et al demonstrated that interactions between ondansetron and paroxetine increase vulnerability to serotonin toxicity [1,5]. With the increasing number of cases published in the literature and reported in the database, the WHO concluded in 2012 that an association between 5-HT3 antagonists and serotonin syndrome should be considered in susceptible patients [12]. In our case scenario, the patient was not critically ill. Without any central nervous systemic dysfunction such as epilepsy, neuropsychiatric disorders, or cognitive decline, she did not seem to have blood–brain barrier disturbance either. Whether our patient had cytochrome P450 polymorphisms was not checked, and it is impractical to test the patient before administering 5-HT3 antagonists. In this case report, we could not determine the origin of the patient’s susceptibility to granisetron. Instead, this case report highlighted the importance of close monitoring perioperatively in every patient who receives 5-HT3 antagonists, especially those concomitantly receiving any antidepressants or MAOI.
Conclusions
Both MB and 5-HT3 antagonists are being widely used clinically at present. Intrapulmonary MB can lead to serotonin syndrome in combination with 5HT-3 antagonists when used for preoperative tumor localization. Careful vigilance is of utmost importance to prevent iatrogenic morbidity and mortality associated with this drug interaction. This report has highlighted that physicians, surgeons, and anesthesiologists should be aware of serotonin syndrome, its presenting features, and management, and its association with the use of methylene blue and 5-HT3 receptor antagonists, including granisetron.
References:
1.. Stanford SC, Stanford BJ, Gillman PK, Risk of severe serotonin toxicity following co-administration of methylene blue and serotonin reuptake inhibitors: An update on a case report of post-operative delirium: J Psychopharmacol, 2010; 24(10); 1433-38
2.. Dunkley EJ, Isbister GK, Sibbritt D, The Hunter Serotonin Toxicity Criteria: Simple and accurate diagnostic decision rules for serotonin toxicity: QJM, 2003; 96(9); 635-42
3.. Boyer EW, Shannon M, The serotonin syndrome: N Engl J Med, 2005; 352(11); 1112-20
4.. Francescangeli J, Vaida S, Bonavia AS, Perioperative diagnosis and treatment of serotonin syndrome following administration of methylene blue: Am J Case Rep, 2016; 17; 347-51
5.. Stanford BJ, Stanford SC, Postoperative delirium indicating an adverse drug interaction involving the selective serotonin reuptake inhibitor, paroxetine: J Psychopharmacol, 1999; 13(3); 313-17
6.. Top WM, Gillman PK, de Langen CJ, Kooy A, Fatal methylene blue associated serotonin toxicity: Neth J Med, 2014; 72(3); 179-81
7.. : FDA Drug Safety Communication: Serious CNS reactions possible when methylene blue is given to patients taking certain psychiatric medications, U.S. Food and Drug Administration website
8.. van Ewijk CE, Jacobs GE, Girbes ARJ, Unsuspected serotonin toxicity in the ICU: Ann Intensive Care, 2016; 6(1); 85
9.. Gillman PK, A review of serotonin toxicity data: Implications for the mechanisms of antidepressant drug action: Biol Psychiatry, 2006; 59(11); 1046-51
10.. Turkel SB, Nadala JG, Wincor MZ, Possible serotonin syndrome in association with 5-HT(3) antagonist agents: Psychosomatics, 2001; 42; 258-60
11.. Beatty NC, Nicholson WT, Langman LJ, Pharmacogenetic workup of perioperative serotonin syndrome: J Clin Anesth, 2013; 25(8); 662-65
12.. : WHO pharmaceuticals newsletter, 2012; 3; 16-21, Sweden, World Health Organization
13.. Horn JR, Hansten PD, Chan LN, Proposal for a new tool to evaluate drug interaction cases: Ann Pharmacother, 2007; 41(4); 674-80
14.. Peter C, Hongwan D, Küpfer A, Lauterburg BH, Pharmacokinetics and organ distribution of intravenous and oral methylene blue: Eur J Clin Pharmacol, 2000; 56(3); 247-50
15.. Isbister GK, Buckley NA, Whyte IM, Serotonin toxicity: A practical approach to diagnosis and treatment: Med J Aust, 2007; 187(6); 361-65
16.. Ramsay RR, Dunford C, Gillman PK, Methylene blue and serotonin toxicity: Inhibition of monoamine oxidase A (MAO A) confirms a theoretical prediction: Br J Pharmacol, 2007; 152(6); 946-51
17.. Gillman PK, CNS toxicity involving methylene blue: The exemplar for understanding and predicting drug interactions that precipitate serotonin toxicity: J Psychopharmacol, 2011; 25(3); 429-36
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250









![Drug Interaction Probability Scale [16].](https://jours.isi-science.com/imageXml.php?i=t2-amjcaserep-23-e936317.jpg&idArt=936317&w=1000)